Can Torn Rotator Cuff Be Remedied With Exercise Therapy Alone?

Diagnosed with a torn rotator cuff?
Have you been told that the only solution for torn rotator cuff is surgery?
When the rotator cuff is “torn,” this means that some tendon tissue has been separated, or pulled away from, the bone to which it’s supposed to be attached. Tendons join muscles to bone.
“The shoulder is a ball and socket joint,” says Edmond Cleeman, MD, a board certified orthopedic surgeon who specializes in sports medicine and arthroscopic surgery of the shoulder, knee and hip.
“There are four tendons that move the shoulder and they are called the rotator cuff tendons.
“Covering the entire rotator cuff is a bursa, a paper-thin fluid sac that helps gliding occur with less friction between surfaces.”
Does a torn rotator cuff automatically mean surgery?
“Rotator cuff tendon tears do not heal on their own and this has been verified with scientific study.
The tendon is attached to bone and when it tears it is pulled away from the insertion site by the muscle, like a rubber band snapping back.
“The only way for the tendon to heal is to pull it back to the bone insertion site and sew it to the bone.
“This procedure is customarily performed arthroscopically (minimal invasive surgery), with a regional anesthetic (the arm is numbed), and the patient goes home the same day.
“Success rates are high in small tears but success diminishes with increasing tear size.”
Rotator cuff problems are extremely common, and not just in athletes who do a lot of throwing or overhead movements.
People who don’t exercise are also vulnerable to rotator cuff injuries, particularly degeneration.
“Scientific study has demonstrated that rotator cuff tendon tears, if left unfixed, will increase in size,” says Dr. Cleeman, founding member of TRIARQ, a community of orthopedists and physical therapists.
“Eventually the tear will become large or massive and the results for surgical repair will diminish. Some tears will no longer be fixable.
“This is because the muscle attached to the torn tendon atrophies, contracts and essentially melts away.”
If the tear is partial or very small, this might be treatable without surgery; physical therapy would be the cornerstone of healing.
“But in these scenarios vigilant watch over the rotator cuff tendon tear with repeat MRI is a must. If the tear starts expanding then surgical repair is recommended.”
If the rotator cuff tear becomes too big, surgical repair may not be possible.
“The results after surgery for massive tears is significantly lower than small tears.
“The likelihood of being able to repair this tear is low because of the atrophy changes in the muscle and tendon.
“Non-surgical treatment starts by avoiding activities that cause pain and aggravate the rotator cuff tendons. These are mostly strength activities with the arm over shoulder height.”
 Dr. Cleeman is a highly experienced orthopedic surgeon and sports medicine specialist at Manhattan Orthopedics. He is committed to performing advanced minimally invasive procedures, allowing his patients to go home the same day.
Dr. Cleeman is a highly experienced orthopedic surgeon and sports medicine specialist at Manhattan Orthopedics. He is committed to performing advanced minimally invasive procedures, allowing his patients to go home the same day.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/KDdesignphoto
Best Exercises for Older Knee Replacement Patients

If you’re 65 years or older and have had total knee replacement surgery, you’ll need to know what the best exercises are for recuperation as well as maintenance.
For older people, as well as younger, having knee replacement surgery, there are exercises they should do for the rest of their life, to maintain optimal functioning of the knee replacement.
There are range of motion exercises, as well as strength-building exercises.
For range of motion exercises, “place a towel under ankle and this allows for a passive stretch” for knee extension,” says Edmond Cleeman, MD, a board certified orthopedic surgeon who specializes in sports medicine and arthroscopic surgery of the shoulder, knee and hip.
This can be done lying down. Place the towel under the foot, holding equal parts of the towel in each hand, and gently pull your straight leg towards you while lying.
It’s okay if the leg is a little bent; not everyone is flexible enough to keep their leg straight.
Another stretching exercise for the knee replacement patient is “Flexion: sit in a chair with foot supported on the floor. Patient actively bends knee,” says Dr. Cleeman.
“You are quickly trained to transfer (i.e., lying to sitting, sitting to standing), then progress to gait training (with assistive device), stair training, and eventually work up to the stationary bike.”
The knee replacement patient will also need to work on quadriceps (front thigh muscles) strength by doing straight leg raises from a standing or lying position, one leg at a time.
On a continued basis, the knee replacement patient should do low impact activities like “walking, swimming and cycling,” says Dr. Cleeman.
Strengthening the quadriceps is especially important for knee replacement patients, particularly older ones, because this muscle group controls knee extension.
Quadriceps strengthening will ease pain, says Dr. Cleeman. Knee replacement surgery takes a while to recover from, especially if you’re older.
Strengthening the quadriceps is invaluable because it will make living so much easier, i.e., exiting chairs and cars, climbing stairs, etc..
Examples of Quadriceps Strengthening Exercises
Squats. These can be done by holding a stable support, such as the knobs on either side of an open door, and simply squatting up and down, or squatting while both hands are placed on a wall.

