Aspirin vs. Coumadin for Blood Clot Prevention after Surgery

Find out if aspirin reigns over the powerful blood thinner Coumadin for blood clot prevention following joint replacement surgery.
Typically prior to joint replacement surgery, the patient is given Coumadin (warfarin), a powerful blood thinner, to help prevent development of blood clots during and after surgery.
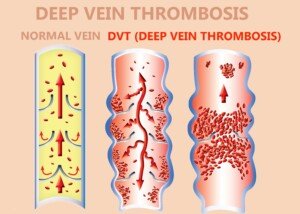
These blood clots are also known as deep vein thromboses (DVT), and can migrate to the lungs and become a pulmonary embolus: a very life-threatening situation.
The Rothman Institute at Jefferson conducted a study showing that aspirin is at least as effective in blood clot prevention as is Coumadin, and more effective in other ways.
You may be wondering, though, why not just stick with Coumadin, since this is more powerful?
Well, that’s the problem; as a blood thinner, Coumadin can do its job too well.
“While warfarin is successful in the prophylactic prevention of clots, it can also lead to increased bleeding,” explains Javad Parvizi, MD, lead investigator, and director of research at the Rothman Institute.
He adds that Coumadin can also lead to infections and readmissions to the hospital.
My father has had three joint replacements, and each time, had to take Coumadin leading up to the surgery, but did not have any complications from the drug.
The Rothman study is very compelling because it compared outcomes of over 26,000 patients who had joint replacement surgery at the Institute.
Over 1,800 received aspirin prior to their joint replacement surgery, and over 24,000 received Coumadin prior to their joint replacement procedure. Both groups received monitoring for up to three months post-surgery.
Point two percent of the aspirin patients developed a pulmonary embolism. And one percent of the Coumadin group developed a pulmonary embolism.
The difference between point two percent and one percent is very statistically significant.
The difference between aspirin and Coumadin doesn’t end there. Hematoma (a type of blood leakage) and seroma (fluid leakage), plus wound issues, acute infection and 90-day mortality rates were actually lower in the aspirin group.
“Our study shows that aspirin is a viable alternative to warfarin in healthy patients,” says Dr. Parvizi, “with better results in preventing clots, and a lower rate of bleeding and wound complications.”
If you’re facing joint replacement surgery, ask your surgeon about aspirin and tell him or her about this study.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Doerr Martin Frommherz
Source: sciencedaily.com/releases/2012/11/121107195842.htm
Is Every Pulmonary Embolism the Same or Can Some Go Away??

There may actually be a such thing as a pulmonary embolus that does not require treatment.
“ A pulmonary embolism (PE) is the development of a blood clot, usually in the veins of the legs, that travels up and gets stuck in the arteries of the lungs,” says Geoffrey Barnes, MD, cardiologist and vascular medicine specialist at the University of Michigan Health System.
“The standard treatment for a PE is to take a blood thinner (anticoagulant).
“The purpose of the blood thinner is to prevent new blood clots from forming.
“The blood thinner itself will not dissolve away the blood clot that already exists.
“Rather, your body has natural activities that will dissolve the blood clot and help convert it into fibrous scar tissue.
“Sometimes our bodies are able to completely dissolve the blood clot so that we cannot see it anymore with our tests.
“Other times the body dissolves part of the clot, and the rest turns into fibrous scar tissue.”
A Study on Pulmonary Emboli
A study shows that some pulmonary emboli can resolve on their own and do not require treatment.
Conditions that are ripe for blood clot formation in a vein (deep vein thrombosis) include orthopedic surgery, lengthy surgery, old age and prolonged immobility following surgery.
Smoking, use of birth control pills and hardly moving on a long airline flight can also give rise to the development of a DVT. Pregnancy is another risk factor.
DVT can even occur in young adult athletes.
Once a blood clot becomes a pulmonary embolus, grave complications can occur including sudden death.
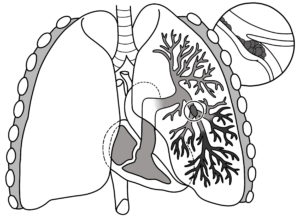
Pulmonary embolism
This report explains that not all pulmonary emboli require the same aggressive treatment in the form of level of blood thinners.
