Can Your I.Q. Be Too High to Have ADHD?
Can a Person Be Immune to ADHD Because of a High I.Q.?
Some people wonder if IQ can be too high for an ADHD diagnosis.
I know this question may seem quite silly, but it’s a popular one on at least one online support site for attention deficit hyperactivity disorder.
Thus, I decided to explore this topic with an expert in ADHD.
For this post I spoke with Dr. Robert Myers, creator of the Total Focus program at Legacy Publishing.
Dr. Myers is a clinical psychologist who has 30+ years of experience working with children, adolescents, families and parents, specializing in children and adolescents with attention deficit hyperactivity disorder.
Is there a connection between high I.Q. and ADHD?
“The answer is absolutely no,” says Dr. Myers. “People with ADHD are most likely to have average to above average IQs. Some are very intelligent.
“This is the source of frustration and confusion for the person with ADHD and those around them. They ask, ‘How can such a bright person be so flakey?’”
The Explanation
Dr. Myers says: “The answer is that these people have deficits in what we call executive functions that are related to such things as paying attention, working memory and planning skills. Their other brain functions are working fine.”
Have you been recently diagnosed with ADHD?
If all along you’ve known that you’re pretty smart, and are now stunned to learn that you have ADHD, you should not jump to conclusions yet over this surprising diagnosis.
(Though in many cases of adult-diagnosed ADHD, the individual is not surprised at all, as they’ve been living with this condition’s challenges all their life.)
Dr. John Huber explains in this article what it really means when an adult is diagnosed with ADHD.
One of the things it could mean is that you have untreated sleep apnea.
Sleep apnea, which can affect thin people and even kids and teens, can cause symptoms that mimic those of ADHD.
This is particularly true for children. Steven Y. Park, MD, an otolaryngologist, explains in this post what the signs are that a child with sleep apnea has actually been misdiagnosed with ADHD.
If anything is often connected to the symptom features of ADHD, it’s untreated sleep apnea, not I.Q.!
 Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Fidgeting Is Linked to ADHD and Has Benefits
A psychologist who specializes in ADHD talks about fidgeting.
Many people who’ve been diagnosed with attention deficit hyperactivity disorder (ADHD) would like to know if fidgeting is a behavior that comes with this collection of symptoms, and in addition to that, they’d like to know if it’s normal.
Sometimes they think it’s not normal at all.
For this article I spoke with Dr. Robert Myers, creator of the Total Focus program at Legacy Publishing.
Dr. Myers is a clinical psychologist with 30+ years of experience working with children, adolescents, families and parents, specializing in children and adolescents with attention deficit hyperactivity disorder.
Dr. Myers explains, “Fidgeting is basically activity to work off excess energy. People who are nervous often fidget when they are worried about something.
“Fidgeting is a symptom often found in kids and adults with ADHD, and then it is a symptom of hyperactivity.
“If it’s not interfering with a person’s ability to do whatever they are doing and it’s not annoying to others, who cares.”
When I was 13, my biology teacher, a nun at the Catholic high school I attended, pointed out that I kept fidgeting in my seat (leg movement).
I told her that it burns more calories. My belief that it burned more calories was one reason I made a point to fidget, though it was also a subconscious habit.
She thought I was nuts and promptly discredited my theory that fidgeting burns more calories.
MANY YEARS later … research was conducted on this very idea, and showed that, indeed, fidgeting contributes to enough extra calories burned to make a difference to someone wanting to be five or even 10 pounds lighter.
And to think that when I was just 13, I was already figuring this out. Maybe I had ADHD, maybe I didn’t.
But realize this: Studies support fidgeting as a means of burning more calories, and those who fidget tend to be leaner.
It’s not natural for the human body to be dead still for long periods in a chair.
THAT’s when you should worry — when you sit for prolonged periods with little movement.
In fact, the more immobile a person is while seated, the higher the risk of developing a dangerous deep vein thrombosis.
ADHD is no reason to try to sit dead still, especially if the chair is not comfortable.
Having ADHD never means you should attempt to behave like a statue.
If you do a lot of sitting, make a point of fidgeting your legs, even if you have ADHD, because this will lower the risk of developing a blood clot (risk of blood clot goes up with inactivity).
