How Doctors Can Tell if High Blood Pressure in One Arm Is Serious

If your doctor finds that the blood pressure in one of your arms is high but not the other, this is serious and needs to be pursued.
“Doctors evaluate you based on many factors, not only physical findings,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“The first thing your doctor considers is your overall risk of any diseases such as cardiovascular disease,” she continues.
“There are risk factors known to put you at increased risk of a dangerous event like a heart attack or stroke.
“These risks include diabetes, high blood pressure, high cholesterol, smoking and a family history of early heart disease.”
A Study
“A study has shown that consistent readings of blood pressure with differences of 10-15 points between the two arms is a marker for increased risk of heart attacks and strokes.”
This is one reason why it’s so important to periodically take your blood pressure in both arms. It’s easy to do at your kitchen table.
“A new finding of a very large difference between the two arms would trigger your doctor to do further investigation with testing,” says Dr. Denier.
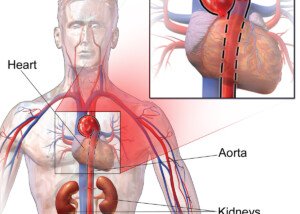
“The most sinister cause of differences in the blood pressure in both arms is aortic dissection or a tear in the aorta.
“It would be very unusual for someone to have this condition without other obvious signs and symptoms.
“The doctor would be looking for these signs very carefully even if he or she does not seem to be” having an aortic dissection.
The most blatant symptom of an aortic dissection is a ripping pain in the chest, which can radiate to the back.
But if you don’t have chest pain but still have big differences in blood pressure in your arms, see a cardiologist.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Alexander Raths
High Blood Pressure in One Arm: Serious Problem or Not?

Should your doctor be alarmed if you have high blood pressure in one arm and what does this mean?
“High blood pressure in one arm is something that is important to notice and report to your doctor,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“If your doctor seems unconcerned, it may be because he or she already knows you well and understands your medical conditions and what is normal for you. Do not assume this, of course.”
Have you discovered, using a home blood pressure gadget, that one of your arms has high blood pressure?
“It’s always wise to bring a finding that concerns you to your doctor’s attention,” says Dr. Denier.
“It’s common to see small differences in the blood pressure readings of each arm.
“Differences of 20 millimeters of mercury for the systolic or 10 mm Hg for the diastolic may be a sign of a health problem.
“This can be caused by narrowing of the blood vessels that travel to that arm.
“Other things that may cause this are chronic kidney disease, diabetes or atherosclerosis, all of which are risk factors for cardiovascular disease.”
My father has a history of having high blood pressure in one arm—not that high, but in the low range of what would be considered “high.”
He was told to take a reading daily and record the numbers.
He doesn’t have diabetes or chronic kidney disease, but he does have heart disease.
His coronary calcium score three years ago was 1195. Over time, the particular arm eventually began yielding readings under 140/90. His doctor was never alarmed over this.
Alert your doctor if you discover that the blood pressure in one arm is higher than the other.
Nevertheless, your doctor should know if you’ve uncovered this phenomenon via a home blood pressure gadget, to see what this finding may mean for your unique medical situation.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Syda Productions
What Blood Pressure Higher in One Arm Can Mean