Diagnostic tests have become increasingly sensitive, and thus, may pick up very small, rather insignificant clots.
These are the clots that can resolve on their own.
So what’s wrong with aggressive treatment for these relatively insignificant clots in the lung?
Treatment for pulmonary embolus typically involves powerful blood thinners that can raise the risk of post-surgical bleeding.
Unfortunately, today’s medical technology does not include an instrument that can distinguish between blood clots that are dangerous and those that do not necessitate treatment.
For instance, the computerized tomography pulmonary angiogram is remarkable at picking up pulmonary emboli, but at the same time, it also detects smaller clots that can go away on their own.
So what’s the solution for now?
The researchers recommend that doctors increase their criteria for blood clot screening prior to ordering blood thinner therapy.
Some criteria may be the location and size of the blood clot.
Hallmark symptoms of a pulmonary embolus are sudden shortness of breath and chest pain.
Additional Symptoms of a Pulmonary Embolus
Swelling in one leg, bluish skin, clammy skin, pronounced sweating, irregular or rapid heartbeat, a weak pulse, fainting and lightheadedness.
The report is in the September 2012 Journal of the American Academy of Orthopaedic Surgeons.
 Geoffrey Barnes, MD, is a cardiologist and vascular medicine specialist at the University of Michigan Health System and spokesperson for the World Thrombosis Day Campaign. Dr. Barnes’ clinical interests include treatment of vascular disorders, anticoagulation and general cardiac care.
Geoffrey Barnes, MD, is a cardiologist and vascular medicine specialist at the University of Michigan Health System and spokesperson for the World Thrombosis Day Campaign. Dr. Barnes’ clinical interests include treatment of vascular disorders, anticoagulation and general cardiac care.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Sources:
sciencedaily.com/releases/2012/09/120901085140.htm
mayoclinic.com/health/pulmonary-embolism/DS00429/DSECTION=symptoms
Can High Vitamin D Doses Help Psoriatic Arthritis?

A doctor answers this question as well as if low vitamin D levels can make psoriatic arthritis worse.
If you suffer from psoriatic arthritis, you may be curious over whether or not vitamin D in high levels can help relieve symptoms, and conversely, if a vitamin D deficiency can make psoriatic arthritis worse.
“Vitamin D deficiency is quite prevalent in patients with both psoriasis and psoriatic arthritis, and in some studies low vitamin D has been shown to be associated with increased inflammatory markers in the blood and increased clinical disease activity,” explains Stuart M. Levine, MD, Vice-Chairman, Department of Medicine, Rheumatology, Medical Faculty Practice, Medstar Good Samaritan Hospital, Baltimore.
However, he adds that the significance of this association has not been determined.
It also has not been proven that low levels of vitamin D, alone as an issue, can cause psoriatic arthritis or psoriasis (skin only).
Dr. Levine points out that he is not aware of any treatment trials that involve vitamin D, which is found in fortified foods, namely milk, cereal and meal replacement bars and beverages. It also comes in supplement form.
Dr. Levine explains that “it is reasonable and is my standard practice to look for vitamin D deficiency in all inflammatory arthritis patients, and to treat patients with documented deficiency with appropriate doses of vitamin D until they are back in the normal range.”
Now, getting back in the normal range is not the same as taking the so-called therapeutic doses of this macronutrient.
In fact, Dr. Levine says, “Raising vitamin D levels to higher than normal levels has not been studied and is not recommended.”
Symptoms of Psoriatic Arthritis
Here are the symptoms of this uncommon autoimmune disease that is sometimes misdiagnosed as rheumatoid arthritis:
- swollen fingers and toes (may appear sausage-like
- hand and foot swelling, possibly deformity
- foot pain, especially at the back of the heel or the sole of the foot
- lower back pain.
Psoriatic arthritis can cause a back condition called spondylitis, which causes inflammation of the joints that are between the spinal vertebrae, as well as inflammation in the joints between the spine and pelvis.