This is why it’s strongly advised that when sitting in an airplane, you regularly move your legs about to prevent a deep vein thrombosis.
As I type this article, my left leg is going. The human body was not meant to sustain long periods of immobility.
Update
In March 2022 I was diagnosed with Autism Spectrum Disorder.
My “fidgeting” is the result of my autism. I did not meet the criteria for ADHD.
Nevertheless, my stimming (repetitive movements) makes my body burn more calories than if I didn’t engage in so much stimming throughout the day. It really adds up!
 Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Leg Shaking Be Caused by ADHD?
A psychologist who specializes in ADHD comments on leg shaking.
“Leg shaking, like fidgeting, is often associated with anxiety or hyperactivity related to ADHD,” says Dr. Robert Myers, creator of the Total Focus program at Legacy Publishing.
Dr. Myers is a clinical psychologist with 30+ years of experience working with children, adolescents, families and parents, specializing in children and adolescents with attention deficit hyperactivity disorder.
“Usually the person is not aware they are doing it. It is a habit that can occur whether the person is relaxed or stressed out.
“If it is bothering others, you could try to point it out so they can stop and perhaps become more aware of it and work on gaining control.
“Sounds easy, but for some it’s not as easy as you might think.”
Does ADHD Directly Cause One or Both Legs to Shake?
“ADHD” is a reference to a composite of symptoms including hyperactivity and difficulty maintaining focus on a task.
Other features include struggling to get tasks completed, disorganization, often losing items, difficulty waiting one’s turn, interrupting conversations, trouble with planning, poor time management and difficulty sitting still.
But despite the part of difficulty sitting still, ADHD does not directly cause anything to happen to a leg.
However, as Dr. Myers had pointed out, the symptoms that are associated with this commonly-diagnosed condition can cause shaking of the legs. This includes impatience with waiting for one’s turn.
Now, if a child or adult is in the habit of bouncing a leg up and down on the ball of the foot while seated, or rapidly moving the foot side to side while the leg is outstretched while seated or lying, or in some other way allows the leg to voluntarily quiver – this does not suggest that the individual might have ADHD.
It often just amounts to a nervous or comforting habit that makes time seem to pass more quickly depending on the circumstance, such as waiting for one’s dental appointment.
I see leg shaking all the time at the gym while people are resting in between sets of upper body exercises.
In fact, I’ve seen it while a person is using their phone in between sets.
It’s not accurate to deduce that all of these people have ADHD.
Leg Shaking and Autism
Leg shaking, which of course can come in various forms, can be the result of autism.
This doesn’t always mean nervousness or anxiety.
I myself have a clinical diagnosis of ASD (and autism only; no ADHD), and I’ve been bouncing a leg since childhood.
It’s a habit. It usually occurs subconsciously regardless of my state of mind.
It could be a quick bounce or a slow bounce. It could be up and down (“knee bouncing”) or sideways (thigh swaying).
It just doesn’t feel natural to sit still.
These movements, particularly when referring to autism, are known as “stimming” (self-stimulatory or self-regulating behavior).
It’s also important not to equate voluntary leg shaking with the involuntary quivering or trembling that may occur from a bout of intense exercise.
For example, intense use of a leg press machine can result in quivering legs.
 Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/GBALLGIGGSPHOTO
Is Walking on One’s Toes Caused by ADHD?
Here is what a psychologist says about the connection between walking on one’s toes and ADHD.
Where did the idea ever originate that walking on one’s toes is a symptom or indicative of attention deficit hyperactivity disorder?
If a child (or adult) has difficulty locking their attention span on something, why would this cause them to walk around on their toes?
As silly as this question is, it’s one that a lot of people would like to know the answer to.
The Connection Between Toe Walking and ADHD
“Toe walking is not linked to ADHD,” says Dr. Robert Myers, creator of the Total Focus program at Legacy Publishing.
Dr. Myers is a clinical psychologist with 30+ years of experience working with children, adolescents, families and parents, specializing in children and adolescents with attention deficit hyperactivity disorder.
He explains, “Toe walking can be a sign of a number of neurodevelopmental disorders and needs to be evaluated by a specialist.
“Some children with autism may have this symptom — as well as possible symptoms similar to children diagnosed with ADHD.
