Do You Have Chest Pain in Different POSITIONS?

Positional chest pain can be due to a variety of causes including heart problems, says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
Positional chest pain isn’t always caused by acid reflux or costochondritis.
“Typically, chest pain associated with deep inspiration [inhaling] or lying flat may be indicative of pericarditis or an inflammation in the lining of the heart,” says Dr. Stevens-Cohen.
“Patients usually get relief with sitting up or forward. The sitting forward allows the lining of the heart (layers) to separate and provides relief.”
The esophagus is right behind the sternum. “Esophageal spasms or GERD may be some GI reasons for having positional chest pain,” continues Dr. Stevens-Cohen. “GERD may increase at night and cause pain.”
Avoid eating fewer than three hours before bedtime to see if this relieves GERD (acid reflux) related chest pain.
“Musculoskeletal (chondritis) is also positional and can be reproduced by touching the affected area.”
This kind of chest pain (also called costochondritis) can hurt quite a bit and can be caused by lifting weights.
“Pleurisy-inflammation in the lining of the lung can also cause positional pain. Localized inflammation.” This worsens with coughing and inhaling.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/New Africa
Heart Palpitations Lasting Daily, Sometimes Hours
What’s going on when heart palpitations persist for hours almost every day?
“Some people use the word [palpitations] to describe a fast or rapid heart rate; others to note an irregular heart rate,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
“Non-cardiac causes may include thyroid disease, anxiety, hormonal imbalance, high blood pressure, pulmonary issues, GERD/reflux.”
I’ll confess that I once felt heart palpitations within seconds after beginning to read an article about…none other than heart palpitations.
The power of suggestion can be very powerful. After I realized how crazy this was, the symptom vanished.
I also experienced that attention-getting thumping heartbeat when I logged onto my e-mail and saw a message from someone — a message I was expecting — and I knew that the news might be very terrible (turned out it wasn’t).
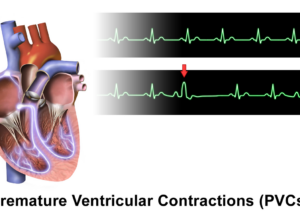
But while I was waiting for the message to open…my heart was just thumping in a PVC type of way.
I don’t mean racing due to adrenaline…but what actually felt like palpitations from PVCs. Both of these incidents were extremely transient and precipitated by anxiety.
Dr. Stevens-Cohen further explains, “If symptoms persists or occur daily, or if they interfere with daily activities including exercise regimen, it’s time to see a physician and be referred to a cardiologist.
“There are some conditions — valvular heart disease (mitral valve prolapse or mitral stenosis) that are associated with palpitations.
“The most important diagnostic tests utilized are an echocardiogram (looking for structural heart disease) and an event or Holter monitor.
“The key is to catch the palpitations on a monitor so we can know if rhythm is dangerous or warrants further treatment.”
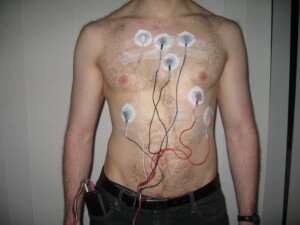
Holter monitor. Jason7825/en.wikipedia
A normal echocardiogram means that the palpitations you feel are benign.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Ejection Fraction 20%: How Long Can You Live?

An ejection fraction of under 20 percent is frightfully low as far as survival…or is it?
“Having a low ejection fraction (absolute number) is not necessarily correlated to symptoms,” begins Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
“For example, a person with an ejection fraction of 40 may be more symptomatic than one with an ejection fraction of 15.
“However, having systolic heart failure with an ejection fraction < 35, there is an increased mortality related to poor cardiac output and arrhythmias.
“Medication and ICD therapy when indicated may help manage symptoms and prevent arrhythmias; however, the mortality is still high.”
ICD stands for implantable cardioverter defibrillator.
“The biggest correlation with heart failure deaths is related to hospital admissions and renal failure/injury.
“Patients with renal failure and more than three hospitalizations in one year may have a mortality rate (one year) of >50 percent.”