 Dr. Levine’swork has been published in peer-reviewed journals including PLoS One, Arthritis & Rheumatism, Journal of Rheumatology, Seminars in Arthritis and Rheumatism, and the American Journal of Medicine.
Dr. Levine’swork has been published in peer-reviewed journals including PLoS One, Arthritis & Rheumatism, Journal of Rheumatology, Seminars in Arthritis and Rheumatism, and the American Journal of Medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Image Point Fr
Why Hunters Aren’t Sissies for Using Hearing Protection
You’re NOT a sissy if you use hearing protection, yet many hunters fail to protect their ears from the loud blasts of rifles which can reach up to 160 decibels.
Having Healthy Sharp Hearing Is Not a Sign of a Sissy
A target shooter, says the Oregon Occupational Health and Safety Administration, can suffer a whole years’ worth of noise exposure in a matter of minutes.
Hunters often protect themselves from the elements in a variety of ways (e.g., sunscreen, purified water), but neglect protecting their hearing from firearm noise.
“Hunters should always use ear protection because they never know when they will have the opportunity to fire their guns,” says Michael Stewart, PhD, Professor Emeritus of Audiology at Central Michigan University and an avid hunter.
“The most commonly used guns for small and large game hunting generate impulse noise high enough to cause hearing loss and associated tinnitus with even one shot under the right acoustic conditions.”
Tinnitus is ringing in the ears, and this can be permanent. Dr. Stewart continues, “Hunters should use electronic hearing protection or non-linear plugs (ex. combat arms).
“These devices allow the hunter to hear soft sounds yet attenuate loud sounds such as firearm noise to safe levels.”

Freepik.diller
Dr. Stewart conducted a survey of 300 shooters; about 40 percent never employed protection for their ears during target practice. 40 percent!
Why is this? Do they think only sissies “cover” their ears? There’s certainly nothing macho about needing hearing aids!
How many used hearing protection all the time? Under 12 percent.
How many used any hearing protection during hunting? Less than 20 percent.
How great is the potential for hearing loss from gun blasts? Dr. Stewart says, for example, that if several blasts are fired from a large bore firearm within 3-5 seconds, the probability of hearing loss is significant.
Does this mean that the hunter, upon arriving home, will have difficulty hearing his wife or kids talking to him? No.
Hearing loss that’s incurred from one day of shooting will not necessarily be noticeable in a normal environment.
The hearing loss may have impaired the hunter’s ability to decipher words from 40 feet away, when the day before the hunting trip, he could have deciphered them from 50 feet away.
Nothing macho about that. And by the way, some hunters and shooters are women, and not all of THEM wear hearing protection for their ears, either. What a mystery.
The deterioration of hearing is not going to be detectable in day-to-day living experiences, “but the individual may have difficulty hearing in very noisy environments,” says Dr. Stewart.
And over time, more and more hearing loss from rifle blasts will start becoming noticeable, as the hunter has to repeatedly ask people to repeat things, or finds he can’t understand the TV unless it’s pretty loud.
This is called noise-induced hearing loss and it is not reversible! “Sudden hearing loss from excessive noise exposure (acoustic trauma) can also occur.”
Dr. Stewart urges all hunters to wear ear protection when shooting firearms.
Ear muffs are sold in the hunting supply section of sporting goods stores and can be ordered online.
“Choose devices with high noise reduction ratings (over 25 dB),” says Dr. Stewart.
A better option is to, in addition to the ear muffs, wear custom made earplugs; hearing aid clinics offer this service. They can also be made from home.
Don’t feel like a sissy for protecting your ears from becoming like an old person’s.
Dr. Stewart also recommends electronic hearing protection (behind-the-ear or in-the-ear devices).
These allow the hunter to hear normally while waiting for approaching game, yet they protect hearing when the rifle is shot.
Dr. Stewart adds that too many hunters believe that hearing protection is too expensive to bother with.
And many other hunters believe that ear muffs or plugs would make them look like a…well…you already know.
But a hunter, who spends quite a bit of money on reliable hunting equipment and clothes, should consider the expense of hearing protection to be part of the experience of hunting, and an investment in hearing protection.
