Will an Unstable Angina Attack at Rest Worsen if You Start Moving?

If you have an attack of unstable angina while at rest, will the pain get worse if you begin engaging in physical activity?
Rest may be in the form of watching TV, standing while doing something passive, soaking in a bathtub, etc., and then suddenly, you have an episode of angina: pain in the chest.
What is unstable angina?
The unstable type is that which occurs while the patient is at rest or even asleep; it’s not predictable. When it decides to come, it will come.
It’s interesting to wonder about the following situation: The pain of unstable angina coming on while the patient is relaxing in a recliner watching TV.
The patient then exits the chair, picks up a vacuum cleaner or a 20 pound crate of books and carries it up a full flight of stairs.
Will the chest pain worsen or is the pain “set” once it occurs?
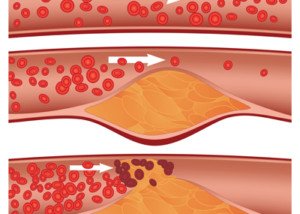
Chest pain from coronary artery disease that occurs at rest is called unstable angina because “it suggests that there is a serious blockage of blood flow to the heart,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“There is not enough blood getting through the blockage even at rest, and this could mean that if anything worsens the situation by increasing demand on the heart or reducing the flow, it could result in a heart attack.
“So, yes, if you are already having chest pain at rest, it will likely get worse with activity and cause the artery to close all the way, causing permanent damage to the heart.”
Persisting with the offending physical exertion will NOT train your heart to be stronger and thus eventually prevent the unstable angina.
Being in denial will not toughen up your coronary arteries.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/fizkes
HOW Sudden Stress Can Cause Fatal Heart Attack or Stroke

When someone says, “You stress me out so much you’re going to give me a heart attack,” maybe they’re onto something.
Ever hear someone say, “All this stress is gonna give me a stroke!”?
David Davies did a study based on a theory that heart attack and stroke can be triggered by a type of hormone that’s released when we are under acute stress.
And of course, we all know that a heart attack can be fatal. So can a stroke. Sometimes the death occurs days or weeks after the event, and other times, that very same day.
This “fight or flee” chemical messenger that Davies looked into is called norepinephrine, a type of catecholamine hormone.
Davies, from Binghamton University, says in his report that a stroke or heart attck often happen after an event in which elevated levels of catecholamine hormones get released into the blood and tissues.
The carotid artery supplies blood to the brain. If a clot forms in this artery and travels to the brain, it can lodge in a blood vessel and block off oxygen to the area of the brain that the vessel feeds: a stroke (ischemic).
If a clot forms in the heart and cuts off oxygen, that’s a heart attack (ischemic).
The clot can be made up of soft arterial plaque, and the clot in this case is often referred to as a “fragment.”
Broken Heart Syndrome — Another Avenue to Consider
Though this name implies that a romantic breakup can harm the heart, that’s not what this term refers to.
“Sudden stress can cause a heart attack due to Takotsubo syndrome or broken heart syndrome,” says Nieca Goldberg, MD, medical director of NYU Women’s Heart Program and radio show host of “Beyond the Heart” on Doctor Radio SiriusXM.
Dr. Goldberg explains, “It this form of heart attack the patient has abnormal heart function and normal arteries. Over time the heart function improves.
“Elderly people [who suffer heart attacks soon after a stressful event] may have underlying heart disease, and this may be due to plaque rupture, but another cause may be Takotsubo syndrome.”
Stress-induced cardiomyopathy – another name for broken heart syndrome – is when the left ventricle in the heart weakens.
This has nothing to do with clogged arteries or plaque fragments obstructing blood flow.
That left ventricle is the heart’s main pumping mechanism. Severe emotional stress – such as that would be experienced by a home invasion, home fire, a car accident or learning tragic news – can literally weaken this pumping chamber.
What causes arterial plaque to rupture in the first place?
Soft plaque is unstable; it can rupture, but what Davies has found is that the rupturing can be triggered by sudden stress.
His team removed diseased carotid arteries from patients, and multiple species of bacteria were isolated and cultured from the walls of these arteries.
These bacteria exist in the form of “biofilms” along the inner arterial walls, and these biofilms were present in every diseased carotid artery in this study.
Under normal circumstances, bacterial biofilms are resistant to antibiotics; the films remain intact. The immune system can’t shake these films, either.
However, something else can: norepinephrine. Norepinephrine delivers a message to the biofilms to break up and release enzymes. These enzymes dissolve the biofilms.
But because the biofilm is in such close proximity to the soft plaque—you guessed it—the soft plaque breaks up, too!
We now have fragments of the soft plaque in the bloodstream, poised to create a blockage of oxygen transport to the brain or heart.
Davies tested his theory by adding norepinephrine to biofilms on the interior walls of silicone tubing.
The amount of this hormone that he added was at a level similar to what a person undergoing extreme stress would have.
At least one species of bacteria, that’s commonly associated with the carotid arteries that were studied, underwent a biofilm disperson response when subjected to norepinephrine, says the paper.
This discovery is new to the world of medical research, so you can anticipate that this will set the stage for bacteria being considered as part of the management of cholesterol levels.
This study, however, does NOT rule out broken heart syndrome as a pathway to emotional stressors leading to a heart attack.
But one thing’s for sure: The more physically fit you are and the more natural is your diet, the lower your risk of suffering from a heart attack in the wake of emotional or physical stressors.
 Dr. Goldberg is senior advisor, Women’s Health Strategy, NYU Langone Health; founder and former medical director, Joan H. Tisch Center for Women’s Health; and clinical associate professor, NYU Grossman School of Medicine.
Dr. Goldberg is senior advisor, Women’s Health Strategy, NYU Langone Health; founder and former medical director, Joan H. Tisch Center for Women’s Health; and clinical associate professor, NYU Grossman School of Medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/photofriday
Source sciencedaily.com/releases/2014/06/140610102010.htm
What Is the Shortest Time Angina Pain in the Chest Can Last ?