Or, says Dr. Cleeman, “Practice rising from a chair start with several cushions, then remove one at a time.” Work up to 20 repetitions.
Leg presses. This requires gym equipment. Keep feet flat on the pushing platform and don’t let legs bend more than 90 degrees. Work up to 20 repetitions.

Shutterstock/wavebreakmedia
Knee replacement patients, especially older ones, will benefit from a personal trainer once they are finished with all of the post-surgical rehabilitation exercises that were prescribed for them.
Sometimes the surgeon will prescribe specific exercises, and other exercises will be performed through special physical therapy.
Once these programs are concluded, the patient can then upgrade by hiring a personal trainer.
If money is tight, consider this format for just a few sessions. Recreation centers provide personal training at reasonable costs.
Whatever you decide, having knee replacement surgery means a lifelong commitment to home exercises to keep the knee functioning optimally.
 Dr. Cleeman is a highly experienced orthopedic surgeon and sports medicine specialist at Manhattan Orthopedics. He is committed to performing advanced minimally invasive procedures, allowing his patients to go home the same day.
Dr. Cleeman is a highly experienced orthopedic surgeon and sports medicine specialist at Manhattan Orthopedics. He is committed to performing advanced minimally invasive procedures, allowing his patients to go home the same day.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sasirin pamai
Sources: triarq.com
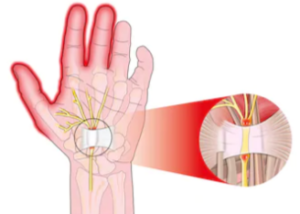
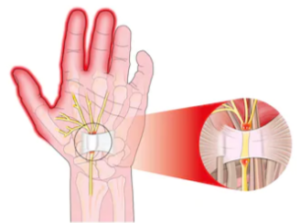
10 Minute Carpal Tunnel Release: No Stitches, Fast Recovery
Traditional carpal tunnel release requires up to three months of recovery, leaves scars and requires restrictive bandages up to two weeks following surgery.
However, there is a shorter, less invasive carpal tunnel release surgery that takes only 10 minutes, called stitchless endoscopic carpal tunnel release.
The incision is 1 centimeter and results in minimal scarring. A local anesthetic is used and there are no bandages necessary.
Stitchless endoscopic carpal tunnel release offers no restrictions after 48 hours and a recovery time of just one week. Stitchless endoscopic carpal tunnel release results in much less pain than the traditional “open” surgery.
Dr. John T. Knight, MD, an L.A.-based hand and wrist orthopedic surgeon and director of the Hand and Wrist Institute at the D.I.S.C. Sports and Spine Center, performs the stitchless endoscopic carpal tunnel release. I asked him some questions.
Why isn’t the stitchless endoscopic carpal tunnel release more well-known?
This technique has been around since the ’90’s but has become much more sophisticated.
When I first went into practice in the early ’90’s I treated quite a few patients with complications from other doctors that took a weekend course and were not hand specialists.
Once the equipment has become much more refined I began doing the procedure in the recent past. I have had excellent results and a much quicker recovery than the older open procedure.
There at two common techniques: one vs. two incisions. I use the single incision which minimizes scarring.
Can you comment on infection risk with stitchless endoscopic carpal tunnel release, vs. the traditional open carpal tunnel release?
I have never had an infection with either procedure, but usually the less invasive, the less infection, as the larger wounds are exposed to the air longer.
With any procedure, no matter how minor, there is always a risk of infection.
Outpatient surgery centers, like the one at D.I.S.C. Sports and Spine Center, have lower incidences of infection than a hospital, even if done in an outpatient setting.
We take extra precautions to ensure against infection, and is vitally important that any facility adhere to strict guidelines of hygiene and cleanliness to reduce the risk whenever possible.
Why don’t more surgeons utilize the stitchless endoscopy method for carpal tunnel release?
Most surgeons are creatures of habit and if they have had pretty good results with the open procedure, then they are unlikely to want to try a new technique.
Many surgeons find it difficult to learn endoscopic procedures, as it requires an ability to work with longer and smaller instruments at a distance from the structure to be repaired, or released in this case.
Are there any contraindications to the stitchless endoscopic carpal tunnel release, that would require the patient to undergo the open method?
If a patient has had a previous open release with recurrence, significant inflammatory disease such as rheumatoid arthritis, a tumor, or incomplete visualization doing it endoscopically.
Is the “local” anesthetic literally local to the hand/forearm, or is it actually a nerve block for the entire arm?
Usually we give a local injection in the palm and wrist along with intravenous sedation.
This allows for a quicker recovery for the patient, who can then begin mobilization of the hand and wrist within an hour or two of the procedure.
It is not uncommon for the patient to be able to hold a glass of liquid within a relatively short time span.
When they are discharged a few hours after the procedure, the only real restriction is to avoid any lifting or intense movement for a few days, but light activities are fine within a few days.
While pain medication is prescribed upon discharge usually very little is taken, as many patients manage their pain with over-the-counter medication like Advil during the initial healing process.
If you have been diagnosed with carpal tunnel syndrome, it would be very wise to consider the stitchless carpal tunnel release when conservative methods of treatment have failed.
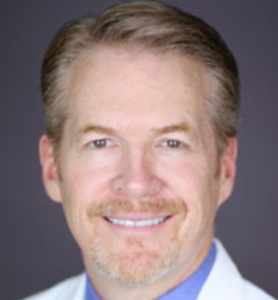 Dr. Knight is widely regarded as one of the most prominent hand and wrist specialists in the U.S., specializing in minimally invasive techniques for hand, wrist and upper extremity injuries and disorders.
Dr. Knight is widely regarded as one of the most prominent hand and wrist specialists in the U.S., specializing in minimally invasive techniques for hand, wrist and upper extremity injuries and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/jcomp
What Exercises Relieve Carpal Tunnel Surgery Pain?