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Rocketclips, Inc.
Can CoQ10 Help PVC’s?

CoQ10 is one of the best antioxidant supplements, but how does it work against PVCs: premature ventricular contractions?
For this article I asked Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
This is what Dr. Stevens-Cohen explains:
“Coenzyme Q is a powerful antioxidant that improves oxygen utilization.
“It may help with high blood pressure but has also been reported as causing palpitations. By itself, it is not a known treatment for palpitations.”
PVCs, though frightening, are often just benign premature beats that make it seem as though your heart is skipping a beat or inserting an extra beat.
If you’re worried, see a cardiologist, who will probably order an echocardiogram and will also have you undergo an EKG.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/OBprod
What Does Frequent Nausea with IBS Mean?

It is no secret that irritable bowel syndrome (IBS) can lead to nausea, but what should a sufferer do?
In fact, nausea that’s caused by irritable bowel syndrome isn’t even uncommon, says a doctor.
*****
“IBS is a condition that affects the function of both the upper and lower GI tract, so it would not be uncommon to see nausea, bloating or other upper GI symptoms with IBS, as they can all be related to abnormal gastrointestinal function,” explains Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“That being said, there are many problems that cause nausea, so while this can be seen with IBS, it is important not to get ‘tunnel vision’ and not consider other possibilities.”
This is especially true if you’re over age 50. Even 40. But even in younger people, unexplained nausea or stomach aches, constipation and/or diarrhea, need to be evaluated by a gastroenterologist.
Sometimes, nothing comes up in the test results. IBS is a diagnosis of exclusion, and if the patient then undergoes treatment for this disorder, and the nausea and other symptoms subside, then the diagnosis was likely very accurate.
If you’re having unexplained nausea and have been diagnosed with IBS, but the symptoms persist despite treatment…and especially if the symptoms are becoming progressive in some way and you’re a woman…then see a gynecologist about having your ovaries checked.
Ovarian and other gynecological conditions can cause symptoms that seem like they are digestive in origin.
Remember, cancer (which can cause nausea) can occur alongside IBS, though there is no causal relationship.
Another Condition Similar to IBS; Can Sometimes Cause Nausea
The benign condition of microscopic colitis is sometimes misdiagnosed as IBS.
However, in microscopic colitis, there is no constipation; it’s all diarrhea–and usually watery and “explosive.”
But there may be nausea and painful cramps, too. Only a colonoscopy can diagnose microscopic colitis.
If you’ve been diagnosed with IBS, have not had a colonoscopy, sometimes have nausea, and suffer only from diarrhea — there IS a chance you might actually have microscopic colitis.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/KDdesignphoto
Can IBS Cause Severe Backaches and What’s the Remedy ?