What can it mean when one arm has higher blood pressure than the other?
“Blood pressure readings come from the blood flowing through the vessels in the arm (or leg) which can be heard with a stethoscope,” says Donna Denier, MD, with The Cardiology Center with the Appalachian Regional Healthcare System.
“When readings are significantly different on both sides (20 systolic points or 10 diastolic points), it suggests that the flow of blood is different on the two sides,” continues Dr. Denier.
Blood Flow Differs on Both Sides of the Arm: Why Is This?
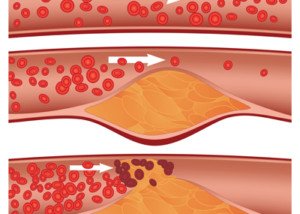
Dr. Denier explains, “Things that block flow in the arms are the same as those which cause blockage in the coronary arteries or other arteries in the body.”
This means that the arteries in the arm are clogged with the same fatty deposits or plaque that are involved with coronary artery disease.
“Diseases like chronic kidney disease and diabetes or conditions like high cholesterol or habits like cigarette smoking can all lead to blockage in the arteries anywhere in the body,” warns Dr. Denier.
“Finding it in the arms can be a warning that other vessels may also be blocked.”
If the blood pressure of one of your arms is higher than the other, you should undergo cardiac testing to see if your coronary arteries might have blockages.
One such test is the treadmill (or stationary bike) echocardiogram stress test. It measures blood flow through the three main coronary arteries during the exertion of exercise.
Home BP Measuring
• Before taking the measurement, make sure you have been seated and calm for five minutes.
• Do not cross your legs, not even at the ankles. They should be in a co mfortable, relaxed position and not up against anything. Keep them still, including your feet.
• The device’s cuff should be against bare skin, not clothes, for optimal accuracy.
• Keep the arm that’s being measured resting on a table, desk or the chair’s arm rest.
As innocuous as this finding may seem — that blood pressure is higher in one arm — you should report this to your doctor if you’ve discovered it with a home blood pressure device.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ kurhan
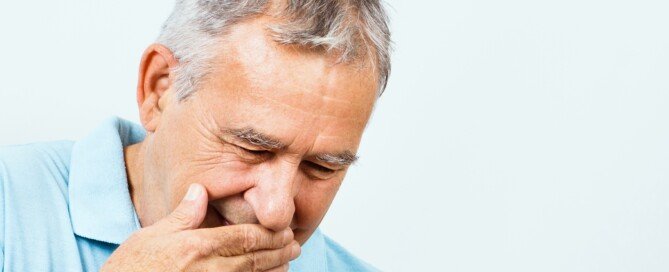
Chest Pain: Persistent vs. Intermittent vs. Sharp vs. Dull Ache

Here is what a cardiologist says about different kinds of chest pain like sharp, dull, persistent, intermittent.
How can the different types of chest pain—constant, intermittent, sharp and dull/achy be distinguished from each other?
“Chest pain that is intermittent and related to physical and/or emotional stress is more likely to be angina and related to the heart,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“With any intermittent pain, it’s important to look for the things that bring it on like exercise, eating or coughing.”
When a pain or ache of a come-and-go nature strikes, make a note of this: time, body position, recent foods eaten.
See if a pattern develops over time. For example, you may find that almost always, a particular type of brief aching in your chest occurs one or two days after your chest workout at the gym.
“Sharp pain is more likely to be inflammatory in nature, where dull pressure or tightness is more like cardiac pain,” says Dr. Denier.
Though a dull pressure or tightness is a common description in the symptom lists of gastroesophageal reflux disease, do NOT assume this is what you have before you’ve had your heart checked!
Though acid reflux is very common, so is heart disease.
Furthermore, a dull pressure or tightness in the chest, that isn’t correlated to food intake or related to acid reflux, is great cause for concern.
If it’s not heart related, it can still be potentially serious—like a bleeding ulcer in the upper esophagus.
“Persistent pain is usually not caused by the heart unless the person is having a heart attack.
“Angina comes and goes. Pain can be differentiated based on the other symptoms and findings that go with it and the risk factors for that particular person.”

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Oleg Golovnev
If You Upchuck for no Reason, Could It Be Caused by Angina?

Vomiting can definitely be related to a problem with the heart, including angina.
“Angina can lead to vomiting, and it is one of the important signs of a heart attack,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“Vomiting can be a response to any pain. It is caused by stimulation of the autonomic nervous system.
“When it occurs in the presence of chest pain, it is very concerning.”
Two days before my mother underwent emergency quintuple bypass surgery, she had a few episodes of light vomiting, following an episode of difficulty breathing. Two days later she had chest pain.
After her second ER visit in three days she was diagnosed with unstable angina, and that evening had the bypass surgery.
“Other signs to look for are sweating, pale cool skin. These are all signs that someone may be having a heart attack.
In some patients, such as women and diabetics, nausea and/or vomiting may be the only symptom of the heart in need of oxygen.”
HOW does angina lead to vomiting?
“Vomiting in the presence of chest pain is caused by increased activity of the autonomic nervous system,” says Dr. Denier.
“The ANS is stimulated when a person is under severe stress and suffering from pain.
“Internal organs can become stressed when they do not get enough oxygen and that can trigger the ANS leading to nausea and/or vomiting.”
Two Main Types of Angina
Angina pectoris is chest pain resulting from reduced blood flow through the heart.
The stable type means that the problem occurs in response to physical exertion or emotional stress like anger.
Unstable angina refers to reduced blood flow at rest, for no apparent reason.
This can even occur while someone is asleep, and then the chest pain wakes them up.
In such a case, it’s not likely they’ll be awakened by the need to vomit.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/InesBazdar
Bodybuilding Guidelines after Heart Bypass Surgery (CABG)