The Price of Hearing Protection
Hearing aids are very expensive, not to mention a major hassle (know anyone with hearing aids? Ask them), and a hunter will never be able to get back his (or her) lost hearing.
The ear muffs are actually cheap, coming in as low as $15. Custom made earplugs can be around $100 for a pair, maybe $150 tops.
Electronic devices can range from $200 to $600. Dr. Stewart, who suffered permanent ringing in the ears from hunting as a child, insists that electronic protection should be a staple of every hunter’s gear.
If that sounds pricey, then start with a $175 investment in the combo of ear muffs and custom made earplugs. This is nothing compared to that $1,000 rifle.
 Dr. Stewart is widely published in academic journals, and his research area focuses on industrial and recreational hearing conservation, and amplification.
Dr. Stewart is widely published in academic journals, and his research area focuses on industrial and recreational hearing conservation, and amplification.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Sources:
newswise.com/articles/unprotected-hunters-at-risk-of-hearing-loss?ret=/articles/list&category=life&page=1578&search
http://www.cbs.state.or.us/external/osha/pdf/pubs/3349.pdf
Pulmonary Embolism Detection with D-Dimer & CT Scan

In the ER a doctor should order a D-dimer test if there’s suspiction of a pulmonary embolism based on symptoms.
It’s alarming, however, that in some cases this procedure is not followed.
A study shows this. And another finding of the study was that some ER doctors were ordering CT scans for pulmonary embolus even though the D-dimer test was negative.
The study was carried out at the Warren Alpert Medical School of Brown University and Rhode Island Hospital, Providence, RI.
You’re in the ER with Concerning Symptoms
Symptoms that are suspicious for a pulmonary embolism — which is a blood clot from the lower extremity that travels to the lungs — include chest pain, difficulty breathing and one leg that is swollen, painful and red.
The physician should order the D-dimer.
But if this test comes back positive, is a CT scan (which emits radiation) always necessary?
“Not every D-dimer needs a follow-up CT chest scan,” says Reena Patel, MD, a board certified family medicine physician who treats patients at Garnet Health Urgent Care in NY.
“It is helpful to rule out PE if it is low/normal. If suspicion is high for pulmonary emboli, and the D-dimer is elevated, a chest scan or V/Q scan should be ordered to look for a potential clot.
“Generally, the lower extremities will also get an ultrasound looking for a DVT.
“If the D-dimer is low and you have a lower suspicion of PE, then a chest scan is not always imperative.
“This is when scoring criteria and looking at the patient as a whole come into play.
“Specifically for PE I can use Wells’ criteria, PERC or PESI scores.
“This can give me a good idea of what percentage risk a patient has for the emboli.
“If a patient had a low score, potentially unclear or low risk history and associated low D-dimer result, I would not always need to add on chest imaging.
“It is also important to recognize what else aside from a PE/DVT may cause an elevated D-dimer.
“This can happen with DIC [blood clotting disorder], malignancy, pregnancy, renal disease and even surgery, to name just a few.”
Positive D-Dimer on Three Separate Occasions but No Pulmonary Embolism
My mother’s D-dimer test came back positive on three separate ER visits over time. We were told that this could mean that there was a blood clot somewhere in her body.
We were also told that simply being elderly could cause a positive D-dimer result.
My mother then underwent a CT scan of her chest, which did not reveal a pulmonary embolism.
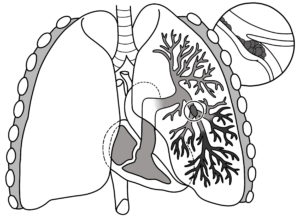
pulmonary embolism
An elderly person with heart disease would certainly not be low risk for a PE. But heart disease can also yield a positive D-dimer.
The Study
For the Warren Alpert study, 5,344 patients were involved, and of the ones who had a positive D-dimer, 42 percent did not get the CT scan.
These patients should have had the CT scan, says lead study author Michael T. Corwin, MD, in the report.
The CT scan was performed, however, in 7 percent of the people who had a negative D-dimer.