Just what causes that backache from your irritable bowel syndrome?
Back pain is perhaps the world’s leading nonfatal health problem.
It affects millions of people, causing significant discomfort and impacting daily life.
The causes can range from poor posture to injury or chronic conditions — to a simple pulled muscle to PMS to fibromyalgia to multiple sclerosis to a pinched nerve to cancer metastases involving the spine.
That last cause, as scary as that is, is not at the top of the list for common causes of back pain.
Irritable Bowel Syndrome’s Connection to Back Pain
- The question isn’t if IBS can cause backache.
- The question is just how does this happen, and what can be done to remedy it?
“Colitic pain (usually crampy pain relieved by having a bowel movement or passing gas) can often be felt in the back,” explains Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“This represents a phenomenon called referred pain, and reflects the innervation of your colon.
“In short, it is how you are wired together. You treat the back pain by treating the IBS.”
Before you attribute your back pain to IBS, first make sure that you have IBS.
Don’t assume it just because other family members were diagnosed and/or your symptoms are a perfect match to this condition.
IBS is a diagnosis of exclusion, meaning, there is no test for this disorder. It is diagnosed when all other tests are negative.
This includes a colonoscopy. Even young adults with IBS-like symptoms should still undergo a colonoscopy to rule out other causes for the bloating, cramping, diarrhea, constipation and back pain.
A benign inflammatory bowel disease called microscopic colitis causes symptoms very similar to that of irritable bowel syndrome.
This includes back pain in a small percentage of MC patients!
Treatment of MC differs from that for IBS. This is why a colonoscopy is so important.
This procedure can also detect other conditions that can cause symptoms that mimic those of IBS that also cause back pain. Colon cancer, however, is very rare in people under 40.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com jcomp
Is Burping a Symptom of IBS?
A GI physician addresses the question of burping being caused by irritable bowel syndrome.
- Have you been diagnosed with IBS?
- Do you find that you’ve been burping a lot more lately and it seems to be related to your IBS?
It probably is.
“Burping is a not-uncommon symptom in patients with functional gastrointestinal disorders,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“It is usually related to problems with the way your stomach empties. We all swallow air, and usually passes through the GI tract and comes out the way air normally comes out.
“In situations where your stomach does not empty normally, air does not travel the way it normally does; your stomach may get distended, and since it cannot travel and be expelled from below, it comes out from above.”
And hence, you burp.
IBS is a functional disorder of the gastrointestinal tract, and to date, no cause has been defined.
This disorder involves symptoms without detectable structural abnormalities or chemical deviations.
This is why it’s a diagnosis of exclusion, which means the patient must undergo a colonoscopy, among many other tests, before getting a truly valid diagnosis of IBS.
Despite extensive research, no single definitive cause has been identified.
Instead, IBS is believed to result from a combination of factors, such as gut-brain communication issues, changes in gut motility, sensitivity, microbiome imbalances and even mental stress.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Vladimir Gjorgiev
Can IBS Cause Joint Pain? Are There Solutions?

Find out what may actually be going on if you’re having joint pains and have been diagnosed with IBS.
“IBS as a rule does not directly cause joint pains, such as with Crohn’s disease or ulcerative colitis,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“If they do occur they may be from an unrelated issue or may indicate that there may be some other issue going on.”
First off, IBS is not an inflammatory bowel disease. It’s not an autoimmune disease, either.
In fact, irritable bowel syndrome is actually a collection of symptoms.
If you’re having joint aches or “pain” that seem to correlate with your IBS attacks or episodes … it’s possible that these joint aches are connected to your gastrointestinal problem — but this would have to mean that you’ve been misdiagnosed as having IBS!
As mentioned, Crohn’s and ulcerative colitis can cause joint aches or pain. Both these conditions are inflammatory bowel diseases.
However…it’s not likely that Crohn’s or ulcerative colitis will be misdiagnosed as IBS.
There’s another inflammatory bowel disease, that can cause joint aches, that is often misdiagnosed as IBS: microscopic colitis.
There’s symptom overlap. However, the diagnosis for microscopic colitis can be made with 100 percent conclusion: a biopsy of a tissue sample taken from the colon during a colonoscopy.
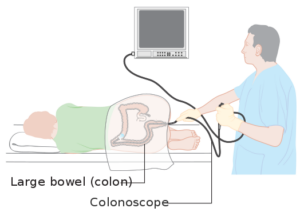
Colonoscopy. Cancer Research UK
The problem is that sometimes, the diagnosis of irritable bowel syndrome is made when there’s been no colonoscopy.
This misdiagnosis is far more likely to occur in a younger person, since GI symptoms in young people aren’t as alarming as they are in those over 40 and especially 50.
When I had my first flare-up of microscopic colitis…as I was being prepped for my colonoscopy…the nurse wasted no time telling me that the diarrhea could be from IBS.
- People with non-retractable IBS may actually have microscopic colitis.
- The treatment for IBS will not work on microscopic colitis.
Microscopic colitis causes joint aches in a small percentage of those diagnosed. I’m one of them.
The joint aches are identical to those that women get with PMS. (Search this site for more information on the joint aches of microscopic colitis, also referred to as enteropathic arthropathy).
If you’ve been diagnosed with IBS, have not had a colonoscopy, and have joint aches that your doctor has said are not rheumatic, you should have a colonoscopy to see if you have microscopic colitis.
And by the way, the joint aches or enteropathic arthropathy from microscopic colitis are benign and transient.
Let them run their annoying course and you’ll soon be back at rock climbing, CrossFit, trail running, power lifting, or whatever your physical passion is.
The joint aches are caused by hormones called prostaglandins, not any degeneration in the joint itself.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/fizkes
Can IBS Cause Hot Flashes?