Straight from a cardiologist, here are the guidelines for bodybuilding after having heart bypass surgery, a.k.a. CABG.
CABG stands for coronary arterial bypass grafting, and there are two kinds of patients when it comes to bodybuilding:
1) Those who wonder if they can continue bodybuilding after they recover from the heart bypass operation, and
2) Those who’ve hardly ever touched weights, but would like to take up bodybuilding once they fully rehabilitate from their CABG.
“Assuming the patient underwent cardiac rehab successfully, he should be able to perform strenuous activities including weightlifting,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
“Even a patient who has sustained permanent damage from an MI [heart attack] or has heart failure following CABG, should be able to begin strength training. The physical limitation would be based on symptoms only.”

So if you’ve been into bodybuilding all along, then you can resume it without a hitch — once you have completed your post-op cardiac rehab program.
“Assuming the patient is fully revascularized with no residual blockages that were left unaddressed, there is no limitation,” says Dr. Cohen-Stevens.
In case you’re wondering how a bodybuilder would wind up needing heart bypass surgery in the first place, consider the following:
Some bodybuilders hardly ever, if at all, do structured aerobic exercise. Next, steroid use can damage coronary arteries.
But in non-steroid users, you must consider a lack of aerobic exercise, and a diet that promotes systemic inflammation (which can lead to heart disease).
Not all bodybuilders have Zen-like diets or are faithful to cardio-centric exercise. Remember, their goal is physique sculpting, not running long distances.
If you’ve had (or will have) heart bypass surgery but have never done any bodybuilding, but would like to take up this endeavor, then once you complete your cardiac post-op rehab regimen, your biggest issue will be the orthopedic element of strength training.
That is, you don’t want to rush into lifting heavy weights simply because this can strain untrained tendons and muscles.
The biggest limitation, then, in the novice is that of an out-of-condition musculoskeletal system.
So though your heart may be doing just fine and may be ready for some more serious strength training, your rotator cuffs or low back structures may require a slower entry into more serious weight lifting.
Dr. Steven-Cohen also explains, “Patients should keep in mind that not all coronary disease is revascularized, and CABG is not ‘all new arteries,’ and you may not be completely symptom-free.
“We are able to open moderate to large size vessels that have a significant blockage (> 50%) with symptoms.
“Disease in smaller vessels or diffuse disease, may not be addressed with a stent or bypass.
“It is possible to have symptoms because of these blockages that would require titration of medication and may limit ability to exercise.”

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
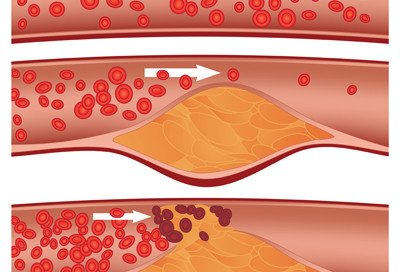
Can Exercise Cause Soft Plaque to Rupture?
Just who should worry about soft plaque rupture every time they work out?
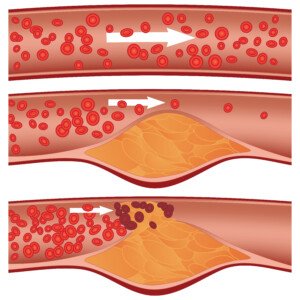
“We define plaque in two ways,” begins Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
“Soft/unstable vs. stable/calcified plaque. Soft plaque is considered more unstable and is the plaque thought to rupture to cause myocardial infarctions [heart attacks], whereas stable plaque is more likely to cause predictable angina with exertion.”
Dr. Stevens-Cohen continues, “Soft plaque may rupture at any time. Normally, it doesn’t cause symptoms,” in that, despite the rupture, blood flow is not inhibited.
“We don’t know what causes soft plaque to suddenly rupture and trigger the sequence of events culminating in MI [heart attack].
Can exercise increase the odds of soft plaque rupturing?