After carpel tunnel syndrome surgery, it’s possible to experience lingering or residual pain that might shoot up the entire arm and affect the shoulder.
Remember, the carpal tunnel compression has caused irritation to the median nerve, which runs the length of the arm (beginning from hand) all the way up to the shoulder and neck where it comes out from the spinal cord.
Pain from carpal tunnel syndrome doesn’t always disappear 100 percent immediately after surgery.
The median nerve may still be irritated, and this can cause pain or discomfort even several days after carpal tunnel surgery, including pain in the shoulder. My mother had carpal tunnel surgery on both hands at the same time.
She was experiencing pain from carpal tunnel in the shoulder before surgery, and post-surgery for several days, and sometimes it ran down the length of the arm.
Based on my experience working with my mother; plus my experience as a certified personal trainer working with clients who had various body tweaks; and my own experience with sports injuries over the years, I had my mother do some specific exercises to relieve the post-surgical carpal tunnel pain.
The surgeon told her that this post-surgical carpal tunnel shoulder pain was “par for the course” and that it would eventually disappear.
However, in the meantime, it’s not pretty. A person with this problem will typically intuitively remain immobile and ride the pain out, perhaps taking “pain pills,” namely, whatever their surgeon prescribed for them for post-surgical carpal tunnel pain.
The combo of narcotics and inertia didn’t work for my mother, and quite frankly, I don’t see how they can work for anybody’s post-surgical carpal tunnel pain.
The drugs caused other undesirable side effects, and inertia “unteaches” the body to be efficient at movement.
Stand with feet shoulder width apart.
Raise both arms straight up, as though to shake someone’s hand. Keep them nearly straight. Raise them parallel to floor.
If this hurts, raise to just below the threshold of pain. If you can go past parallel, do so. Lower. Repeat for total of 12 times.
Continuing to stand, keep both arms straight at sides, palms facing body.
Rotate palms outward so that they’re facing forward, then rotate them so that they’re facing behind you.
This action will open and close the shoulder joint as well as rotate entire arm. Repeat both directions 12 times.
Bend over, one hand resting on countertop or table for support.
Let other arm dangle. Rotate shoulder in circles, forward 12 times, then backwards 12 times, letting arm hang relaxed. Don’t bend arm. Repeat other side.
Place two coins on kitchen countertop about a foot apart.
Place hands before either coin. Now, cross forearms over each other so that opposite hands are now aligned with each coin. Return to start position. Repeat 12 times.
Standing, move arms as they would as if running in slow motion.
Exaggerate the arm movement so that shoulders get a good rotary and vertical workout. Do this for 30-60 seconds.
By this point, the shoulder pain should be mostly dissipated. If it isn’t, then perhaps you can design some different exercises.
I also recommend follow-up visits with the doctor who performed the carpal tunnel surgery.
Inertia in absence of structured exercise isn’t the answer; it will only further stiffen up the joint and reduce blood circulation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Shutterstock/WSW1985
Carpal Tunnel Syndrome: Why Post-Surgical Bandages Are So Thick

