Are You Scared of a Catheter Coronary Angiogram?

Are you scared to have a catheter angiogram, but need one?
A catheter coronary angiogram is an invasive procedure, and if your doctor recommends you should have one, you may end up too afraid to go through with the procedure — once the risks are outlined to you.
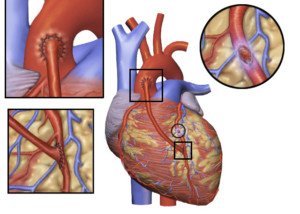
“The definitive test for the diagnosis of coronary artery disease remains cardiac catheterization/angiography,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
“In this test a catheter is guided to the heart, and dye is introduced into the coronary arteries.
“Images can then be obtained to determine the extent and location of any blockages. In many cases, the cardiologist can perform angioplasty and relieve the blockage on the spot.”
My mother was told she should have a catheter coronary angiogram. She was verbally told the risks, then given paperwork detailing the risks.
When she was done reading, she put the papers aside and refused the procedure, wanting to go home (she had been admitted to the cardiac unit after visiting the ER with chest pain).
I insisted she have the catheter coronary angiogram, even though I, too, was quite nervous about the risks.
Risks of a Catheter Angiogram
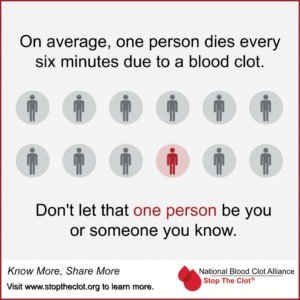
Heart attack, stroke, tear in an artery, blood clots, excessive bleeding, kidney damage and infection. That’s enough to scare away an elephant.
At the same time, I knew that the coronary catheter angiogram would get to the bottom of my mother’s problems.
The procedure would be able to — with 100% accuracy — rule out, or in, blockages in the coronary arteries.
My mother had been experiencing peculiar symptoms for a few months, and especially over the few days preceding the hospital admission.
I was fearful of the coronary catheter angiogram, but more fearful of not finding out what was causing the shortness of breath and chest pain.
How to Put Your Anxiety Over a Catheter Angiogram at Ease
Think about what could happen if you skip this procedure out of fear, and go home … and then a few days later, you feel a large brick pressing down on your chest: a heart attack.
Tell yourself there’s a very good reason your doctor wants you to undergo this procedure.
If you’re having symptoms that fit the bill for coronary artery disease and especially an impending heart attack — and you’ve been repeatedly dismissing these symptoms as yet another panic attack, anxiety attack or acid indigestion — for once and for all, have the coronary catheter angiogram if your cardiologist recommends it.
This procedure is not a standard screening tool and if you don’t present with certain criteria, your doctor will advise against it.
Though the procedure is invasive and carries the frightening risks, the chances of serious complications are actually small.
I’m certainly glad I talked my mother into having the catheter coronary angiogram.
I had told her: “If you go home, you’ll be back to square one and be wondering if something’s wrong with your heart. Just get this procedure done and you will finally have answers, and a treatment plan in place.
“Otherwise, if you skip this and go home, you’ll be empty handed. And what if something really is wrong with your heart? No treatment plan in place, you’re home, heart attack, you’re screwed.”
My Mother’s Cath Angiogram Results
The catheter coronary angiogram revealed extensive blockage in five of my mother’s coronary arteries.
Within two hours of this result, she was in the OR for quintuple bypass surgery. She fully recovered.
 Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/MAD.vertise
CT Abdomen Scan Can Predict Heart Disease and Mortality
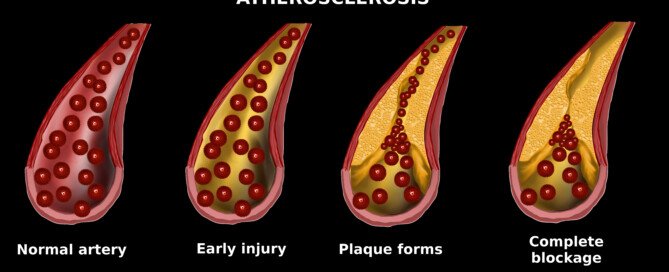
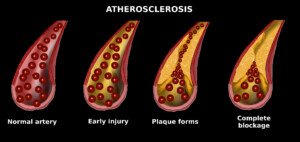
Plaque in your abdomen is a strong clue that there is plaque in your heart: coronary artery disease, or “sludge” in your heart’s arteries.
When a CT abdominal scan shows very high degrees of abdominal aortic calcium, these patients are about 60 percent at risk of having CAD: coronary artery disease.
Plus, the presence of the abdominal aortic calcium (high levels) means a higher risk of death.
Not surprisingly, the absence of abdominal aortic calcium is associated with low risk of the coronary artery disease.
“The typical abdominal CT (whether or not it includes the pelvis) starts above the diaphragm and includes some of the lung base and some of the bottom of the heart,” says Brett Mollard, MD, a board certified diagnostic radiologist who specializes in abdominal imaging and nuclear medicine.
“The coronary arteries are generally at least partially visualized, particularly the right coronary artery, allowing us to see if any atherosclerotic calcifications are present.
“Coronary artery calcifications are used to help risk stratify patients for underlying coronary artery disease.
“While a CT of the abdomen won’t fully assess the coronary arteries, it can tip off an ordering provider to the presence of coronary artery calcifications and lead to further risk stratification and/or a dedicated coronary calcium screening CT.
“Occasionally, incidentally detected coronary calcifications may be the most important finding we make on an abdominal CT.”
Risk Factors for Coronary Artery Disease
- smoking, obesity and overweight (especially the “apple” shaped body)
- high fat diet
- high salt (sodium) diet
- lack of exercise
- emotional stress
- family history
- diabetes
- high blood pressure.
- untreated obstructive sleep apnea
Additional Risk Factors
- chronic sleep habits of less than six hours a night
- chronic sleep habits of more than nine hours a night
- ingestion of trans fats (manmade fat found in many foods)
- insulin resistance (forerunner of type 2 diabetes).
A less invasive but accurate diagnostic tool for coronary artery disease is the CT angiogram.
The CT calcium score is also a highly regarded diagnostic tool.
 Brett Mollard, MD, completed his residency in diagnostic radiology and nuclear medicine at the University of Michigan where he served as Chief Resident. He subsequently completed a fellowship in abdominal imaging at the University of California, San Francisco (UCSF). He currently works in private practice.
Brett Mollard, MD, completed his residency in diagnostic radiology and nuclear medicine at the University of Michigan where he served as Chief Resident. He subsequently completed a fellowship in abdominal imaging at the University of California, San Francisco (UCSF). He currently works in private practice.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Cessna152
Postmenopausal Women: Fast Resting Pulse Linked to Heart Attacks

A fast resting pulse rate in postmenopausal women is correlated to a higher risk of heart attacks and coronary deaths.
But should you allow this study’s unexpected results to scare you into worrying about your heart simply because you’re past menopause and have a fast resting pulse?
What’s startling is that, according to this research, resting pulse rate in the women was able to predict coronary events (heart attack, coronary death) independent of common risk factors for heart attacks, and also independent of the level of physical activity.
Study Summary
For this study (appearing on the British Medical Journal website, 129,135 postmenopausal women were followed.
None of the women had a history of any heart problems. Resting pulse rate can be affected by certain things, such as high cholesterol, high blood pressure, drinking and smoking.
So at the beginning of the study, these items were taken into consideration.
For an average of 7.8 years, the postmenopausal subjects were monitored, and this tracking included any hospital stays that occurred as well as all coronary events.
- During the 7.8 years, the number of heart attacks and coronary deaths totaled 2,281.
- And the number of strokes reached 1,877.