Dr. Corwin says that these patients should not have had the CT scan. This is unnecessary exposure to radiation.
The paper points out that a lot of CT scans are being ordered despite a negative D-dimer, and a lot of those CT results are negative for a pulmonary embolism.
D-dimer testing does not rule out PE completely, but in people with a chance of having this — based upon their presenting clinical picture — a negative D-dimer can spare these patients the radiation dose from a chest CT scan.
In addition to treating many chronic conditions, Dr. Patel treats urgent conditions that affect every part of the body. Instagram: That_dr_next_door
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Tyler Olson
Source: sciencedaily.com /releases/2009/05/090522131927.htm
Can a Thin Child Have Sleep Apnea?

Is it possible for a skinny or thin child to have sleep apnea?
Yes, believe it or not, a thin child can actually suffer from obstructive sleep apnea without the parent ever realizing it.
Because sleep apnea is sometimes misdiagnosed as ADHD, Dr. Frank Barnhill, MD, sees many children with sleep apnea.
Dr. Barnhill is a board certified family physician practicing child and adult preventative care/ADHD-behavior medicine in upstate South Carolina,
Though SA much more commonly strikes overweight middle-aged men, thin adults can have sleep apnea, and of course, since kids can be afflicted with this disorder, thin children as well can develop sleep apnea.
Dr. Barnhill explains, “Yes, it can occur because of central sleep apnea – CSA — a true brainstem dysfunction.” This dysfunction in the brainstem is not caused by excess fat in the body.
What causes the brainstem dysfunction?
Dr. Barnhill says: “Those who are born with it suffer from failure of the brainstem to mature. This is called a neurodevelopmental disorder and its cause is unknown.
Other causes or theories include hazardous chemical use during pregnancy and simple genetics as an inheritable disorder.
For whatever reason, the child’s brainstem respiratory drive center fails to send proper messages to diaphragm and chest muscles to prompt normal breathing during sleep.”
So why does such a child’s apnea (thin or overweight) occur only during sleep?
Dr. Barnhill explains: “While we sleep we rarely use our chest muscles to take a breath. Most of our breathing occurs as a result of the brainstem sending messages that stimulate the diaphragm to contract and draw air into our lungs.
“When we lay down and go to sleep our breathing naturally slows and becomes more shallow and we don’t really intake as much air.
“Anything that makes this worse causes a decrease in blood oxygen which would normally prompt the brainstem to send more and stronger messages to breathing muscles and the low oxygen would be corrected. In CSA this just doesn’t happen.”
Other reasons why a thin child can have sleep apnea (central) is due to other insults to the brainstem such as:
- Brainstem stroke
- Infections
- Overuse of narcotic (painkillers)
- Brain trauma
- Exposure to toxins like lead
- Some cardiac conditions.
What percentage of kids with sleep apnea are thin?
Dr. Barnhill says that most children (85 percent) with CSA are not overweight.
However, most children (65 percent) with obstructive sleep apnea are indeed overweight.
The obstructive version is when the structures deep in the throat become too relaxed during slumber and obstruct the airway.
Enlarged tonsils or an enlarged thyroid can also cause obstructive sleep apnea … and this can happen in thin kids.
About 2 percent of kids have either OSA or CSA, or a combined type.
 In practice for 30+ years, Dr. Barnhill is the author of “Mistaken for ADHD.” He has additional training in Infant, child and adolescent medicine, urgent and emergent medicine, and gerontology. Selfgrowth.com/experts/frank_barnhill
In practice for 30+ years, Dr. Barnhill is the author of “Mistaken for ADHD.” He has additional training in Infant, child and adolescent medicine, urgent and emergent medicine, and gerontology. Selfgrowth.com/experts/frank_barnhill
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer. .
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer. .
Is Cervical Cancer Screening Necessary for Gay Women?

Cervical cancer isn’t just caused by HPV transmission between a woman and a man, which is why lesbians absolutely should get an annual Pap smear.
Though we know that cervical cancer is primarily caused by the human papillomavirus (HPV), which is transmitted via intercourse between a man and a woman.