Shutterstock/Liderina
“A sudden increase in demand of the heart, i.e., by increasing heart rate (strenuous exercise or any exercise in a patient not used to exercising) can change the workload of the heart and precipitate symptoms.”
If as an absolute rule, intense exercise (or any level exercise) increased the risk of soft plaque rupture, then people in gyms, on tennis courts, hiking trails, etc., would be dropping left and right from heart attacks.
But then again, bear in mind that people who regularly engage in gym workouts, tennis and basketball games, jogging, etc., in general have far better heart fitness and health than do sedentary people.
The problem is when a sedentary person, whose heart is NOT used to a hard workout, one day engages in a hard workout (shoveling snow, chopping wood, helping a friend move, hiking for the first time in years, etc.).
THIS is the person who’s at greater risk of suffering a soft plaque rupture that can result in a heart attack.
“Yes, most sudden MIs or what we call massive heart attacks that change the ECG (the true medical emergency where we want the vessel open in < 90 minutes), occur in the rupture of soft plaque,” says Dr. Stevens-Cohen.
“With the increase in demand caused by sudden exercise/excitement [in a deconditioned person], a not so stable plaque may rupture, exposing the inside of the plaque to the bloodstream and causing a thrombus to form.”
So if your body is already well-acquainted with intense exercise, you don’t need to worry as much about a soft plaque rupture as you perform your deadlifts, chin-ups to exhaustion, squat jumps or high intensity interval training.
It’s your paunchy, sedentary neighbor who’s out there hurriedly shoveling snow who’s at notable risk of that soft plaque rupture.
Though the cold air adds a burden to the heart, this individual is at risk of a soft plaque rupture even in warm weather should he decide one day to engage in strenuous exercise (i.e., a pickup basketball game with the neighborhood teenagers).
The degree of stable/calcified plaque that’s present in the coronary arteries is strongly correlated to the amount of soft plaque present, and is strongly correlated to likelihood of a cardiac event within three years of such a finding.
In other words, if a person at low risk for heart disease has a calcium score of zero, chances are pretty high that this person has very little, if any, soft plaque buildup.
The higher the calcium score, the greater the chances of having soft plaque buildup.
Exercise is great for the heart and helps prevent soft plaque buildup.
The problem is when a sedentary person, especially one with risk factors for heart disease and attack (e.g., high blood pressure, diabetes, abdominal obesity, overall excess body fat, smoking, standard American diet), takes on way too much exercise at once.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Diamond_Images
Survival of Untreated Mild Heart Attack

If you have a mild heart attack but no surgical treatment, how long will you survive?
“The short answer is we don’t know,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
“If we suspect a silent MI (based on ECG, echocardiogram or stress test results), patients are immediately targeted for secondary prevention and are placed on an aggressive regimen including cholesterol lowering medication, aspirin and usually anti-hypertensives.”
I’ve always wondered about this because a man I used to work with in an office one day was absent. I later learned he had a “mild heart attack.”
He was 47 and a few days later was back at work. He had been driving when he felt chest pain and drove himself to the ER.
He’d had no bypass surgery, no stent. The only difference was that he was bringing grapefruits to work and saying how his heart needed the “roughage” of the fruit.
So this begs the question:
If someone has a mild heart attack but no surgical treatment, how long can they be expected to live?
Seems to me that if nothing is done (either surgically or major lifestyle changes), a major heart attack will surely occur.
Dr. Stevens-Cohen explains, “It may have to do with the wording. Sometimes, the blood tests (positive troponins) can be positive, but when you perform an angiogram or a stress test, there is no damage, area of ischemia or significant blockage.”
Troponins are enzymes that damaged heart muscle release, so when someone has a heart attack, these proteins WILL be released and show as elevated in the blood test. Ischemia refers to oxygen supply being cut off.
But back to the “mild heart attack”…
“Some physicians may word this type of event as a mild heart attack (almost comparable to the phrase chemical pregnancy),” says Dr. Stevens-Cohen.
“We see a change in the blood levels but no evidence of pregnancy and then the patient gets their period.
“If we don’t see anything of significance on the angiogram or stress test, a physician may opt for medical management.
“I would assume that a statin and baby aspirin would be indicated and you observe the patient. But lifestyle changes should also be a part of that conversation.
“In order for a CABG [bypass surgery] to be successful, there must be an area on the native coronary vessel that makes for a good target (a good bypass target).
“With diffuse disease, sometimes, there is no target to drop the bypass graft, and evidence shows us these grafts fail.
“Surgeons look at cath images to decide on targets, and if they don’t see a good one, they usually leave the vessel alone.”
One of the greatest things you can do to avoid a major and mild heart attack is to eliminate processed foods. Think this is impossible?
Processed foods are an invention of modern man. What do you think people were eating before canning factories and food manufacturing plants were invented?