Scary News
Women who had the highest resting pulse (exceeding 76 beats per minute), were substantially more likely to experience a coronary event, than were the women who had the lowest resting pulse (defined as 62 beats or less per minute).
Additional analysis revealed that this correlation (coronary event, not fast pulse) was not influenced by physical activity, or whether or not the subjects had diabetes.
However, the correlation was more pronounced in women who were 50 to 64, than in subjects over age 65. There was no correlation between resting pulse and stroke, however.
Researchers’ Conclusion
Resting heart rate in postmenopausal women independently predicts the occurrence of heart attacks as well as coronary deaths.
Is fast resting pulse as strong a predictor of heart attacks in women, as are smoking and diabetes? No.
But the researchers believe that the association is strong enough to have clinical significance.
What to Do if Postmenopausal and You Have a Fast Resting Heart Rate (76+ bpm)
“While this may be true in that there is some association, I would not advise my patients to excessively worry about their resting heart rate,” says Sendhil Krishnan, MD, a board-certified adult general cardiologist with advanced subspecialty training in interventional cardiology.
“Just being anxious and worrying about something can, in fact, lead to a higher baseline heart rate.
“It was also noted that during this study that physical activity was inversely related to a resting heart rate.
“This is a well-known phenomenon: People who are physically fit and more conditioned tend to have lower heart rates (athletes for example can have resting heart rates 10-20 beats slower than the general population).”
Though the study found that physical activity was not associated with the cardiac events, keep in mind that the faster heart rate WAS.
The study did not specifically explore postmenopausal athletes who had fast resting pulses to see if they had a higher rate of heart attacks.
“Another important thing to realize is that patients who were on medications that can slow the heart rates (beta blockers or digoxin, etc.) were excluded from this trial,” says Dr. Krishnan.
“This information would’ve been helpful because it could suggest that patients with a faster heart rate may be put on a beta blocker just to slow the pulse down. However, we do not have this data to suggest doing this at this time.
“My recommendation for any patient is to continue to do all things necessary to be cardiovascularly fit which includes proper health, exercise, not smoking, maintaining proper cholesterol levels and controlling blood pressure.
“A treadmill exercise stress test will help identify early onset of coronary artery disease and help prevent significant problems down the road.
“It’s also important to realize that a fast heart rate may be secondary to other arrhythmic conditions such as atrial fibrillation which can cause intermittent episodes of tachycardia [rapid heart rate].
“Patients should be screened with at least an EKG or even wear a portable event monitor to catch any arrhythmic events.”
The Questions this Study Begs
#1) What about a study of premenopausal women, resting pulse and heart attacks? That will span a longer period of time, but is worth it.
#2) And what about the cause of the fast resting pulse?
Wouldn’t there be a difference in association with heart attacks, if the fast resting pulse is caused by persistent anxiety in an otherwise healthy super-fit, postmenopausal woman, versus a disease process ?
 Dr. Krishnan is with Pacific Heart & Vascular, where you can view his videos on heart disease and healthy living. He has numerous publications and often speaks at local and regional events.
Dr. Krishnan is with Pacific Heart & Vascular, where you can view his videos on heart disease and healthy living. He has numerous publications and often speaks at local and regional events.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Elena Ray
Source: sciencedaily.com/releases/2009/02/090203192429.htm
Early Menopause, Heart Attack Risk: Thin Fit vs. Obese Women

The research-verdict is out that early menopause appears to double heart attack risk and increase risk of cardiovascular disease.
But does this take into consideration variables of exercise, diet, body weight and smoking history?
The research points out that cardiovascular disease, for which early menopause is a potential risk factor, is the No. 1 killer of American women.
But working hard to improve modifiable risk factors will go a long way at helping to prevent cardiovascular disease. Modifiable risk factors include:
- Dietary habits
- Exercise habits
- Smoking
- Stress management
- Sleep habits
- Blood pressure
- Cholesterol profile
The study had over 2,500 participants of varying races.