Thus, one has to wonder where gay women fit in, when it comes to routine Pap smears.
Though some lesbians have had sex with men, what about lesbians who have never been involved with a man, and absolutely have no intention of ever getting close to a man?
Do such gay women still need to get their annual Pap smear? How much are gay women at risk for cervical cancer?
I posed this intriguing question to Lisa B. Bazzett, MD, a gynecologic oncologist (cancer specialist) at Ochsner Medical Center in New Orleans.
The literature, regarding Pap smears and cervical cancer screening, typically states that women need to begin getting Pap smears either
1) when they become sexually active, and
2) or when they turn 21. This directive for Pap smear screening and cervical cancer is ubiquitous, yet leaves out a particular segment of the populace, the gay woman.
Can HPV be transmitted from one gay woman to another? Though a lesbian may have never been near a man and may have no intentions of such, her partner may have been with a man and may have contracted the HPV.
Though lesbian sex obviously does not involve the same kind of penetration that heterosexual intercourse involves, a gay woman can still contract HPV from her lesbian partner (who contracted it from a past heterosexual relation). The result could be cervical cancer.
Dr. Bazzett explains that this is possible, even though there is no vaginal penetration with a male organ, because HPV can be transmitted from skin-to-skin contact.
Thus, the mere act of genital fondling and rubbing, in the absence of actual intercourse, can transmit HPV.
You can now see how a gay woman can end up getting cervical cancer, and thus needs to get Pap smears on a routine basis.
Dr. Bazzett explains, “As for lesbians …. I think anyone that engages in any sexual activity, should have yearly Paps.
“I have plenty of lesbians in my practice with HPV. With any sexual partner, you never know about their previous sexual activity, or the person they were with, etc. etc.”
As for the origins of HPV in the first place, Dr. Bazzett says, “We don’t know where HPV comes from. It’s been around a long time, but linked to cancers just in the last couple of decades.”
 Dr. Bazzett specializes in the treatment of malignancies of the female reproductive organs including that of the ovary, uterus, cervix, vagina and vulva.
Dr. Bazzett specializes in the treatment of malignancies of the female reproductive organs including that of the ovary, uterus, cervix, vagina and vulva.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Emily frost
Painful Sex, Vaginal Pain: Q & A with a Medical Doctor

Painful sex is a problem for more women than you think. Some women fake sexual pleasure to please their men, but other times, the pain during sex is so agonizing that these women avoid sex at all costs.
When women don’t know why they have painful sex, they are more apt to believe the problem is “all in their head.”
But painful sex is a real problem that’s in the genital area, NOT a woman’s head.
If you suffer from painful sex, it has a name: DYSPAREUNIA, of which vestibular vulvodynia is a possible cause.
Vestibular vulvodynia describes a condition that afflicts many women in varying degrees.
The degree of pain during sex can vary, from minor discomfort to excruciating.
In fact, in severe cases of painful sex, the pain has been described as feeling like a steak knife is being jammed through the vaginal entrance. In severe cases of vestibular vulvodynia, sexual relations are not possible.
I asked an expert a number of questions about vestibular vulvodynia: Adelaide G. Nardone, MD, OB/GYN, Medical Advisor to the Vagisil Women’s Health Center; Providence, Rhode Island.
Just what is VV?
Vulvodynia is a condition of chronic pain and discomfort in the vulvar area. It is considered to be a pain disorder and the exact etiology (cause) is unknown.
It has been associated with a prior history of certain conditions such as chronic yeast infections, allergic reactions, low estrogen levels, trauma or injury to the vulvar area, and even genetic factors and sexual abuse.
Why is it so painful?
While the exact cause of the pain is unknown, there are theories that women with this problem have suffered some type of nerve damage to the sensory nerves in this area, which results in chronic and sometimes debilitating pain.
It may also be possible that they have developed a state of “hypersensitivity” from prior insults such as chronic infections or allergic reactions.
Vulvodynia is also reported in postmenopausal women, so there may be some link to low estrogen levels as well.
Whatever the cause, it is real pain for these women and has real impact on their overall quality of life.