If you have carpal tunnel syndrome and planning on having the traditional, “open” surgical technique, you’ll be required to wear thick bandages that cover the carpal area of your hand for up to a few weeks following surgery.
The carpal area of the hand encompasses the wrist all the way up to the knuckles.
Your fingers will be free to move and bend, but the palmar and back of your hand will be bound in a thick wrapping of bandages.
My mother had carpal tunnel syndrome release surgery, the open technique, on both hands at the same time, and wearing the heavy bandages was no picnic.
She wondered why the wrappings had to be so constricting for such a seemingly small incision.
The purpose of the thick bandages following carpal tunnel surgery was to provide immobilization to the wrist.
Post-surgical swelling is another reason for the layers of bandages, since carpal tunnel release involves the cutting of a band of tissue that goes across the median nerve.
After 10 days, my mother had the bandages removed. They were cut away with a pair of shears by the surgeon’s nurse, and revealed incisions, with stitches, that appeared to be about an inch and a fourth in length.
The nurse then removed the stitches; a painless procedure. At that point, my mother was good to go, with no restrictions with the use of her hands as far as getting them wet.
When the bandages were on, she was instructed not to get any water on the wrappings.
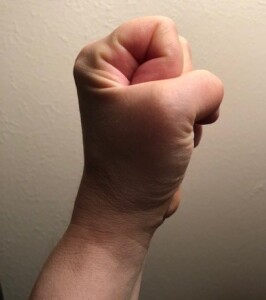
Symptoms of carpal tunnel syndrome:
- tingling, numbness and/or weakness in all the fingers except the pink
- reduced grip strength of the hand
- reduced pincer strength of the fingers
- inability to make a complete fist
- aches or pains in the hand; pain upon flexing the wrist (bending the palm so that it’s closer to the underside of the forearm)
- and pain upon tapping the area of the palm just above the wrist.
Symptoms of carpal tunnel syndrome can also include pain in the forearms and even shoulder, even though the compression site of the median nerve is at the wrist.
This nerve goes all the way up the arm, into the shoulder and runs into the spinal cord at the neck, and the entire nerve can become irritated.
If you decide to have carpal tunnel “open” surgery, expect to wear thick bandages for 10-14 days afterwards.
There is another type of surgery for this nerve entrapment disorder that eliminates the need for bandages afterwards: stitchless endoscopic carpal tunnel release.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Angkana Sae-Yang
Hand Exercises After Carpal Tunnel Surgery to Regain Strength in Senior Citizens
After my mother had carpal tunnel syndrome surgery on both hands, she was left with weakness in both hands; weak fingers and a weak grip.
This is because the carpal tunnel syndrome progressed from mild to severe in only a matter of several weeks.
As a result of carpal tunnel syndrome’s effect on the median nerve, she lost some use of her hands and fingers.
This meant that some muscles weren’t getting used for several weeks. When muscles don’t get used, they shrink or atrophy (become atrophied).
An atrophied muscle is a weakened muscle, and often very stiff due to dis-use.
The fingers have muscles, and just because they are naturally small, doesn’t mean they can’t atrophy and weaken when not used, and carpal tunnel syndrome at its worst will definitely cause muscle weakness in the fingers.
My mother’s EMG test did not detect muscle weakness (EMGs measure nerve conductivity), and the doctor said there was no sign of muscle atrophy.
However, the weakness was there for sure, and remained there even after the carpal tunnel surgery.
To combat this lingering weakness, I designed some exercises for my mother.
Post-surgical exercise for carpal tunnel release #1
The first obvious exercise for strengthening the fingers and grip following carpal tunnel surgery is to simply open and close the fist well past the point of fatigue. Each close should be as tight as possible.
Post-surgical exercise for carpal tunnel release #2
Roll out a section of toilet paper about 5-7 feet long. With just the carpal tunnel hand, hold one end of the paper, then start scrunching it up within the confines of your palm, without using the other hand for help.
See if you can bunch up all the paper into your palm without using the other hand to help.