The medical definition of early menopause is having completed the process (either naturally or surgically) before a woman’s 46th birthday.
Completion of menopause is when a woman goes 12 months without menstruating, and if this happens before she turns 46, it is “early.”
Surprising News
The researchers had adjusted for modifiable risk factors.
But despite that, early menopause was determined to be an independent risk factor for a higher risk of heart attacks and other cardiac events.
The reason why this is has not been established, as this was an observational study.
Two questions should hang before the savvy health-conscious woman:
Does early menopause increase heart attack risk?
Or, does cardiovascular disease bring on early menopause?
Says Nanette Santoro, MD, Professor and E. Stewart Chair of Obstetrics and Gynecology, University of Colorado at Denver School of Medicine:
“CVD burden may well have a connection to earlier menopause, and there are a few cohort studies that have shown that. This study (Wellons) shows that in a sizable, multi-ethnic cohort – – which is meaningful.”
Question to Ask
Were the early menopause women actually divided into several groups such as 1) never smoked, 2) never were overweight, 3) long history of intense exercise, 4) long history of clean all-natural eating habits?
What would make an intriguing study?
A study in which the heart attack rates of obese early menopause women are compared to the heart attack risks of never-overweight early menopause women, and so on; it’s nearly endless as far as which groups to compose for comparisons:
1) lean, never-smoked, vegetarians
2) obese but who’ve always exercised
3) obese who never smoked
4) obese heavy smokers
5) exercise enthusiasts with low body fat
6) exercise enthusiasts with high body fat
7) exercise enthusiasts with poor stress management and frequent junk food binges.
What to Do in the Meantime
If you’re obese or even moderately overweight, don’t wait till menopause, retirement or some other distant event to start making lifestyle changes to reduce excess body fat.
Two Major Weapons Against Obesity
- Compound strength training
- High intensity interval training
The mistake that many big women make is that of using tiny weights. I’ve seen this time and time again — and it just doesn’t beget the results they’re looking for.

Trade those tiny dumbbells for a heavy barbell for optimal fat loss. Shutterstock/Lisa F. Young
The general rule is that for optimal weight loss, you must use an amount of weight that makes it absolutely impossible to complete more than 12 repetitions.
However, you should be able to perform at least eight reps.
A compound exercise is one in which more than one joint is used.

Preparing to squat, which works the glutes, thighs, hamstrings and core. Shutterstock/Reshetnikov_art
The best compound exercises are the squat, deadlift, leg press, any barbell pressing motion, and pulling movements such as the seated row.
If you’re already in the midst of menopause, or you sense that it’s around the corner, don’t let this stop you from embarking on a serious strength training program.
Not only does strength training benefit the heart, but even more so, high intensity interval training will boost heart health and significantly reduce the risk of cardiovascular disease.
Dr. Santoro has been an active clinician and researcher in reproductive endocrinology beginning in 1986.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Estrada Anton
sscpywrt26
Sources: sciencedaily.com/releases/2010/06/100621133948.htm;
endocrinetoday.com/view.aspx?rid=65730
Why Eating and Swallowing Increase Heart Rate

Ever notice an increase in heart rate when eating or swallowing?
Perhaps you can feel your heart rate increase upon eating or swallowing; or, maybe you accidentally discovered this by happening to take your pulse while eating.
At any rate, there is a distinct reason why heart rate can increase as a result of eating, which includes the act of swallowing. As far as a faster heart rate, eating and swallowing are one and the same.
“Eating and swallowing affect the autonomic nervous system,” says Teresa Caulin-Glaser, MD, a cardiologist and senior vice president with Service Lines, OhioHealth.
“The autonomic nervous system has two arms that can impact the heart rate:
1) the sympathetic system, which increases the heart rate
2) the parasympathetic, that slows the heart rate. When a person is eating and swallowing, the parasympathetic nervous system, specifically the vagus nerve, is inhibited.