So if chest pain lasts under a certain period of time, like really short, would this mean it CAN’T be from angina and thus nothing to worry about?
Or can angina cause sudden but very brief shots of chest pain?
Here’s the answer from a cardiologist to what the shortest duration of time is for angina pain.
“Anginal pain typically lasts at least a few minutes and sometimes as long as hours,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“It lasts as long as the demand on the heart is greater than the supply. That means that the pain usually lasts as long as the activity or stress that is causing it.
“Once a person knows they have angina, they may stop an activity as soon as they feel the pain come on. In that case, it may last only a very brief time like a minute or so. This is not common, however.
“Most brief episodes of chest pain (seconds) are not angina. All chest pain should be reported to your doctor.”
What about unstable angina?
This is when the pain, from insufficient blood flow in the heart, occurs spontaneously—when the person is at rest, under no stress.
This type may even occur in their sleep and awaken them.
How long can unstable angina last?
“Unstable angina means there has been a change in the pattern of your known angina,” says Dr. Denier. “It may be more frequent, last longer than usual or be brought on more easily, sometimes even at rest,” she explains.
“It suggests that there is a serious blockage of one of the coronary arteries. This type of angina may last for hours.”
It wouldn’t be short-lived, “and it would most often be associated with other signs of coronary artery disease such as sweating or nausea or shortness of breath.”
In particular, this kind of angina will be brought on by physical exertion (as will the stable kind) — even something as seemingly innocuous as going up a flight of stairs or quickly pushing a shopping cart across asphalt will usually bring it on.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dan Kosmayer
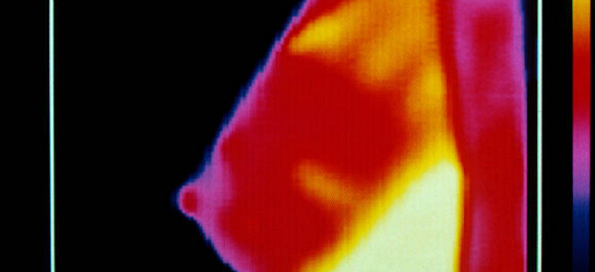
Breast Cancer Thermography: Truth or Hype?
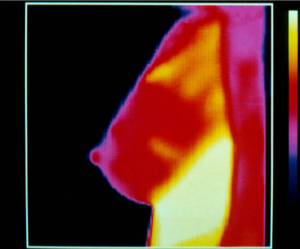
What is REALLY the truth — or hype — about how effective breast thermography is at detecting cancer?
Some claims are that thermography can detect breast cancer years before a mammograph would pick it up.
Is this too good to be true? And if it’s all a lie, how is it that thermography companies are getting away with these claims?
I decided to get a radiologist’s take on this. But to be fair, keep in mind that this article represents the doctor’s perspective.
My job here is to accurately represent Dr. Debora Fineman.
Dr. Fineman is a former diagnostic radiologist with Cancer Treatment Centers of America.
Breast Thermography Claims: Too Good to Be True?
You may have read somewhere that thermography, which does not use radiation, can detect breast cancer years before it actually develops, and that this imaging device does not require the painful compression of the breast, but instead, uses heat.
So it’s fair to wonder just how accurate these reports are and why thermography isn’t a standard screening tool for the detection of breast cancer.
Here is how Dr. Fineman responded to my questions:
I’ll refer you to a position paper from the American College of Radiology, which is the main board determining policies and procedures for radiology including mammography.
The appropriateness criteria from 2012 states, “There is insufficient evidence to support the use of other imaging modalities such as thermography for breast cancer screening.”
The American Cancer Society position on thermography quotes a 2012 research review that found that “Thermography was able to detect only a quarter of the breast cancers found by mammography.
In other words it failed to detect three out of four cancers that were known to be present in the breast. Digital infrared thermal imaging, which some people believe is a newer and better type of thermography, has the same failure rate. This is why thermography should not be used as a substitute for mammograms.”
When I type into the search engine, “Can thermography detect breast cancer that a mammogram misses?” the results indicate that there has been no research on this; that there’s no data.
 Dr. Fineman has been in practice for 30+ years.
Dr. Fineman has been in practice for 30+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Workplace Bullying Leads to Depression