Post-surgical exercise for carpal tunnel release #3
Next, lean forward in a seated position, forearm on thigh, palm up.
Place a weighted ball in palm and lift the wrist upward, so that your palm — still holding the ball — is facing towards you. Then relax.
Repeat past point of fatigue.
If this doesn’t fatigue you within about 40 repetitions, use a heavier weight.
Small weighted balls can be found in sporting goods stores or online.
Post-surgical exercise for carpal tunnel release #4
Pretend there’s ink on the tip of your middle finger.
Keep fingers together and straight, and move just the wrist, and “draw” each letter of the alphabet in the air, pretending that the ink on your middle finger is creating the letter on a vertical sheet of paper hanging in the air.
Each exercise should be done 2-3 times each, and then each session three times per day.
These exercises are not replacements for the normal hand/finger activity that you’d do as part of your daily routine.
These carpal tunnel post-surgical exercises are supplements to your routine daily hand motions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Alexonline
Do Blacks with Freckles Have Higher Melanoma Risk?

Do freckles raise the risk of melanoma in a black person?
Maybe you already know that melanoma risk in blacks, overall, is far lower than in whites or Hispanics, and perhaps you already know that having freckles is one of many increased risk factors for melanoma.
But what about black people who have freckles? After all, people with freckles are overwhelmingly of the Caucasian race.
Blacks do get freckles, and being black does not insure against developing melanoma.
The question is: Do freckles in blacks raise their risk of melanoma?
“Yes. Overall assessment of one developing a melanoma does not depend on a single factor,” says Joshua L. Fox, MD, founder and director of Advanced Dermatology, P.C., of New York and New Jersey.
“It depends on various factors such as skin type, personal or family history of melanoma, life-time accumulative UV exposure, etc.
“Thus, we can attribute one’s risk based on one or two physical differences. I have diagnosed melanoma in blacks.
“Their high risk areas (different than that for Caucasian) are palms, soles, mouth and under the nails.”
People with dark skin are 20 times less likely to get melanoma than Caucasians (who have no family history of this disease), but this doesn’t mean they can’t develop it.
However, blacks are more likely than whites to develop a certain kind of melanoma, called acral lentiginous (ALM).
ALM accounts for half of the melanomas that occur in dark skin.
What’s even more troublesome about ALM is that it develops in locations that you wouldn’t think are at risk for skin cancer: soles of the feet; palms of the hands; beneath fingernails; and even on mucous membranes that line the nose, mouth and anus.
ALM may appear as a bruise, or a streak in the nail. Benign nail streaks are common, but the hallmark feature of an ALM nail streak is that it originates at the base of the nail bed, whereas a benign nail streak usually sits in the middle of the nail bed.
However, this doesn’t mean that a nail streak that connects to the base of the nail bed is necessarily a melanoma.
These indefinites are why all people, including blacks and even dark skinned blacks, should examine their skin monthly and have annual screenings for melanoma by a dermatologist.
Since blacks with freckles do have that increased risk of melanoma, is this heightened risk just in the freckled areas of their body (most prominently the face), or does this higher risk of melanoma apply to any part of their body?
Dr. Fox explains: “Once a person is at higher risk, the risk is not only in the area of freckling, but in all body areas, particularly in areas of high risk for African Americans.
“These are the palms, soles, nails, mouth and other mucous membranes.”