Can VV be so painful, that it outright prevents a woman from having sex?
Vulvodynia is often so painful that it prohibits women from enjoying a healthy sexual relationship.
Many women can no longer engage in any sexual activity because mere contact with that area results in excruciating pain. This has been and continues to be a major quality of life issue for VV sufferers.
Furthermore, many of these women cannot engage in regular exercise, they cannot use tampons, they cannot wear certain clothing, etc.
Many women refrain from openly discussing this delicate issue with others, so they often feel isolated, “different” and may even suffer with depression.
One step in the diagnosis of VV is the “Q-tip” test. This is a simple procedure done in a doctor’s office whereby a Q-tip is gently applied to the vulvar area. This alone is enough to provoke “pain” in these patients.
The doctor may then go onto “mapping” the pain and its intensity. This test also helps to distinguish if the patient has generalized VV or localized VV, which is referred to as vulvar vestibulitis syndrome.
How do patients describe this pain? Men have a difficult time understanding that even a lubricant and painkillers won’t help.
This is a chronic pain disorder with no known cause and no known cure. The pain is described in many ways, but the most common is: a burning pain.
Other descriptions include: stinging, rawness, aching, throbbing and sometimes itching.
Whatever perception of pain women may have from VV, it is certainly not easily remedied.
Is it possible that vestibular pain can be all in a woman’s head, perhaps from past sexual abuse?
The psychological and emotional affects that sexual abuse have on women are varied and far reaching.
There are cases of vulvodynia where a prior history of sexual abuse is notable.
However, sexual abuse is also associated with some aspects of sexual dysfunction such as dyspareunia (painful intercourse) and vaginismus (strong muscular spasms of the pelvic muscles with sex often preventing penetration and vaginal intercourse).
Is VV necessarily something that a woman has always had, since childhood (i.e., first becoming aware of it at age 13 when attempting to insert a tampon); or, can it sometimes just develop when she’s an adult?
VV can occur in women beginning with the teenage years. However, it is more common in women after the third decade of life and more so in the postmenopausal years.
Are there known treatments?
Just as there is no known cause to VV, there is no known cure. Here are some precautions and prevention:
Avoid harsh soaps, detergents, shampoos and chemicals on the vulva area.
Use cotton-lined undergarments and loose-fitting clothing Avoid scented and fragranced sanitary products.
 Dr. Nardone received her medical degree from New York Medical College and has been in practice as an OBGYN for more than 20 years.
Dr. Nardone received her medical degree from New York Medical College and has been in practice as an OBGYN for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/siam.pukkato
Birth Control Pills: Blood Clot Risk in Nonsmoking Women?
Women who don’t smoke take birth controls, and so do women who smoke–and they have a higher blood clot risk.
However, nonsmoking women are STILL at an increased risk for a blood clot simply due to the birth control pills.
You’ve often heard that birth control pills raise blood clot risk in women who smoke.
But what about blood clot risk in nonsmoking women who use birth control pills?
I wondered about this and asked Randy Fink, MD, Director of the Center of Excellence for Obstetrics & Gynecology in Miami, FL. I assumed that something inherent in the birth control pills raised blood clot risk for any female, smoking or nonsmoking.
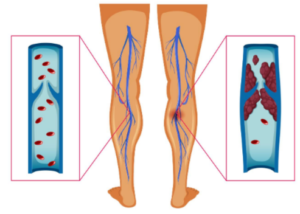
Dr. Fink explains: “Deep vein thrombosis and pulmonary embolus – a blood clot that travels to the lungs – are called thromboembolic events. Consider the rate of blood clots in women who are not on hormonal birth control.
“The common estimate is that it happens in 5 to 10 cases per 100,000 woman-years. {A more recent study even suggests it happens much more frequently: 50 to 100 cases per 100,000 woman-years.}
“On hormonal birth control, a clotting complication is said to occur in 20 to 30 cases per 100,000 woman-years. This is clearly higher than the 5-10 per 100,000 for women not on birth control.
“So, while the increase may seem frightening, the risk of these same clotting complications occurring during pregnancy is 60-96 per 100,000. During the postpartum period, it is 511 per 100,000 woman-years!”