“My guess is that this is the cause for the confusion about this symptom.”
The idea that walking on one’s toes might be linked to ADHD is not widely supported by established research.
But yes, it has come up in clinical and layperson discussions, likely due to overlapping behaviors with autism or misunderstandings of motor patterns.
Toe-walking kids may also have been initially diagnosed with ADHD — only to be re-diagnosed later with autism spectrum without the ADHD.
This phenomenon could also explain the misunderstanding that ADHD causes habitual toe-walking.
Though an ADHD child may, indeed, at some point walk on their toes due to fleeting excitement or just for the heck of it, this motor pattern is not a universally acknowledge trait of ADHD.
Walking on one’s toes, even in adulthood, can also be due to a sensory processing disorder.
It’s also not uncommon for autistic adults to walk on their toes for sensory input or because they don’t like the feel of their heels making contact with a surface.
As children, adults with ASD would have very likely walked on their toes as well.
Do Typical Kids Walk on Their Toes?
Yes, all the time. You’ve seen it plenty: typical children walking around on their toes. There’s a novelty about it.
In fact, this helps strengthen the ankles. An adult may include a little toe walking during an exercise session for this very reason.
Of course, there is a time and place for everything.
If your child walks on their toes during inappropriate times, then this should be corrected (don’t scold or insult; just merely point out not to do it).
True signs of ADHD include what these letters stand for: a deficit in the ability to maintain one’s attention — what would be considered a normal degree of attention span for a child’s particular age — paired with hyperactivity and lack of impulse control that’s out of proportion for the event at hand.
 Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can Bad Sense of Direction Be Caused by ADHD?
An expert on ADHD answers the question: Can attention deficit hyperactivity disorder cause bad sense of direction?
A bad sense of direction can be evident in children when they ride their bikes or navigate the interior of their new school.
For older kids it can manifest itself inside a large retail store or unfamiliar neighborhood.
For adults with a bad sense of direction, they will be aware of this when driving in a new town, or hiking or running on unfamiliar trails.
Not everyone with a “bad sense of direction” has attention deficit hyperactivity disorder.
But the fair question remains: Can ADHD actually cause a poor sense of direction?
“Poor sense of direction such as confusing left and right sometimes goes along with dyslexia,” begins Dr. Robert Myers, creator of the Total Focus program at Legacy Publishing. Dr. Myers is a clinical psychologist with 30+ years of experience working with children, adolescents, families and parents, specializing in children and adolescents with attention deficit hyperactivity disorder.
“Some people with dyslexia may also have ADHD,” continues Dr. Myers.
This explains why some people wonder if attention deficit hyperactivity disorder actually causes a person to have a bad sense of direction.
But look at it in reverse: Imagine having a bad sense of direction. See if you can then imagine this having anything to do with ADHD.
The neurodevelopmental disorder known as ADHD can cause numerous issues.
These include frequently misplacing items, challenges with working memory, difficulty maintaining attention, becoming easily distracted, impulsiveness, excessive talking, poor time management, taking unnecessary risks, problems being organized and struggling to complete tasks.
Like Dr. Myers says, a person can have both situations — ADHD plus a poor sense of direction — but that doesn’t mean that the conditions are causally linked.
In fact, there has been no research showing any causal relationship between ADHD and getting lost easily.
Though some adults have a lousy sense of direction, keep in mind that by nature, very young children aren’t the best at navigating through unfamiliar surroundings such as a big house that they’ve never been inside of.
You should not assume that you, or your child, might have ADHD simply because the child’s or your sense of direction seems crummy.
 Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
Dr. Myers has 30+ years’ experience working with children, adolescents and parents, specializing in children and adolescents with ADHD. Total Focus is a comprehensive program to improve attention, concentration and self-control in children.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
MICROSCOPIC COLITIS: DIARRHEA, JOINT ACHES, OTHER SYMPTOMS

Did you know that microscopic colitis can cause joint aches?
The exact mechanism is not clearly known, but have you noticed that often, either in the days (or weeks) preceding a microscopic colitis flare…you have strange aching in your low back, ankles, neck, even wrists?
You may also have muscle aches, such as in the back of the upper legs and also where the top of the thigh meets the pelvic area.
Some people have even reported aching in their arm muscles.
