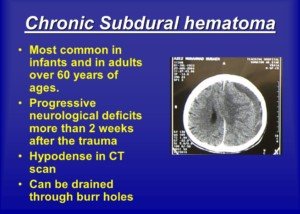
Chronic Subdural Hematoma Symptoms: Young vs. Old Patients
Yes, there tends to be differences in symptoms of chronic subdural hematoma in young patients vs. elderly.
A report in the journal Injury points out differences in symptom presentation of chronic subdural hematoma in young patients (under age 40) and elderly (over age 75).
Young Patients with Chronic Subdural Hematoma
The researchers observed particular characteristics of symptoms: a higher incidence of headache, and a higher incidence of vomiting, along with a shorter time span between initial trauma and corrective surgery.
Elderly Patients
They tended to have symptoms relating to change in mental status, deficits in motor control and larger collections of blood in the brain.
Pertaining to the patients in this analysis, there was no statistically significant difference in the rate of surgical complications.
Just what is a chronic subdural hematoma?
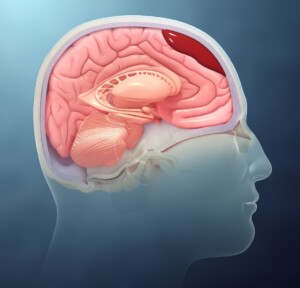
Depiction of a subdural hematoma. Scientific Animations, CC/BY-SA/Attribution-ShareAlike 4.0 International
A chronic subdural hematoma is a type of brain injury where blood collects between the brain’s surface and the dura mater, the outermost layer of the protective coverings of the brain.
It’s significantly more common in people over 65 vs. middle age and especially younger adults.
Unlike an acute subdural hematoma, which occurs suddenly due to trauma and involves rapid bleeding, a chronic subdural hematoma develops over weeks or months.
This slower progression happens when small veins between the brain and the dura mater are torn, often due to minor head trauma or even spontaneously, particularly in individuals with weakened blood vessels or elderly people on blood thinners.
Brain shrinkage due to age is the primary reason people over 65 are much more likely to suffer from a chronic subdural hematoma.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/wavebreakmedia
Source: injuryjournal.com/article/S0020-1383(02)00020-7/abstract
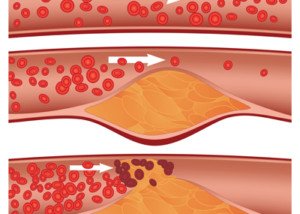
Soft Plaque Rupture, Chest Pain, Low Heart Disease Risk?

Can chest pain in a physically fit person with low heart disease risk be caused by a soft plaque rupture?
“Recent literature suggests two different kinds of plaque: calcified plaque which is considered more stable and less likely to rupture; and soft plaque which is considered to be more lipid-laden and more likely to rupture,” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
The coronary calcium score test measures only the calcified plaque, and the amount is converted to a numerical value.
There is a strong correlation between numerical value and likelihood of heart disease and near-future cardiac events.
However, in a person with a low or zero calcium score, or, to put another way, very little “sludge” in their coronary arteries, it’s not impossible for them to experience a soft plaque rupture.
After all, the soft plaque in a fit, nonsmoking athlete with a healthy lifestyle is just as “unstable” as the soft plaque in a sedentary, diabetic, junk-food eating person with high blood pressure.
The classic cause of cardiac chest pain other than heart attack is a condition called angina.
This is when blood flow in the coronary artery is temporarily restricted, causing chest pain (and sometimes shortness of breath).
Usually there’s a trigger, namely physical exertion and/or high-charged emotions.
But I wondered about chest pain from a soft plaque rupture that resolves after a few minutes, something that might explain a sudden unfolding of chest pain for no reason (no physical exertion) that then goes away after a few minutes or so.
Obviously, a rupture is more likely to happen in a person with a ton of soft plaque versus in someone with a small amount. But having a small amount of soft plaque doesn’t guarantee no rupture.
How do you know if that recent chest pain was a soft plaque rupture?
Especially if you have low risk for heart disease?
“As with any biological system, there really is no ‘rule’ – only trends,” explains Dr. Reynolds.
“Obviously, those with risk factors TEND to develop more extensive coronary disease sooner than those without risk factors. But no one is guaranteed not to get coronary disease.”
Heart Attack & Plaque
“Many years ago, it was felt that most plaque builds up gradually over years until it eventually reaches a critical mass in obstructing the blood flow and the patient develops symptoms,” says Dr. Reynolds.
“More and more, however, we have come to appreciate that plaque buildup is not really a smooth process but can be described as a series of small ‘eruptions’ followed by healing.