In 1987 Dr. Fox founded the AAD Melanoma and Skin Cancer Prevention Program in Queens, NY. He has been chief of dermatology of several major teaching hospitals including Mt. Sinai Hospital of Queens.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: skincarephysicians.com/skincancernet/who_is_most.html
Why Can GERD Cause a Stomach “Hiccup”?
Have you been experiencing something like an occasional hiccup, that your doctor has said is the result of acid reflux or GERD (gastroesophageal reflux disease)?
This isn’t in reference to what we all know are “the hiccups.” When it comes to GERD, this hiccup-like sensation is different, kind of like a spasm in the stomach.
Acid reflux can cause a wide assortment of symptoms — not just the widely publicized heartburn.
Hiccups and GERD
“Hiccups can be associated with GERD,” says Dr. Maxwell Chait, MD, gastroenterologist at ColumbiaDoctors Medical Group in Westchester County, NY.
Other Causes of Hiccups
“It can be due to irritation of the diaphragm or the vagus nerve because of severe reflux, ulcer of the esophagus or even a tumor invading these structures.”
An esophageal ulcer can be caused by acid reflux. A tumor can grow out of esophageal cells, or be a metastasis from another site in the body.
Dr. Chait adds, “Also, severe distention of the stomach pushing up on the diaphragm can cause this, such as in gastroparesis, which is a motility disorder that can be seen in such diseases as diabetes.”
Stopping the Hiccups
If you suddenly have a hiccup — see what happens when you hold your breath. A benign hiccup just might go away.
If you experience a lot of hiccup-type activity or stomach spasms, see your doctor about the possibility of acid reflux.
In the meantime, make sure that you are trying to avoid foods that you know trigger acid reflux or stomach hiccups.
Take note of any foods that seem to be correlated with heartburn, hiccups or other GERD symptoms such as a burning feeling in the throat, an unpleasant taste in the back of the throat and a liquid regurgitation of just-eaten food.
If you’re a fast eater and/or tend to gulp your beverages, slow down. Also cut back on late night eating.
These tactics will help reduce GERD symptoms including stomach hiccups.

Dr. Chait’s practice interests include digestive conditions such as colon cancer, gastrointestinal endoscopy and internal medicine. He has authored numerous publications in reputed journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/nhungboon
How Much Weight Gain Raises LDL Bad Cholesterol?

Even a small weight gain in fat can raise your “bad” cholesterol (LDL), and I’m talking a very small weight gain.
“Interestingly, a 10 percent weight loss has been shown to significantly decrease a broad variety of health risk parameters,” says Richard Kelley, MD, a practicing physician in Texas for 20+ years, and author of “The Fitness Response,” “The Three-Hour Appetite” and the ebook, “The Fitness Response ‘Diet’ for Women.”
Dr. Kelley continues, “For example, a woman who is 5 ft. 2 inches tall and weighs 170 pounds, would be at a much healthier weight, at 120 pounds, by body mass index.
“However, it is evident through research and clinical experience, that if this woman even lost 17 pounds (10%) off of her starting weight, a variety of physical parameters tend to improve.
“With a 10 % weight loss, we often see blood pressure improve, blood glucose levels decrease, asthma may improve, as well as decreases in cholesterol levels, including LDL level.”
When I was a personal trainer I had a new client who wanted to lose 15 pounds.
She had gained about 13 or 14 pounds of pure fat from junk food bingeing that resulted from stress. The year prior her LDL or bad cholesterol was in the 80s.
Shortly before seeing me, she had a lipid test and this time the LDL bad cholesterol was in the 130s.
She was floored because she had started eating healthier and less just a few months prior, and had even begun losing a little weight.
I said that the LDL increase was from the 14-pound weight gain, and that had she taken the test eight weeks prior, the bad cholesterol probably would have been even higher.
Dr. Kelley explains, in reference to the 5-2 woman, “Conversely, this same woman might see elevation of her LDL and total cholesterol even with a 5 to 10 pound weight gain, over a fairly short period of time.”
Dr. Kelley stresses that genetics influence LDL response to weight gain and food.
“I have seen many individuals who were well over 100 pounds overweight who had completely normal range LDL and cholesterol panels.
“By the same token, most physicians have seen patients who are rail-thin who have total cholesterol and LDL levels which were off the charts.”
Dr. Kelley adds that he’s been surprised at how much of an improvement some patients experience with their lipid/cholesterol panels with just a 5-10 pound weight loss.
He also explains, “I don’t know that there is any data that shows a direct and specific, linear correlation of increases in cholesterol with specific number of pounds of weight gained.
“Meaning, it is unlikely you will see that a 10 pound weight gain in a susceptible individual, necessarily means that there will be a corresponding, linear increase in cholesterol levels by a particular factor of X.”
Dr. Kelley states that it’s common for doctors to observe increases in total cholesterol including LDL that cannot be attributed to just an increase in a patient’s weight.
 Richard Kelley, MD, is an author, speaker, fitness expert and transformation coach.
Richard Kelley, MD, is an author, speaker, fitness expert and transformation coach.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Phonlamai Photo
Dumbbell Curls vs. Barbell Curls: Pros and Cons