All of these issues are most likely connected to this inflammatory bowel disease, and sometimes may occur at the same time as the diarrhea.
It’s a phenomenon called enteropathic arthralgia.
A small percentage of people with MC (lymphocytic and collagenous) experience enteropathic arthralgia.
“Enteropathic” refers to a disease process that involves the intestinal tract.
“Arthralgia” translates to joint pain. This is different from “arthritis,” because the “itis” means that something’s inflamed (the joint). “Algia” in medicine means pain.
Thank goodness that the enteropathic arthralgia in microscopic colitis is only a pain issue, rather than a degenerative issue of the joints.
The following links will take you to articles about microscopic colitis and enteropathic arthralgia.
Many of these articles contain information from gastroenterologists whom I interviewed, while the rest are based on my personal experience with this quirky but benign condition (I was diagnosed in 2010), and my extensive research.
ENTEROPATHIC ARTHRALGIA
- Time lapse between joint pain flare and diarrhea and how this process occurs
- How does MC joint pain compare to ulcerative colitis and Crohn’s?
- Detailed description of what microscopic colitis joint aches feel like
- PMS joint aches vs. those of microscopic colitis
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
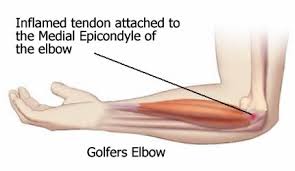
Elbow Pain: How to Get Your Deadlift Back
If you have elbow tendonitis, it can greatly interfere with the deadlift.
The type of elbow tendonitis that I had is called medial epichondylitis (golfer’s elbow).
Just a little gripping would aggravate it. My initial therapy (hand grips and very gradual over time increase of resistance on the close-grip hammer-grip pull-down) was working well.
Then I did some very heavy yard work and messed things up. The initial therapy then proved to be worthless.
I then decided to do the two exercises that aggravated the problem the most: farmer walks, and the deadlift.
To my distress, I discovered that a barbell deadlift (which I had been avoiding for a very long time due to this injury) of more than 50 pounds aggravated the tendon. A farmer walk with 15 pound dumbbells aggravated it as well.
You Need a Starting Point
But I decided to make that a starting point. Below is the program I used. It took approximately TEN MONTHS to get my deadlift up to 135 pounds (reps). I consider that a major milestone.
Keep in mind that my inability to initially deadlift more than 40 pounds was due to feeling a tweak in the elbow, rather than lacking the strength.
Same with the farmer walks; carrying the 15 pounders induced an unpleasant feeling in the elbow.
This sensation meant that the tendon was being aggravated.
So do not think in terms of strength. This is rehabilitation of the tendon in your elbow.
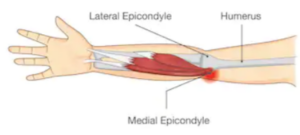
Shutterstock/solar22
Getting Your Deadlift Back After an Elbow Tendon Injury

Shutterstock/Nomad_Soul
– At first, six to seven days/week, do farmer walks.
– Deadlift twice a week (Monday and Thursday; Tuesday and Saturday; or Wednesday and Sunday).
– Use a weight for the farmer walks that you can walk around with, literally for five minutes nonstop without making you “feel” anything going on with your elbow. If you can feel anything that you shouldn’t, use a lighter weight.
– Do this three times a day for one week at the same weight.
– Every week, increase the farmer walk weight to the next possible increment. I had three sets of dumbbells at home: 10, 15 and 35 pounds.
Progressive Load of the Weights
Once I was ready to go heavier than 15 pounds, I decided to bring in sets of 3, 5 and 8 pound dumbbells.
I then took four paper grocery bags that had handles. I doubled them up, then placed a 15 pounder and 3 pounder in each (or a 10 and an 8). This way, I could farmer walk with 18 pounds.
Why not just hold the dumbbells without the paper bags?
Because this was being done at home (and daily) where I did not have access to every incrementally-weighted dumbbell at the gym.
After a week I put a 10-, 8- and 3-pounder in each bag, for a 21 pound farmer walk. The doubled bags were sturdy enough still.
I kept increasing over time, so that eventually, I had a 15- and a 10-pounder in each bag. I then put a 15-, 10- and 3-pounder in each bag.