“A small bit of plaque in an artery ‘ruptures’ and exposes the undersurface to the bloodstream where platelets and other clotting factors are stimulated to repair the rupture.”
- What happens when you pick off a scab?
- The scab is replaced by an even bigger scab.
“In a similar way, when the ruptured plaque is repaired, the new plaque is a little larger,” continues Dr. Reynolds.
“With repeated ruptures, the plaque can eventually reach critical mass and cause symptoms which prompt a cardiac workup and can lead to elective catheterization and stenting.
OR – the rupture can lead to such a vigorous platelet and clotting factor response that the artery goes from having mild non-obstructive plaque to total occlusion [blockage] in a matter of minutes.
“An acute rupture is now considered the mechanism for many of the patients who present with an acute heart attack or unstable angina.”
What are the odds that any given chest pain can be a soft plaque rupture?
This question applies to chest pain that doesn’t have an apparent trigger.
For example, mild chest pain can result from the motility of fecal matter building up through the large colon.
Some of the large colon runs in the upper abdominal area, so if a good chunk of BM is being transported through, it can cause mild chest pain.
The chest pain will gradually vanish, and then you’ll realize you have to do a big No. 2.
Acid reflux causes chest pain. Does it occur only when you lie down? That’s a tip-off, though acid reflux can hit when you’re upright.
Does “chest pain” occur only upon exhalation or inhalation? It’s likely a strained muscle or inflamed cartilage.
What about occasional chest pains that come out of the blue?
“Could it be plaque rupture and angina?” says Dr. Reynolds. “Maybe …. but I wouldn’t start with that. Each person is unique. Each comes with his/her own set of risk factors.
“Life is full of aches and pains. The overwhelming majority are NOT life-threatening. Common sense must prevail or we will be spending every waking hour in the hospital ER.”
Dr. Reynolds regularly sees patients for chest pain. “Very rarely is it ‘classic angina’ – it is usually some atypical presentation.
“Each time a patient comes in for an evaluation of chest pain, I do a complete history and get a good description of the pain.
“I do a physical exam and check the EKG. I assess the risk factors. If there is a moderate risk for heart disease, I will refer for a stress test and sometimes (not often) in patients with atypical pain, the stress test is positive.
“Those patients often go on to have a cardiac catheterization and some get a stent.
“And guess what – it is not uncommon that the patients with really atypical pain [who underwent stenting] come back to my office a few weeks later and STILL HAVE THE PAIN.
“Why? Because the pain wasn’t cardiac to begin with, but we just happened to find some coronary disease because, guess what – coronary disease comes with age!”
Kick Back the Soft Plaque
“Bottom line – do not walk around in a state of overwhelming anxiety about what might pop up around the next corner,” says Dr. Reynolds. “Eat right. Exercise. Don’t smoke. Enjoy life.
“Anxiety can only make everything worse – raise your BP and cholesterol, age you faster and maybe even accelerate heart disease. No one is immune to heart disease. But you must keep this in perspective.”
A hardcore overhaul of dietary habits can reverse soft plaque buildup.
Add rigorous exercise and you’ll reverse any heart disease even faster.
Think of all the exercise people did before machines took over.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Hriana
Do Doctors Give too Many Tests for Heart Disease?
What does a cardiologist have to say about the belief that doctors order too many tests for heart disease?
These tests include stress tests and angiograms.
There are also various blood tests related to diseases of the heart.
“Recent data has confirmed that we are over-testing our patients,” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“Regular echocardiograms and stress tests in patients with low risk profiles and atypical symptoms do NOT prolong life or improve quality of life.”
A low risk profile might be a man or woman under age 45 who does not smoke, does not have diabetes, does not have high blood pressure and is not overweight.
Another example of a low risk profile is a 55-year-old man who has always been an exercise enthusiast, has none of the problems mentioned above, is only a little overweight and has no family history of early-onset coronary artery disease.
What about stenting in patients with blocked arteries but no symptoms?
“In fact, stenting arteries that are partially blocked but have not caused symptoms does NOT prolong life or improve quality of life,” adds Dr. Reynolds.
The CT Angiogram
This non-invasive but radiation-emitting procedure involves looking at the inside of coronary arteries via the use of a contrast dye that lights up blood vessels on an imaging screen.
The CTA can view soft plaque buildup inside the arteries. Soft plaque is unstable in that a piece of it can break off and block blood flow or trigger a clotting mechanism that obstructs blood flow in the heart.
Dr. Reynolds explains, “CT angiograms looking for soft plaque is of very debatable use in a patient with a low cardiac risk profile and only atypical symptoms.