Dumbbell curls vs. barbell curls: Which is better, and what are the pros and cons?
Many of the great bodybuilding champs swear by barbell curls, yet many other bodybuilding legends swear by dumbbell curls.
But let’s look at it this way: Which routine – dumbbell curls or barbell – will better prepare you to have the strength to scoop your arms under a family member who just fainted and pick him or her up?
Of course, deadlift and squat workouts should be included in any strength training program, but in addition, isolated biceps work is important.
Dumbbells, as opposed to barbell work for the biceps, will better prepare you because they allow subtle shifts in hand/wrist and even forearm position while lifting — and this is what would occur if you were lifting a person.
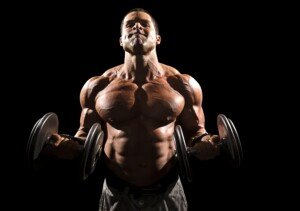
Shutterstock/Mark McElroy
Of course, you need more than strong biceps to scoop something heavy off the floor.
You also need stability and strength in your lower back, plus legs (“Lift with your legs”).
Barbell Curls vs. Dumbbell Curls
Both routines have their virtues, and you should not replace one with the other, even though it’s okay to stick to just one mode for a while when you get tired of the other.
- With dumbbells, you have greater range of motion, since you can bring your arms back further.
- A barbell will get in the way as it makes contact with your front, thus limiting range of motion. Many people don’t like this.
- With dumbbells, you can include wrist movements during the routine. A barbell, which fixes the wrists in place, prevents this.
Dumbbell biceps routines more closely mimic real-life lifting, because in real-life lifting, your wrists are rarely in a fixed position, but rather, in a variable position, sometimes continuously shifting angles.

Shuttersock/Nicholas Piccillo
A barbell also has limitations if all you have is a standard straight bar, because the straight bar has a tendency to strain the wrists for some people during biceps routines.
You can counteract this strain by using dumbbells and rotating your palms inward a bit.
In addition to a standard straight bar is the “E-Z” bar, which is very popular for biceps routines, because the bent nature of the middle portions of the bar allow you to use it with inward palms, eliminating wrist strain.

Shutterstocfk/BLACKDAY
But if you don’t have access to an E-Z bar, you’re stuck with the straight bar.
The preacher curl apparatus can be used for E-Z or straight bar work, and many find this equipment to be very stabilizing to the elbows, as well as very effective at isolating the biceps group.
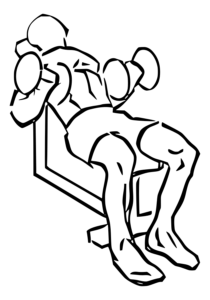
Dumbbells allow you to do hammer curls, and are also far more convenient to use while in a seated position, expecially angled back.
Everkinetic.com
However, there’s nothing like doing biceps routines with a loaded Olympic bar.
The length of this bar adds a new dimension to the resistance, and many women struggle with an unloaded bar because it’s long and weighs 45 pounds.
Imagine curling one of these with a 25 pound plate on each end.
No science proves dumbbells superior to a bar, nor vice versa. What it ultimately may come down to is what feels better to the athlete. In short, it may all come down to “Do what’s best for YOU.”