Thick Stools Suddenly Get Thin: Colon Cancer?

So many people are scared of seeing the so-called pencil-thin stools—even if the day before, their bowel movements were thick or fat.
“The reason that a stool changes from wide and then thin can be caused by what a person drank, ate or what environment they have moved to,” says Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
He continues, “It is an overall non-specific variable. If a person has a tumor, the stool can become thinner from obstruction, but this is NOT common.
“Colorectal [colon] cancer wouldn’t cause the thickness of stool to change, but a tumor in the lower anus or rectum could.”
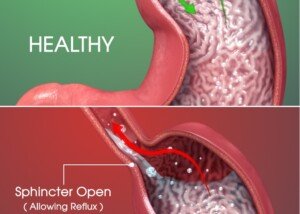
How does cancer make stools come out thin?
BMs come out the anus, which is of a certain width range when normal, allowing the stool matter to come out.
If there’s a cancer mass near the anus or rectum, then the bowel movements that are on the way out would have to go through a narrower pathway or channel, as the tumor would be obstructing the pathway.
The stools would then be compressed into a thinner diameter.
It’s the same principle when the opening of a tube of toothpaste becomes obstructed by dried, caked-on toothpaste.
You squeeze the tube hard, and the paste comes out with difficulty — and it’s much narrower than normal, because the hole that it comes out of is partially blocked by the dried toothpaste.
Dr. Binderow says, “Most persons will see their stools vary in thickness throughout their life, which is considered normal.
“Consistency of the stool and size are not as important as some [people] place on these changes.
“If a person is concerned, they should always discuss with their physician before drawing conclusions and to know what is normal and what to expect moving forward.”
Fear of Colon Cancer
With the increasing publicity about colon cancer, there’s an increase in anxiety over this in people who have taken to inspecting their stools.

Cologuard is a non-invasive screening test for colon cancer.
Cologuard uses the latest advances in bowel movement DNA technology, thus detecting the altered DNA from abnormal cells in the stool sample.
These cellular abnormalities may be associated with colon cancer or precancer.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
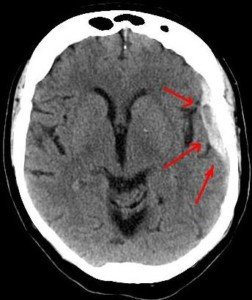
Ruptured Aneurysm Headache vs. Acute Subdural Hematoma