“Patients are better served by changing their diet, exercising more, and taking medications when necessary to reduce cardiac risk.”
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Satyrenko
sscpywrt26
Does Spinach REALLY Cause Black Stools?

Here’s a detailed look at black stools being caused by spinach.
Have you recently looked into the toilet bowl and noticed that your poops were black?
Did you panic?
Did you realize you recently ate spinach?
Spinach may cause stools to appear black. However, in my experience, I have another explanation.
I juice a lot of spinach, enough to sometimes make an 8 ounce glass of juiced produce that includes fruits and greens.
Drinking all that deep green from the spinach can have a striking effect on the color of your stools.
One day I noticed my BMs were nearly black — not like the color of coal, but near black enough to grab my attention.
I had ingested a larger-than-usual amount of spinach.
With a spoon I removed some of the BM, brought it towards the light above the sink and closely inspected it with my eyes.
The stool matter, turns out, was NOT black. It was very, very dark green. I mean REALLY DARK GREEN.
Have you ever seen a blackish-green car? It was kind of like that.
“Spinach contains iron,” says Lawrence Hoberman, MD, a board certified gastroenterologist and creator of EndoMune probiotic products.
“Large servings can cause the stools to be dark, but generally not black.”
Do not let this experience stop you from eating spinach!
Spinach is one of the healthiest-for-you vegetables.
It’s packed with essential vitamins and minerals like vitamins A, C and K, as well as folate, and of course, the iron.
This superfood is also rich in antioxidants, which help protect your cells from damage.
Also, it contains fiber, which supports digestive health.
Plus, spinach is super low in calories, making it an excellent part of a weight loss plan.
So next time you see what appears to be black poops in the toilet bowl, remove some with a spoon and give it a close visual inspection under a good light source to see what color it really is.
 With 40+ years’ experience, Dr. Hoberman is an expert in probiotics. He has extensive first-hand experience treating a variety of digestive health issues and has seen the dramatic results probiotics have had on his patients. endomune.com/meet-dr-hoberman
With 40+ years’ experience, Dr. Hoberman is an expert in probiotics. He has extensive first-hand experience treating a variety of digestive health issues and has seen the dramatic results probiotics have had on his patients. endomune.com/meet-dr-hoberman
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can a Skin Injury Turn into Cancer? Yes, but What Kind?

Yes, a skin injury can indeed develop into cancer, says a dermatologist.
There are three main types of skin cancer: melanoma, squamous cell carcinoma and basal cell carcinoma.
Can an injury to the skin lead to cancer?
“The answer is a resounding yes,” says Dr. Rebecca Tung, MD, a
“A past injury to the skin such as trauma from an accident which formed a scar, a vaccination site scar or even past exposure to radiation or caustic chemicals which resulted in scar formation can potentially turn into a skin cancer over time.”
How long does it take for a scar to morph into cancer?
“Typical malignant change may occur over decades in these cases,” says Dr. Tung.
“Signs that may alert you that your scar is no longer ‘just a scar’ include pain, redness, bleeding or skin breakdown.
“Scars and skin which has been persistently inflamed can turn into a type of skin cancer called squamous cell carcinoma.”
What is squamous cell carcinoma?
“This type of SCC is rare and was initially coined as a ‘Marjolin’s ulcer’ after the surgeon who first described the condition.
“There have also been reports of the more common type of skin cancer called basal cell carcinoma occurring in vaccination scars. Burn scars can also be the site of skin cancer years after the burn has healed.”
Excessive Sun not Always a Factor
“While most non-melanoma skin cancers (BCCs and SCCs) result from sun or ultraviolet exposure, research shows that long-term inflammation and scar formation can also create cancerous change in the skin,” says Dr. Tung.
“Your dermatologist can confirm the diagnosis of skin cancer by performing a skin biopsy.
“A scar (increased density of collagen in the lower part of the skin called the dermis) looks a world of difference away from a skin cancer (collections or islands of atypical cells) under the microscope.”
Be on Lookout for Changing Scar
“Have a changing scar? You owe to yourself to see a dermatologist to help determine if it has transformed into cancer.
“Again, when skin cancer is detected in its early stages, it’s often fully curable with surgical removal.”
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dermatology11
Stomach Cramps After Your Period Ends: Five Causes
Could abdominal cramping after menstruation ends be related to early cancer?
There’s actually a variety of causes for this troubling condition that all women should be aware of.
When a woman who’s completed her monthly cycle then has unexplained abdominal cramps — especially in the lower area of the abdomen — she might start fearing that the cause is ovarian or uterine cancer.