“As a result of the inhibition of this nerve when eating and swallowing, there is a temporary increase in a person’s heart rate (by inhibiting the parasympathetic component of the nervous system the heart rate increases).”
So that’s the reason why heart rate increases while you are eating or swallowing.
Not knowing why this occurs can be scary for some people, particularly people who have risk factors for a heart attack, or who’ve had cardiovascular issues in the past.
Rest assured, a faster HR while eating is nothing to worry about. What you should be more concerned with is what you’re eating.
Some food items are harmful to cardiovascular health, such as trans fats, hydrogenated or partially hydrogenated vegetable oils, and saturated fats.
Read ingredients on the back of the packaging, box or can to see if these fats are in the product.
Forget what it says on the front of the package.
“No trans fat” simply means less than a minimal amount of trans fat in the serving size that’s listed on the nutrition label.
This is a manufacturer’s trick.
The real story is in the list of ingredients.
So next time your heart rate speeds up while eating and swallowing, go easy on the red meat and butter, and heavy on the whole grains, vegetables and fruits. And that’s, of course, after you exercised for a full hour.

Dr. Caulin-Glaser is an experienced physician, teacher and researcher in the specialty of cardiovascular disease, and formerly the system vice president for Heart & Vascular Services at OhioHealth.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
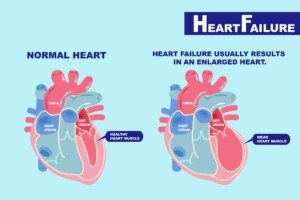
Can Obesity & Overweight Cause Congestive Heart Failure?

When one thinks of obesity’s harm to the heart, it’s usually clogged arteries.
But being fat can impair the heart’s pumping action: heart failure.
- The heart fails to pump the amount of blood it’s supposed to.
- And/or, the heart’s chambers fail to fill up with the amount of blood they’re supposed to before each beat.
“Extra fat around the heart can be dangerous because of the mechanical constriction of the heart muscle,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“If the heart is surrounded by fat, it can’t beat as efficiently, and that can lead to heart arrhythmias or heart failure.”
These days, “congestive” heart failure is becoming increasingly referred to as chronic heart failure, since not all patients with this common disease suffer from congested fluid in the body.
Being Fat Is As Much a Risk for CHF As It Is for Heart Attack or Stroke

Shutterstock/nger Anne Hulbækdal
Exactly how obesity creates a risk factor for congestive heart failure is not clearly understood.
Researchers believe the mechanism may be an indirect effect, in that all the extra internal fat often leads to high blood pressure, heart attack or type 2 diabetes … which all put a person at risk for CHF.
However, some researchers indeed believe that obesity has a direct effect on heart muscle.
Shutterstock/EstherQueen999
Thin people get CHF too, but you must realize that CHF has multiple risk factors. One is obesity.
Others are lack of exercise, smoking, untreated sleep apnea, and of course, high blood pressure, heart attack and diabetes.
The mechanical problem that’s created by the excess fat surrounding the heart may not be the only pathway that leads to CHF in the very overweight person.
Fat cells may behave as endocrine tissue, secreting harmful substances.
Weight Affects Heart Function
A study by Thomas H. Marwick, PhD, compared the left ventricles of normal-weight people, with the left ventricles of severely obese people.

Shutterstock/ Motortion Films
In the overweight participants, there was a very weakened ability of cardiac muscle to contract, and a diminished ability of cardiac muscle to fully relax.
The full-relax is important for enabling the ventricle to be refilled with blood during rest periods between the heartbeats.
The study showed impairments of left ventricular function in mildly obese, as well as overweight, subjects.
“The study showed a direct relationship between the level of obesity and the degree of myocardial dysfunction,” says Dr. Marwick in the paper.
And this finding was independent of other risk factors.
“We think this indicates a direct metabolic effect of obesity on the heart muscle,” says Dr. Marwick.
More than half a million cases are diagnosed in the U.S. every year, and the condition kills about 53,000 Americans yearly, as primary cause of death.