Why is the blood clot risk so much higher postpartum?
“Pregnancy and the postpartum are associated with the classic risk triad for blood clots. First, blood ‘stagnates.’ Pregnancy changes the flexibility of blood vessels by making them swollen.
The pregnant uterus sits on and compresses the giant blood vessel that is the final pipe leading to the heart (the vena cava) from all the smaller veins. Blood therefore tends to pool.
“The swollen vessels sustain temporary damage, which is the second factor: injury to the muscular walls of these vessels. Finally, pregnancy itself is a hypercoagulable state.
There is a natural increase in several clotting factors, and a decrease in function of the systems our bodies use to break down clots.
A good explanation for this is so that the body does not form small clots that decrease the flow of blood (thus oxygen & nutrition) to the placenta & the baby.
“So, while birth control is not without risk (for blood clots), the risk of pregnancy itself is clearly much higher. Thus, hormonal birth control is said to be a safe way to avoid an unintended pregnancy.”
If, despite being a nonsmoker, you’re still concerned about blood clots because you are taking birth control pills, you can significantly lower risk of blood clots by:
1) exercising daily and including sessions of intense exercise several times/week, 2) ensuring your blood pressure is normal, 3) managing stress and 4) eating a plant-based diet.
Creating an environment where the very best of medicine and gentle gynecology are practiced and where patients come first has always been Dr. Fink’s goal.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Freepik
Painful Sex in Women: Vaginal Trigger Point Therapy May Help

Vaginal trigger point therapy can treat painful sex in women.
Painful sex for women has multiple causes. Sometimes, the pain during sex in women can be relieved by adding a vaginal lubricant, and prolonging foreplay to trigger more natural lubrication.
On the other hand, numerous conditions can cause a woman to experience painful sex.
A woman can have any one of these painful sex conditions, and yet benefit from a therapy called vaginal trigger point.
For this article I asked Randy Fink, MD, Director of the Center of Excellence for Obstetrics & Gynecology in Miami, FL, about just how effective vaginal trigger point therapy is for women who have pain during sex.
Dr. Fink says yes, vaginal trigger point therapy can help reduce pain during sex. He explains:
“Trigger point injections use a type of long-acting local anesthetic, sometimes combined with an anti-inflammatory such as a steroid, to alter the function of the nerves that contribute to certain types of pain syndromes.
“This is best described for women in one called Myofascial Pelvic Pain Syndrome (MPPS).
“The pain may occur in the pelvis, vagina, vulva, rectum, or bladder, or in more distant referral areas such as the thighs, buttocks, or lower abdomen.
“Commonly associated symptoms include a sense of aching, heaviness, or burning in these areas, sometimes with symptoms of overactive bladder, constipation, or painful sex.
Many experts believe that many, if not most, women with chronic pelvic pain have some degree of MPPS.”
How long do the vaginal trigger point therapy injections last?
“Anywhere from a few hours, to a few months, depending on what is being treated,” says Dr. Fink.
“Injections including local anesthesia and a steroid were studied in women with myofascial pelvic pain, and 72% still had relief at three months.”
Exactly where is the injection made?
“This depends on where the pain actually is. In the case of vulvodynia, they are made in and around the vulva, with specific focus on the pudendal nerve (4 and 8 o’clock positions).”
About how many injections?
“Again, depends, But usually 4-8.”
Is this therapy effective with vestibular vulvodynia?
“Can be. See above.”
Vestibular vulvodynia can cause significant pain during sex, as well as when anything is inserted into a woman’s vaginal orifice, such as a tampon, birth control device or even a swab for a Pap smear.
Additional Causes of Painful Sex for a Woman
• Injury to vagina or vulva from giving birth
• Sexually transmitted disease
• Menopause causing a dry vaginal lining
• Pelvic inflammatory disease
• Ovarian cysts
• Endometriosis
• Uterine fibroids
• Cervical infections
• Vaginal infections
• Vaginismus, which is when the vaginal muscles go into spasm due to a woman’s anxiety over sex or a Pap smear.