After all, these cancers DO strike fertile women. According to the National Cancer Institute Surveillance and Epidemiology and End Results Program, 28.9 percent of ovarian cancer diagnoses in the U.S. occur in women between 20 and 54. For uterine cancer it’s 23.4 percent.
What benign condition can cause abdominal cramping after menstruation ends?
This depends on how long after the period ends, that a woman experiences abdominal cramping, says Wendie Trubow, MD, an OB/GYN with Five Journeys, a membership-based wellness organization that uses functional and integrative medicine for evaluation and treatment.
In a menstrual cycle that lasts seven days, ovulation for the next cycle may begin in just a few days.
“So the cramping can be due to release of a dominant follicle from one of the ovaries,” says Dr. Trubow.
“This typically causes some fluid in the pelvis, and that can cause irritation and cramping.”
In a typical menstrual cycle, ovulation usually occurs around the middle of the cycle, often about 14 days before the start of the next period.
However, if your cycle lasts only seven days, this suggests a shorter overall cycle.
For example, if your cycle lasts 21 days, ovulation could happen around day 7, which means you may be close to ovulating as soon as the current cycle ends.
In this case, ovulation could potentially happen just a few days after your period ends.
Other Causes of Stomach Cramping Following a Period Include Cancer
“The cramping could also be due to fibroids, or a polyp or an IUD (intrauterine device),” says Dr. Trubow.
Discomfort from any of these conditions “is due to the body trying to get rid of a foreign body, and the uterus only really knows how to do a few things, including grow to accommodate a fetus, and contract, to get rid of whatever doesn’t need to, or shouldn’t be there.”
Irritable bowel syndrome and microscopic colitis (both are inflammatory bowel diseases) can cause cramping in the stomach or pelvic region.
Both conditions, though potentially capable of impacting one’s quality of life, are benign and can’t lead to cancer.
But speaking of cancer, ovarian cancer and uterine cancer can cause an abdominal cramp as well.
 Having practiced functional medicine since 2009, Dr. Trubowworks with women to identify causes of their symptoms and then works with them to achieve their greatest health and life balance.
Having practiced functional medicine since 2009, Dr. Trubowworks with women to identify causes of their symptoms and then works with them to achieve their greatest health and life balance.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Dragana Gordic
Source: seer.cancer.gov
Why Does Morbid Obesity Stop Menstruation?

Being morbidly obese, no matter how confident you are, can have a bad effect on your menstrual cycle.
It is no secret that when a very obese woman has been unable to conceive despite a lengthy time period of attempts, her size is to blame when all other tests — including those of her husband — have turned out normal.
“Morbid obesity can have either effect; either to stop menstruation, or to increase it,” says Wendie Trubow, MD, an OB/GYN with Five Journeys, a membership-based wellness organization that uses functional and integrative medicine for evaluation and treatment.
How Morbid Obesity Influences a Woman’s Period
“The mechanism is this: Circulating androgens are converted into estrogen by fat cells,” begins Dr. Trubow.
The more fat that you have in your fat cells, “the more conversion to estrogen. Ovulation occurs by ‘spikes’ in estrogen and progesterone.
“A constant stream of estrogen inhibits ovulation. If a woman does not ovulate, but has circulating estrogen, which serves to build the uterine lining, it will eventually shed.
“However, since the woman didn’t ovulate, the shedding doesn’t occur in an organized fashion (which is a typical menstrual flow).
“It occurs in a disorganized fashion, which can occur in varied amounts, at any time.”
So while some morbidly obese women struggle with reduced or ceased menstruation, others experience an increased flow of blood — which is never a picnic.
Solution to Menstrual Issues Caused by Obesity
The solution is weight loss. If you desperately are trying to conceive, you may want to put that plan on the shelf for awhile as you pursue safe weight loss via healthier eating, portion control, aerobic exercise and intense strength training.
Do not go on a crash diet to get the job done faster out of eagerness to conceive.
If you have the opposite problem — heavy periods — again, see if safe weight loss doesn’t correct this problem over time.
 Having practiced functional medicine since 2009, Dr. Trubow works with women to identify causes of their symptoms and then works with them to achieve their greatest health and life balance.
Having practiced functional medicine since 2009, Dr. Trubow works with women to identify causes of their symptoms and then works with them to achieve their greatest health and life balance.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Causes of Slow, Prolonged Menstrual Bleeding
Find out what can cause bleeding from your period to be slow and prolonged.
“Perhaps the most common cause of this is when the blood has difficulty passing through the cervical canal, due either to obstruction (perhaps a fibroid is in the canal), or to the cervix simply being ‘tight,’” says Wendie Trubow, MD, an OB/GYN with Five Journeys, a membership-based wellness organization that uses functional and integrative medicine for evaluation and treatment.