However, if congestive or chronic heart failure was named on death certificates as contributing cause of death, the annual death rate would jump to over 260,000.
Congestive failure usually starts in the left ventricle, and may be diagnosed as diminished left ventricular function.
Regular exercise (strength training and cardio) plus prevention of obesity and even overweight, will go a dynamically long way in preventing congestive or chronic heart failure.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Motortion Films
Source: sciencedaily.com/releases/2004/11/041108013816.htm
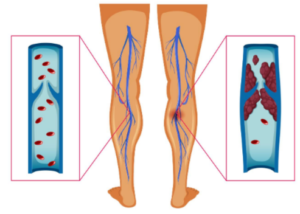
Does DVT Risk Increase with a Cast or Splint?

Wondering if your risk of deep vein thrombosis goes up if you must wear a cast or a splint?
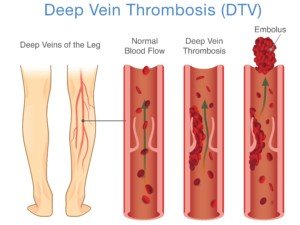
“Any kind of immobility, which slows down the blood flow in the legs, will increase the risk of DVT,” says Dr. Paramjit “Romi” Chopra, MD, founder of the Midwest Institute for Minimally Invasive Therapies (MIMIT), an interventional radiology and endovascular therapy practice.
“When we walk, our calf muscles act as pumps to work against gravity and pump blood from the legs back to the heart,” explains Dr. Chopra.
The German Institute for Quality and Efficiency in Health Care (IQWiG) conducted a study on young athletes — who, by the way, are not immune from a deep vein thrombosis.
Young athletes with a cast or splint are at increased risk for deep vein thrombosis, especially if they’re sitting for extended periods on a bus or airplane traveling with their team.
After all, the cast or splint forces a considerable degree of immobilization, even if the cast only goes from the ankle to below the knee for a broken ankle.
The limited movement from the leg, due to the cast or splint, can also increase risk of deep vein thrombosis forming in the pelvis.
What Should You Do?
So if you end up with a cast or splint on your leg or a portion of your leg, what should you do, to minimize developing a deep vein thrombosis?
Get back on your feet and move around as soon as possible. Of course, this is easier said than done when you have an injury.
The next defense is medication: anticoagulant drugs, also known as blood thinners, which reduce clotting ability in the blood.
Blood thinners do not bust up the clot (that’s another class of drugs known as “clot busting” or thrombolytic drugs).
But they can prevent pre-existing clots from getting bigger, and of course, blood thinners go a long way in preventing the formation of new deep vein thromboses.
Ditch the Cigarettes + Other Preventive Measures
Another way to reduce the risk of deep vein thrombosis while you’re stuck in a cast or splint is to quit smoking if you’re a smoker.
Next, if you have high blood pressure, get it under control asap.
Ask your orthopedic or sports medicine physician to recommend some exercises you can do with the leg that has the cast or splint.
For instance, if only the lower part of your leg is in the contraption, you can do quite a bit of exercising with that leg.
- For example, get on all fours.
- Bring the knee of the affected leg towards your chest, then extend the entire leg out straight behind you.
- Bring the knee back in, and so on, for 10-20 repetitions. Switch legs.

Freepik, yanalya
Another exercise is to be on all fours but extend the leg out to the side.
If the entire leg is in a cast, lie on your back and lift the leg up and down (if your doctor clears you for this).
Or, while standing on your good leg, swing the casted leg from the hip, or make circles with it.
Do these exercises every so often to reduce the risk of deep vein thrombosis.
Dr. Chopra combines his Eastern roots and 30+ years’ Western experience to unify the best of both worlds at MIMIT to treat venous disease, peripheral artery disease and musculoskeletal disease.
combines his Eastern roots and 30+ years’ Western experience to unify the best of both worlds at MIMIT to treat venous disease, peripheral artery disease and musculoskeletal disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sources: sciencedaily.com/releases/2009/07/090723113523.htm; mayoclinic.com/health/deep-vein-thrombosis/DS01005/DSECTION=treatments-and-drugs
sscpywrt26
Do ALL Pulmonary Embolisms Come from a DVT?