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
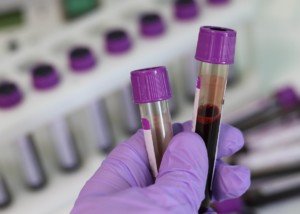
Can a Troponin Level Be Normal After a Heart Attack?

A myocardial infarction is a heart attack. Troponins “leak” from damaged heart tissue and make their way to the bloodstream.
Normally in the absence of a heart attack the levels are very low. A heart attack will substantially spike the levels.
But can there be an exception to this rule?
“No. The definition of a myocardial infarction is myocardial/muscle damage, and that is defined by the presence of troponins in blood,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
If someone has chest pain and an abnormal ECG, but negative troponins, Dr. Stevens-Cohen says that the diagnosis would be unstable angina.
“The management is the same. However, the definition of infarction implies muscle necrosis [death] and we measure that by troponins and CPK levels.”
CPK is an enzyme found in the heart. “The levels usually rise within six hours of presentation and can remain elevated for 1-2 weeks following an event.”
If you go to the emergency room complaining of chest pain or “shortness of breath,” a doctor will order a test to check the level of troponins.
The doctor wants to rule out (or in) a heart attack as quickly as possible, and in fact, the results of this highly sensitive blood test will come back amazingly fast.
However, one test is not enough. If you had a heart attack, that initial blood draw — if done soon enough after the cardiac event–won’t necessarily show an elevation into the heart attack range.
Remember, it takes several hours for the levels to rise.
This is why at least four hours after the first test the doctor will want to have another blood draw taken.
If the patient indeed suffered a heart attack, then for sure, several hours later (it may be four, five or six, depending on the ordering-physician), the troponin level will be elevated into the definitive range for a myocardial infarction.
So maybe five minutes after a heart attack the troponin level is normal, but it won’t be several hours later — it will clearly be elevated enough to show heart muscle damage.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Robert Kneschke
Is Intense Exercise Possible with Clogged Arteries?

If you’ve been diagnosed with heart disease, does this mean that strenuous exercise is off-limits?
Is intense exercise even POSSIBLE with blocked arteries?
First of all, let’s define strenuous exercise. Some people think this is running 10 miles nonstop.
Others see it as deadlifting twice your body weight for five repetitions. There are multiple ways to define “strenuous exercise.”
As a fitness expert, I’ll define it as brief bursts of very intense activity. Thus, deadlifting for an 8-12 rep max, with only one minute of rest in between sets, is quite strenuous.
Dashing up a hill for 15 seconds five times with a three minute slow-walking rest in between each dash is a strenuous workout.
Heavy kettlebell swings that leave you breathing too hard at the end to complete sentences is strenuous exercise.
Can a person who’s been diagnosed with heart disease carry out any of these types of strenuous or very intense exercises?
“This largely depends on how well the coronary artery disease is being managed and other complications associated with CAD,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
CAD stands for coronary artery disease.
Dr. Stevens-Cohen continues, “Important things to note: Is the patient fully revascularized? Does the patient have normal left ventricular systolic function?
If the answer to both of these questions is yes, I would expect the patient to perform strenuous activity with no specific limitations.”
Revascularization refers to a bypass surgery. The heart’s left ventricle pumps or “squeezes” blood into the aorta great blood vessel to be distributed throughout the body. The strength of this pump is referred to as systolic function.
If the contraction to pump out this blood is weak, then there won’t be adequate blood supply throughout the body. So imagine the burden that intense exercise will place on a heart with weak ventricular systolic function.
Though this won’t necessarily damage the heart, the patient simply won’t have enough circulating oxygen to perform intense workouts.
Dr. Stevens-Cohen continues, “Not uncommonly however, we are unable to fully revascularize patients. Sometimes we cannot stent arteries due to vessel size or diffuse nature of coronary artery disease. There are vessels that are not amenable to stenting nor bypass.
“In these situations, we try and optimize with aggressive medical therapy. However, patients may experience angina or anginal equivalents with strenuous activity.”
Angina refers to chest pain. Shortness of breath may also result, though shortness is what will happen even when the fittest person performs strenuous exercise (that which results in considerable fatigue and heavy breathing soon after commencement).
However, the shortness of breath in a person with heart disease may occur during the warmup, making intense levels of exercise impossible.
“If there is significant pump damage (decreased systolic function) following a large infarction [heart attack] or diffuse coronary disease, patients may also be limited by symptoms and unable to engage in strenuous activity,” says Dr. Stevens-Cohen.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.