Workplace bullying is a serious problem that can lead to a depressing low mood and/or insomnia.
The recipient depends on their job for income — which throws a real huge kink in the chain.
A study that appears in the journal BMJ Open says that even just witnessing bullying on the job increases the odds that employees will be on drugs for depression, taking prescribed sleeping pills or tranquilizers.
The study participants were between age 40 and 60 and they were part of the Helsinki Health Study.
The association between workplace bullying and the use of prescription psychoactive drugs (for depression, sleep and anxiety) was present for both genders.
A hostile work environment can be incentive enough for people to feel so crummy and “depressed” — not to mention being riddled with anxiety — that they ask their doctor to “prescribe something to help.”
This association of medication usage remained after variables (that could influence the study results) were adjusted for, such as being bullied in childhood.
Is there bullying at your workplace?
“We must distinguish between low mood and brain depression,” says Rupali Chadha, MD, former chief of medical staff at Metropolitan State Hospital in Norwalk, CA.
“If you have major depressive disorder in yourself or even your family, sure, any stressful situation can cause you to fall into a depression (brain type).
“If not, of course, a stressful situation can demoralize you (just plain low mood, not necessarily needing medicine).
“The best way to tell is to see an MD psychiatrist, not a psychologist, to see if this has blossomed into a brain depression — or is low mood treated better with stress management, therapy, yoga … even maybe a new job (or standing up to the bully with HR).”
 In addition to general psychiatry, Dr. Chadha is also a forensic psychiatrist who treats the brain conditions of the criminally insane and serves as an expert witness in trials. She has a passion for fitness plus how the body, mind and spirit come together to build a healthy individual.
In addition to general psychiatry, Dr. Chadha is also a forensic psychiatrist who treats the brain conditions of the criminally insane and serves as an expert witness in trials. She has a passion for fitness plus how the body, mind and spirit come together to build a healthy individual.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com/katemangostar
Source: sciencedaily.com/releases/2012/12/121212205727.htm
Causes of ADHD: Bad Parenting or Brain Wiring?
What more likely leads to ADHD? Parenting methods or innate brain wiring?
If you’ve ever known someone whose child was diagnosed with ADHD, or, if your own child has received this diagnosis, perhaps you’ve often wondered if errors in parenting were mostly responsible, as opposed to just how the child’s brain is naturally hardwired.
“ADHD is a ‘brain wiring’ issue,” says Dr. Divyansu Patel, MD, a psychiatry specialist for 15+ years.
Dr. Patel explains, “It can be genetically inherited, meaning at least one of the parents has had symptoms.”
What if the child seems to have a behavioral issue, such as acting “bratty” in the presence of his or her parents?
What if one of the parents is very lenient, and the other seems to be indifferent, which then creates the illusion of a parenting issue that promotes the hyperactive, impulsive or “rude” behavior?
Dr. Patel points out that in such a case, though the child may have clinical signs of ADHD, that child may also have what is known as oppositional defiant disorder.
Though some people may be tempted to consider this a more technical term for “disobedient child” or a “child whose parents are not consistent with rules,” Dr. Patel explains the following:
“This is a comorbid disorder with ADHD about 40% of the time.
“ODD is more about behavior issues, as it is managed with therapy and then medication.
“Typically, it can originate or be exacerbated when parents are not on the ‘same page’ about parenting.”
ADHD and the Brain
Neuroscientists are looking more towards the miswiring of the brain’s reward system as a potential cause of ADHD, vs. so-called bad parenting.
For instance, study results appear in the journal Neuron.
The researchers from the Mayo Clinic in Florida and Aarhus University in Denmark investigated a type of neuron that regulates pleasure, reward, motivation and cognition.
These dopaminergic neurons are thought to be connected to the development of attention deficit hyperactivity disorder.
SorCS2 is a receptor system that’s responsible for the correct wiring pertaining to the dopaminergic neurons. This occurs during embryonic development.
However, after the brain matures, if there’s a cut in SorCS2, a two-chain receptor results. This two-chain receptor causes cell death.
SorCS2 acts as a molecular switch, say the scientists, between what seems to be opposing effects in proBDNF, a neuronal growth factor.
This growth factor aids in the selection of cells that can most benefit the nervous system, and it also gets rid of the cells that are less beneficial.
This way, a finely tuned network of neurons is established.
Mice that are deficient in SorCS2 lack a response to proBDNF.
The contacts between dopaminergic neurons are dysfunctional.
The paper also notes that numerous other studies have reported that people with ADHD commonly exhibit miswiring in the said brain region.
Think of a single-chain protein that’s the SorCS2: a long chain composed of amino acids.
Now, imagine it gets snipped in two. It now functions differently, leading to damage in the nerves of the peripheral nervous system.
What is ADHD?
“ADHD” is actually a term that describes a number of symptoms or signs.
So if someone “has ADHD,” they have enough of these features to get the diagnosis.
ADHD is also considered a neurodevelopmental disorder that one never outgrows. A first-time diagnosis may even occur in adulthood.
“Typical symptoms include inattention, poor concentration, poor organization, poor attention to detail, forgetful in daily activities,” says Dr. Patel.
“They can also have hyperactivity which is typical in childhood, which can include fidgeting, squirming when seated, difficultly with remaining seated, hard time playing quietly, talking excessively.
“Impulsivity is also a symptom including impatience, a hard time waiting for a turn and interrupting.”
ADHD in the form of atypical brain wiring also comes with perks such as easily adapting to fluctuating schedules and the ability to hyperfocus on a topic that one is passionate about.
 Dr. Patel specializes in child and adolescent psychiatry. He is also well-versed in clinical research, medical education, pediatrics, psychopharmacology and medicine.
Dr. Patel specializes in child and adolescent psychiatry. He is also well-versed in clinical research, medical education, pediatrics, psychopharmacology and medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2014/06/140604123424.htm
Why Can Acute Stress Sometimes Cause Chest Pain?