The common-held belief among physicians is that pulmonary embolism is always from a DVT, a blood clot that forms in the legs or pelvis.
The DVT may break away and end up in a lung, causing the potential to kill a person.
The belief, then, has been that pulmonary embolism and deep vein thrombosis should coexist in the majority of patients, since, allegedly, only part of the blood clot in the leg breaks away, rather than the entire clot.
A report in Archives of Surgery says something very interesting.
The report concerns a study involving 247 trauma patients who had scans done of their lungs, legs and pelvis.
Forty-six of these patients had pulmonary embolus. And 18 percent had deep vein thrombosis.
However, seven of the patients had both pulmonary embolus and deep vein thrombosis.
Were there differences between patients with pulmonary embolus plus deep vein thrombosis, and patients with PE without deep vein thrombosis? No.
The study authors concluded that there is little evidence that pulmonary emboli always come from a DVT of the peripheral veins.
Cadaver studies have shown that usually, only part of the blood clot dislodges and travels elsewhere. The study authors further state that many pulmonary emboli indeed form in the lungs.
Where are all the places in the body a deep vein thrombosis may form?
“DVT is the general term, meaning a thrombus in any deep vein including the veins in the lungs,” says Steve Elias, MD, FACS, a vein specialist with Englewood Health in NJ.
Shutterstock/solar22
“DVT in the legs is the most likely source, but DVTs in unusual places such as the lung, ovarian veins, veins in the brain, etc., should make the doctor more suspicious for an underlying cause: cancer, clotting problems.”
Every year in the U.S., 100,000 to 180,000 people die from a pulmonary embolism.
Every year, 600,000 Americans are hospitalized for a pulmonary embolism!
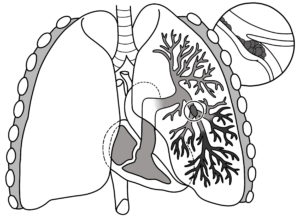
Pulmonary embolism
Symptoms include sharp pain in the chest, difficulty breathing, shortness of breath and coughing up blood.
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sources:
sciencedaily.com/releases/2009/10/091019172329.htm
sciencedaily.com/releases/2011/03/110305105233.htm
DVT from Air Travel: Truth or Hype?

Is deep vein thrombosis from air travel exaggerated?
DVT from long air travel times is not likely in healthy people, says the German Institute for Quality and Efficiency in Health Care (IQWiG).
The IQWiG reveals some intriguing findings, based on analysis of millions of air travelers.
For people on a flight longer than six to eight hours, only two to five, out of every 10,000 travelers, developed a deep vein thrombosis that resulted in symptoms.
What about flights under 4-6 hours? The researches uncovered no convincing evidence that flights under this time frame put people at increased risk for deep vein thrombosis.
Nevertheless, nobody knows if they’ll be that two to five out of 10,000, so to lower risk of deep vein thrombosis, the researchers say to wear compression stockings – but put them on at least two hours prior to your flight, and they should stay on during the whole flight.
What if You’re not so Healthy and Have Risk Factors for DVT?
Though there may be a little hype relative to healthy fit air travelers, it’s certainly not a case of overreaction for flyers with DVT risk factors:
- Smoking
- Obesity
- Old age
- Lack of exercise
- Sedentary lifestyle
- Recent joint replacement or abdominal surgery
- Pregnancy
- Family history of blood clots
“DVT is the occurrence of blood clots forming in the venous system, usually the lower extremities,” says Morton Tavel, MD, Clinical Professor Emeritus of Medicine, Indiana University School of Medicine, and author of “Health Tips, Myths and Tricks: A Physician’s Advice.”