What can cause a tight cervix?
Dr. Trubow explains that this can be due to not yet having given birth, “or if the woman has had surgery on the cervix to remove abnormal cells and had scarring in the cervix, which makes it harder for the cervix to open to let the blood through.”
Another Cause of Slow, Prolonged Menstruation
“Alternatively, the bleeding could be slow due to inability of the uterus to contract, which can usually be attributed to fibroids,” says Dr. Trubow.
“Lastly, this could be bleeding due to an anovulatory [absent] cycle, so the bleeding is simply occurring in a disorganized fashion.”
Cancer and Vaginal Bleeding
Bleeding in between periods, or vaginal bleeding after menopause, needs to be checked out by a gynecologist because uterine, cervical and vaginal cancer can cause this symptom.
However, if you know the behavior of your period very well, and can recognize that the slow or prolonged bleeding is part of your menstruation, then the chances of this situation being caused by cancer are not likely.
Nevertheless, any kind of bleeding or spotting that is out of the ordinary, that has no confirmed explanation, needs to be evaluated by a doctor.
You should keep a documentation of the nature of your monthly cycles so that you can get acquainted with what your normal is.
Some women do spot before and after four or five days of actual flowing.
 Having practiced functional medicine since 2009, Dr. Trubowworks with women to identify causes of their symptoms and then works with them to achieve their greatest health and life balance.
Having practiced functional medicine since 2009, Dr. Trubowworks with women to identify causes of their symptoms and then works with them to achieve their greatest health and life balance.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Evan Lorne
How Common Is a Flesh Colored Melanoma?

Here’s what a dermatologist has to say about frequency of flesh colored melanoma — which can go undetected during your self-exams.
Melanoma can present as flesh colored.
But just how often does this occur?
How common are flesh colored melanomas?
“Amelanotic (flesh colored) melanomas are a rarer type of melanoma,” says Dr. Rebecca Tung, MD, a
“The incidence of amelanotic melanoma is only 2-8 % of all melanomas.
“They often appear as flesh colored to reddish lesions, often on the skin of the trunk, and do not follow the usual ABCD rules (asymmetry, border irregularity, color changes, diameter of 6mm or larger or growing in size) of melanoma detection.”
Sometimes, this flesh or pinkish/red colored melanoma can pass as basal cell carcinoma or squamous cell carcinoma.
A basal cell carcinoma is the most common cancer in the world. This easily curable tumor grows very slowly and very rarely spreads beyond locally.
Squamous cell carcinoma can spread, but it’s nowhere near as deadly as melanoma.
Both of these skin cancers are strongly linked to exposure to the sun.
Alarmingly, the amelanotic melanoma can also pass as a common pimple or blemish.
“Patients often initially mistake this type of melanoma as scars or pink moles,” continues Dr. Tung.
“Even under a special magnifying device called a dermatoscope, the features which usually signal cancer are often absent.
“For these reasons, diagnosis is frequently delayed.”
If you don’t have a good feeling about a new spot and especially “pimple” on your skin, you should have it removed.
“Suspicious lesions should be biopsied to confirm the diagnosis,” says Dr. Tung.
“Treatment is surgical with wide local excision.
“If the lesion extends deeply into the skin, lymph nodes may also need to be sampled (a procedure called sentinel lymph node biopsy) to determine if they do or do not contain melanoma.”
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Causes of White Peeling Skin Inside Lip Include Cancer
A dermatologist names cancer as a possible cause of white peeling skin inside the lip.
In addition to having just brushed one’s teeth, which can cause cells inside the lip to slough off, other conditions can cause the inside of the lip to develop a white, peeling reaction.
“Lichen planus (LP) is a condition that can affect the mucus membranes of the mouth,” says Dr. Rebecca Tung, MD, a
“It often looks lacy in a lattice pattern. While most cases occur on their own as a result of a body’s altered immune response, other cases can be the result of sensitivity or allergy to metal in dental work, or even a skin finding of an infectious viral hepatitis (inflammation of the liver; hepatitis C).”
Cancer As Cause of White Peeling Inside the Lip
“A more serious white patch on the inside of the bottom lip could be skin cancer — specifically squamous cell carcinoma (SCC) or its precancerous state (leukoplakia),” says Dr. Tung.
“Smokers, tobacco chewers and heavy drinkers are at increased risk for SCC.
“A biopsy of the lesion can confirm the diagnosis and direct treatment.”
In fair skinned people, squamous cell carcinoma is the second most common skin cancer, after basal cell carcinoma.
SCC is highly curable when caught early, but it kills thousands of Americans every year.
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.