Here’s a cardiologist’s explanation for how sudden stress can sometimes cause chest pain.
It can feel like a heart attack, especially when you remind yourself that there’ve been cases in which a heart attack indeed was set off by an acute episode of severe stress.
“Acute stress can lead to chest pain by causing the muscles of the chest wall, the back, the neck or the face to contract and tighten, leading to a sensation of pain,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“Acute stress can also raise your blood pressure which can place an increased burden on your heart, causing pain.
“When stress happens suddenly, the body is not prepared for it.
Even a normal response to stress can feel very abnormal.”
Do chest muscles spasm?
“Any muscles can spasm, especially when under stress,” says Dr. Denier. “The chest muscles can do this, causing pain. The diaphragm and the esophagus can also spasm which sometimes mimics heart pain.”
The esophagus’s composition includes striated and smooth muscle, so it definitely has the capacity to spasm.
“Acute stress and release of catecholamines can trigger spasm of the esophagus,” says Dr. Denier.
“Most often, esophageal spasm occurs while someone is eating or drinking something.
“It is more common in women and people with reflux disease or anxiety.
“Sometimes specific foods can trigger it.
“The important thing is that the symptoms can be exactly the same as a heart attack and should always be reported to your doctor.”
To minimize the harmful effect of stress on your heart, you should take up some form of intense exercise at least twice a week.
As for the benign chest pain, strength training and yoga would be a great combination to help keep the musculature less vulnerable to uncomfortable tensing up.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/tommaso79
What Does Chest Pain Only when Breathing Mean?