“Such clots are fairly common [while on the ground] and most often are produced by slowing the venous blood flow in these extremities, which can occur in a variety of situations such as sitting for prolonged periods, as can occur during a long air flight,” explains Dr. Tavel.
“Although clotting is unusual even under this circumstance, it can be avoided by frequent moving of the legs, flexing of the leg muscles and walking about.
“The main danger presented by these clots is their breaking away from the veins of origin to be carried by normal blood flow to the lungs, where they can suddenly block flow to portions of the lungs, a process called pulmonary embolus or PE.
“If the blocked artery is sufficiently large, it may cause serious damage and even death.”
Precautions Against DVT Are Easy
If you’re on a long airline flight, make a point of moving your legs periodically — whether you’re as fit as a fiddle or have health ailments.
Stretch your legs out if you can. If you’re cramped, then knock them together; go up and down on your toes; and lift your legs at the hip area (flex the hips).
But the best way to keep blood circulating efficiently, so that it doesn’t clump together and form a deep vein thrombosis, is to just get out of your set and walk up and down the airplane’s cabin.
Even if you don’t have symptoms of a DVT (cramp, pain, swelling, warmth or redness in a leg), you should get up at least every hour.
After all, about half of deep vein thromboses don’t cause symptoms.

Dr. Tavel’s medical research includes over 125 publications, editorials and book reviews in peer-reviewed national medical journals. He was formerly director of the cardiac rehabilitation program at St. Vincent Hospital in Indiana. mortontavel.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: sciencedaily.com/releases/2009/07/090723113523.htm
Which Is Better for CABG: Radial Artery or Saphenous Vein?
What’s better for coronary bypass surgery: a vein from your leg or an artery from your arm?
In coronary bypass surgery (aka CABG), the saphenous vein from the leg is typically used for the grafting procedure.
“Radial artery has been championed as a bypass conduit two or three times during my 20+ years of practice, and then falls out of favor due to graft closure or spasm,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“As the medications have improved to prevent spasm, again — the radial artery is making a small comeback,” continues Dr. Fiocco.
“This artery is only used as a graft to arteries with 90-100% narrowing; anything less and graft closure incidence increases.
“Comparing to saphenous veins is difficult due to variations in vein quality (is the vein dilated, are there varicosities, or is it pristine?).
“The radial artery can be an excellent conduit in the right circumstances, but overall is likely equivalent to a good quality saphenous vein.”
Coronary artery bypass grafting is the most common surgical procedure in the United States.
Study Pitting Radial Artery Against Saphenous Vein for CABG
A study shows that the radial artery from the forearm, wrist and hand, when compared with the saphenous vein, does not result in a better outcome as far as angiographic patency (open, unobstructed graft).
It has been believed that grafts from arteries are better conduits than grafts of the saphenous vein, because grafts from the left internal mammary artery have worked well for bypassing the heart’s left anterior descending artery.
It’s estimated that around six percent of CABG patients receive radial artery grafts.
For this study, over 700 patients were involved, who underwent elective coronary bypass surgery.
The one-year angiographic patency of the saphenous veins and radial artery grafts were compared in the patients.
The investigation was headed by Steven Goldman, MD, of the Southern Arizona VA Health Care System and the University of Arizona Sarver Heart Center.
For the left anterior descending artery, the left internal mammary artery was the graft of choice.
Remaining arteries that needed to be bypassed received either the radial arterial grafting or the saphenous vein graft.
At the post-CABG one-year mark, the angiographic patency was measured.
Was there any significant difference in the one-year graft patency between the saphenous group and the radial artery group? No.
There also wasn’t any difference, when comparing the two groups, regarding adverse events.
Here is what the study authors write: “Although most clinicians assume that compared with vein grafts, arterial grafts have an improved patency rate, there are little multi-institutional prospective data on radial artery graft vs. saphenous vein graft patency.”
If you have a coronary bypass surgery scheduled, do not hesitate to meet with your surgeon and ask questions.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.