When I was in the gym, I used their incremental dumbbells. However, once I got up to 28 pounds, I decided to par back the farmer walks to three times a week (only at the gym).
This is tedious work: walking around holding dumbbells for five minutes. But this should re-train a compromised elbow tendon to be efficient.
However, the five minute rule can be broken at around 20 pounds. Three minutes will do.

The progression with the farmer walks went a lot slower than with the deadlift.
This is due to the positioning of the hands while carrying the weights; it puts more stress on the tendon.
When I got to 40 pounds with the farmer walks, I still considered myself in rehab mode.
I was strong enough to use 50 pounders, but this would bring out the tweaky feeling in my elbow.
I then built up to farmer walks with a 45 pound plate in each hand (the style with the openings at varying points around the hole).
The plates are easier on the elbow tendon because they don’t require as much of a grip.
More on the Deadlift Rehab
– Do eight reps of the deadlift with 90-120 seconds in between sets, six sets total. This will be very tedious due to the long rests and the ridiculously light weight.

Shutterstock/Vladimir Sukhachev
Do not use a weight that makes you “feel” your elbow tendonitis. Work just below that point. Increase the weight five pounds every two weeks.
If the increase results in “feeling” the tendonitis, return to the previous weight! It took me 10 months with this approach to get from 50 pounds to 135 pounds.
The long rests will protect the tendon from over-work. Do half the sets with an underhand grip and half with an overhand. Do not mix.
– For deadlifts with pre-fixed barbells or an Olympic bar with 25 pound plates or less on it, there’s no need to touch the plates to the floor. Go down as far as you would if you were using 45 pound plates.
– When you get to 35 pound plates, it’s okay, but not necessary, to touch the floor with them.
– If you decide to make contact with the floor, DO NOT BANG THE PLATES! This will force the elbow tendons to absorb some of this!
Instead, gently touch the floor—so gently that you’re the only one who hears it. This includes at the end of each set.
– When you get to 95 pounds, increase the rest to two minutes. The set range can be six to eight.
– You are still increasing by only five pounds every two to three weeks. You’ll be tempted to make bigger increases if the weight you’re using is still very light relative to what you were lifting pre-injury.
The elbow tendonitis is the weakest link and it calls the shots, no matter how much weight your legs, back and shoulders want to lift.
– Don’t assume that once you get to, say, 120 pounds, you’ll be able to increase the incremental gains from five pounds every 2-3 weeks to 10 pounds. Stay with five.
I made a 10 pound jump and “felt it” in my elbow. So I backed down to the five pound increase (and my elbow felt fine).
– Don’t worry what people think when they see you using a light barbell, when you know that they’ve seen you in the past with a much heavier weight! This was difficult for me to digest, but I had to get used to it.
Getting your deadlift back from elbow tendonitis begins with accepting the fact that you will have to be lifting peanuts for many months.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lag Time Between Joint Pain & Diarrhea in Microscopic Colitis
Why can there be a time lapse between joint-pain onset of microscopic colitis and the onset of diarrhea?
It’s possible for a flare-up of microscopic colitis to consist of, initially, some joint aches (some patients may refer to it as “pain”), without the diarrhea, even though the gushing- or porridge-like diarrhea is a hallmark feature of this inflammatory bowel disease.
When a person with microscopic colitis has a flare, the joint pain and the diarrhea won’t always come at the exact same time.
The arthralgia may precede the diarrhea.
Why is this?
“Lag time may be caused by a combination of factors: diet, exercise, genetics, sleep patterns, stress, environment, ongoing medical conditions, viruses, infections, and your body’s individual inflammatory load,” explains Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“The inflammatory load – how much inflammation the body is enduring and how much it can handle – varies from person to person.
We have built-in mechanisms that are supposed to help neutralize inflammation, but when your system becomes too overwhelmed, something has to give.”
To reduce inflammatory load, eliminate as many processed foods as possible. This means avoid eating foods from cans and boxes.
Eat as you would if there were no such thing as food factories or processing plants.
If you DO eat anything processed, opt for a minimally processed version, and make sure there are no unnatural ingredients. The more ingredients, the more processed.
The closer a food is to its natural form, the less pro-inflammatory it is: An apple is better than apple sauce is better than bottled apple juice is better than apple pie.