The good news is that chest pain only when breathing probably doesn’t mean a heart attack, but the real bad news is that it likely means that there is something else wrong with your heart.
Causes of chest pain only when breathing can involve the heart, though this does not necessarily mean a heart attack.
“Chest pain while breathing is called pleuritic chest pain and usually means there is inflammation involving the lining of the lungs and/or the heart,” explains Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
This is not related to a heart attack or clogged coronary arteries.
Dr. Denier continues, “When there is inflammation of the lining of the lung it is called pleurisy. Inflammation of the lining of the heart is called pericarditis.
“Both can follow an innocent upper respiratory infection or viral illness. This type of pain is worse on a deep inhale or with movement or lying flat.
“Both are relieved by anti-inflammatory medications and will go away once the inflammation is gone.”
These are not minor conditions. They DO need prompt medical attention. If you’re experiencing pain in the chest only when you breathe in — and it’s significant pain — get to the emergency room.
A Few More Causes of Chest Pain only While Breathing
Dr. Denier says, “Chest pain with breathing can also be caused by pneumonia which would usually also be accompanied by a cough and a fever.”
Unlike viral pneumonia, bacterial pneumonia doesn’t produce a fever.
However, a family member should never take the sufferer’s word for it that they says they “don’t feel warm.”
Take that person’s temperature yourself even if they insist, “I don’t feel hot.”
“Severe coughing can sometimes lead to a rib fracture which causes considerable pain with breathing,” adds Dr. Denier.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ShotPrime Studio
Which Side Chest Pain More Likely Means Heart Attack, Illness?
A cardiologist explains which side that chest pain is more likely to mean a heart problem or attack.
“Typically, left sided chest pain is more common in patients with angina and/or heart attacks,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“This is because the heart is located slightly more to the left of the chest.
“There are patients who experience right sided chest pain and truly have heart disease.
“This is called referred pain and can travel anywhere like the jaw or the arm.
“Women can have symptoms that are not typical of the usual angina and this includes right sided chest pain.
“Very rarely, we do see people with a heart on the right side of the body! This is why it’s so important to report any chest pain to your doctor.”
Chest pain on the left side of your chest can have benign causes, but you should report anything that concerns you to a cardiologist, with the idea that a cardiac problem can be ruled out.

Heart attack symptoms

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
How Does Sudden Emotional Stress Cause Angina?

Sudden stress or anxiety has a specific way of causing angina or chest pain, even in healthy people.
A person who does not have heart disease (plaque buildup in the coronary arteries) can still experience chest pain as a result of anxiety or stress.
When a person has chest pain from a shortage of oxygen in the heart, caused by clogged arteries, this is called angina.
“Mental stress leads to the release of catecholamines in your body, hormones that help your body to protect itself,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“This is the body’s ‘fight or flight’ mechanism. Catecholamines cause an increase in your heart rate and blood pressure which increases your heart’s need for oxygen.
“Catecholamines can also cause your blood vessels to constrict.
“Sometimes the heart can pump so hard that it cuts off its own blood supply by squeezing the coronary arteries! All of these mechanisms can lead to chest pain.”
Non-angina chest pain from stress can cause chest pain as well.
In this case, muscle tension and shallow breathing, especially in the chest and shoulders, can cause the discomfort in that area.
Prolonged tightening reduces blood flow, causes fatigue and micro-spasms, and sensitizes pain nerves, producing chest wall pain without heart involvement.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.