If IBS causes hot flashes, how on earth does this occur?
IBS stands for irritable bowel syndrome. It is common. So are hot flashes.
Can hot flashes be caused by irritable bowel syndrome?
Yes, says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“This is not uncommon at all. Many people with IBS attacks feel flushed, warm, clammy and can feel as if they have to pass out.
“This has to do with the nervous system supply to your gastrointestinal tract.
“Part of what governs the function of your GI tract is related to your autonomic nervous system, that part of your nervous system that works without your thinking about it.
“One part of this system is called your parasympathetic nervous system, most notably your vagus nerve, and in many patients with IBS, this often becomes very active.
“When it does, it may give the sensation of hot flashes, as well as the other symptoms mentioned above.
“Many patients with IBS feel that they may be running a fever when it often just is related to a feeling of warmth and clamminess one sees with this phenomenon.
“Most people actually running a fever usually feel cold, and may have chills, rather than feeling warm.”
This sensation of cold is largely due to how your body’s thermostat, the hypothalamus, responds to illness or infection.
Also during a fever your body may reduce blood flow to the skin and extremities to keep heat concentrated in the core of your body.
This narrowing of blood vessels near the skin’s surface helps increase your internal temperature, but can leave your extremities feeling cold.
If you can’t tell if you’re having a hot flash or if you might have a fever, you can take your temperature with an instrument — that you can get at a drugstore or online — that very quickly yields your temperature.
It’s also possible that you can be having a hot flash and a fever at the same time, with each situation having different and unrelated causes.
Unlike a fever, though, a menopausal or postmenopausal hot flash may be preceded by a brief migraine or a strange feeling of offness, anxiety or depression that subsides as the body begins feeling hot.
At any rate, IBS can definitely generate a hot flash.
But if you’re going through menopause or have been having true postmenopausal hot flashes, irritable bowel syndrome is likely not the cause of any of these episodes.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/YAKOBCHUK VIACHESLAV
Can Chest Pain Be Caused by IBS?

Is it possible to tell the difference between IBS chest pain and that caused by a heart problem?
Having chest pain, especially in the middle of the night, is scary as heck. It makes a lot of people wonder if they’re having a heart attack.
“IBS is a disorder that can affect the entire gastrointestinal tract, including the esophagus,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“If there is spasm or abnormal function in the esophagus, one can complain of chest pain, trouble swallowing, belching or other symptoms.”
The esophagus is behind the sternum (breastbone), so if your IBS involves esophageal spasms…you will feel discomfort or pain sub-sternally.
However, this is the same location that cardiac-related pain can manifest.
An esophageal spasm can be painful and sudden.
The chest pain from this can mimic the sensation of a heart attack.
These spasms occur when the muscles in the esophagus contract abnormally or irregularly, disrupting the normal movement of food toward the stomach.
The pain may even radiate to the back or arms.
You can’t assume that your chest pain is from IBS or not, or a cardiac problem or not, until you undergo thorough medical testing.
“Keep in mind that it is very important to exclude other causes of chest pain, including most notably, cardiac causes, prior to attributing a symptom to IBS,” says Dr. Blume.
“Sometime one can make that determination clinically, but often it may require diagnostic testing to make sure that there is nothing more serious causing this symptom.”
IBS Chest Pain vs. Cardiac Chest Pain
Is it possible for a person to experience episodes of chest pain that are sometimes from IBS and…sometimes from a cardiac problem like angina? Yes! Why not?
There’s no reason why someone can’t just by chance happen to suffer from both a gastroenterological condition and a cardiac condition.
So even if your troubling chest pain has been determined to be IBS, it would be a very smart move to undergo a thorough exam by a cardiologist — just to be as sure as possible.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.