If you awaken one day with joint aches but no other new symptom, and you’ve already been diagnosed with microscopic colitis, and even if your last (and only flare-up) was several years ago, then consider this:
And that is the the possibility that this new-onset arthralgia is part of another flare-up of microscopic colitis and is simply lagging behind the characteristic diarrhea that will eventually be coming.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Emily frost
Joint Pain in Crohn’s, Ulcerative Colitis vs. Microscopic Colitis

Is the mechanism of joint pain or aches in Crohn’s & ulcerative colitis the same as that in microscopic colitis?
“Enteropathic arthropathy” is the name for joint aches caused by inflammatory bowel disease.
The two most well-known and researched inflammatory bowel diseases are Crohn’s disease and ulcerative colitis.
One of the problems they can cause is joint pain (or aches), also known as arthralgia.
This phenomenon is called enteropathic arthropathy.
But there’s a relatively new kid on the block: microscopic colitis, an inflammatory bowel disease first described in 1976—which is recently, in terms of medical history.
There’s been a lot of research into Crohn’s and ulcerative colitis, which are far more common than MC.
I wondered if the mechanism of joint discomfort (pain, aches) in all three of these IBDs is the same (or at least, very similar).
“In both Crohn’s and ulcerative colitis, there’s a disruption of the microbiota – the microbes that live in the intestine,” begins Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“People who suffer from Crohn’s disease can’t handle their own microbiota. They lack the enzymes to recognize that those bacteria belong down there, so the small and large intestine become inflamed.
“This may be related to increased gut permeability, which we also see in microscopic colitis patients.”
Enteropathic Arthropathy
“In addition, many people who have been diagnosed with gastrointestinal conditions – like Crohn’s or microscopic colitis – also suffer from aching joints,” continues Dr. Fine.
“We know there is a correlation between joint aches and gastrointestinal distress, but we do not yet fully understand it.
“We know they are both associated with inflammation, so perhaps it is an overload of inflammation that spills over to other parts of the body.
“It’s also possible that the patient’s chromosomes are being affected.
“Perhaps when one part of the gene starts becoming exposed, it carries over to a neighboring gene – so microscopic colitis may affect the eyes or the joints because they are near each other on the chromosome. All of this is pure speculation, of course, but it’s worth exploring.”

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/FineShine
Source: emedicine.medscape.com/article/180664-overview
Why Does Microscopic Colitis Cause Joint Pain in Some Patients?
A gastroenterologist comments on microscopic colitis and one of its associated symptoms, joint pain.
Symptom lists for microscopic colitis sometimes include “joint pain,” though the pain may feel more like an ache or dull discomfort.
This inflammatory bowel disease is infamous for its signature explosive diarrhea.
But that’s not all it causes.
A small percentage of patients experience enteropathic arthralgia.
Diarrhea + Joint Pain in Microscopic Colitis
Are these chemical messengers, or their precursor, COX 2, somehow involved in the arthralgia that’s associated with microscopic colitis?
“Aching joints can be a symptom of microscopic colitis, but not necessarily,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“Many patients with aching joints don’t have microscopic colitis, but aching joints and gut problems often go hand-in-hand.
“They’re both associated with inflammation, and many doctors speculate that cyclo-oxygenase (COX 2) or prostaglandins are involved because of the function they provide.
“Prostaglandins are chemicals that generally cause inflammation of our joints.”
Many people with MC report that a specific diet has helped manage or even eliminate symptoms.
It stands to reason that an anti-inflammatory diet would be of great value.
A pro-inflammatory diet promotes body-wide inflammation.
To minimize this, do whatever you can to eliminate processed foods.
That’s the biggest thing you can do to reduce systemic inflammation.
Processed foods often contain additives, excess sodium and unhealthy fats that contribute to inflammation and various health issues.
Instead of opting for pre-packaged meals, choose whole, fresh ingredients.
For example, if you want chicken, potatoes and broccoli for dinner, buy these items fresh and prepare them at home.
Cooking and seasoning from scratch not only enhances flavor but also ensures you’re avoiding hidden additives and preservatives found in frozen or pre-packaged versions.
This approach promotes better health and helps manage inflammation more effectively.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.