A headache expert describes the difference between ruptured aneurysm head pain and that from an acute subdural hematoma.
“Headaches related to ruptured aneurysm can be difficult to distinguish from that of a subdural hematoma,” says Noah Rosen, MD, Director, Northwell Health’s Headache Center in Great Neck, NY.
What a headache from a ruptured aneurysm has in common with the head pain from an acute subdural hematoma is that both are very intense — often described as a thunderclap headache.
However, in the case of a ruptured aneurysm, the thunderclap is more pronounced and sudden, like BOOM!
This is easy to understand when you visualize the aneurysm suddenly rupturing or bursting, spewing blood onto the brain.
“Thunderclap headaches are almost always a warning of some dangerous situation that requires immediate attention,” says Dr. Rosen.
“This can include bleeding such as that of a subarachnoid hemorrhage, intracerebral hemorrhage [hemorrhagic stroke] or epidural or subdural hematoma.”
The term, subdural hematoma, is not to be equated with chronic subdural hematoma.
In fact, the more specific term of the condition associated with a sudden, roaring headache is acute subdural hematoma.
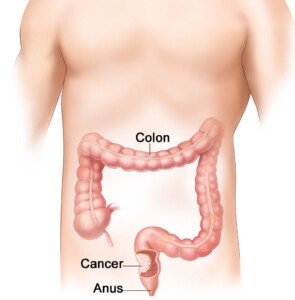
Subdural hematoma. Credit: Lucien Monfils
But often, the term “acute” is left out. “Acute” means sudden, as in head trauma resulting from going through the windshield of a car.
In the case of a chronic SDH, the bleeding in the brain is very slow—so slow that eight weeks may pass before the patient begins developing the first symptoms.
The symptoms are not immediately life-threatening in the chronic type.
In the case of my mother, her surgery to drain her chronic SDH was scheduled for the morning following her early evening admission to the hospital.
Her first symptom (a severe but non-thunderclap headache) came six weeks after hitting her head in a fall.
Dr. Rosen explains, “Acute subdural hemorrhage often presents as a thunderclap headache due to rapid expansion, irritation of local blood vessels and the meninges (or covering of the brain).”
Headache of a Ruptured Aneurysm
“They are also thunderclap in onset, are generally associated with more rapid loss of consciousness or other focal neurologic deficits,” says Dr. Rosen.
Whether ruptured aneurysm or (acute) subdural hematoma, both conditions require “immediate emergency evaluation and neuroimaging (such as a CAT scan) to determine the next course of action.”
The way these headaches feel to the patient, then, may be indistinguishable.
However, one of the hallmark features of an acute subdural hematoma is a type of vomiting called projectile.
An example: If a football player takes a very hard hit in the head and is walked off the field, sitting there on the sidelines dazed, and then suddenly vomits in a projectile path, chances are high that there is rapid bleeding in his brain. This is a medical emergency.
 Dr. Rosen’s career is dedicated to treating what he believes is an underserved patient population: those with migraine and other headache disorders.
Dr. Rosen’s career is dedicated to treating what he believes is an underserved patient population: those with migraine and other headache disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/KDdesignphoto
Can You Die Directly from Multiple Sclerosis?
A neurologist answers the question of “Can you die directly from MS?”
Anyone who has ever known someone who was suffering from multiple sclerosis may wonder if this autoimmune disease can actually be fatal.
Some patients are bedridden from this illness.
Many need a wheelchair to get around.
Can Multiple Sclerosis Kill?
“The disease is not fatal,” says Karen M. Blitz-Shabbir, DO, a neuro-rehabilitation and multiple sclerosis specialist based in Islip, NY.
She explains, “Most patients have normal life spans. Patients with advanced disease and disability can develop infections or other complications that lead to death.”
Infections and complications are potential secondary outcomes of MS, but multiple sclerosis, in and of itself, is not a directly fatal condition.
MS Complication that Can Be Fatal
Excessive bed rest, from being bedridden, can lead to a blood clot in the leg.
In fact, confinement to a wheelchair raises this risk as well.
There is nothing about MS itself that causes blood to pool in the legs and clot up. It’s the inertia of the legs that lead to this.
The name of such a blood clot is deep vein thrombosis. Excessive time in bed, regardless of condition (recovery from surgery, pregnancy, depression, mobility impairment) is a risk factor for a DVT.
This is why anybody who is bedridden from multiple sclerosis needs to have their legs, particular the lower portions, checked daily for signs of a DVT.
A DVT can break loose from where it has formed and travel to the lungs, blocking airflow, resulting in death.
Symptoms of a DVT
• One leg is suddenly swollen. This is often in the calve, but can occur above the knee.
• The leg may have a reddish discoloration. The color may also be pale.
• The leg may be unusually warm to the touch.
• The patient reports that it feels tender when touched.
• The calve area hurts or feels cramped up. This does not go away when seated or even lying down.
• These symptoms may also appear around and behind the knee, as well as in the pelvic area.
People with multiple sclerosis whose mobility is significantly impaired should ask their doctor about blood clot prevention.
 Dr. Blitz-Shabbir is also the medical director of rehabilitation with Holy Name Medical Center MS Center.
Dr. Blitz-Shabbir is also the medical director of rehabilitation with Holy Name Medical Center MS Center.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock, Chinnapong
Can Twitching Muscles Be an Early Sign of MS?
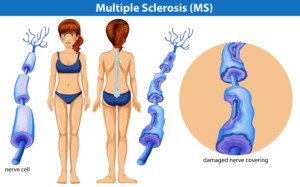
Many people wonder if twitching muscles might be an early symptom of multiple sclerosis.
Multiple sclerosis is an autoimmune disease that can render a person bedridden and comes with an assortment of possible symptoms.
“Twitching per se is not a common MS symptom and is not considered an early sign of MS,” says Karen M. Blitz-Shabbir, DO, a neuro-rehabilitation and multiple sclerosis specialist based in Islip, NY.
“Some symptoms that warrant investigation or consult with a neurologist include weakness, tingling, numbness, tremors.”
When I say “twitching,” I’m referring to fasciculations, or the kind of twitching that occurs in perhaps millions of eyelids every day.
These same kind of fasciculations also commonly occur in the legs, particularly after heavy exercise or activities like a long hike or hard time spent on cardio equipment.
People usually become aware of their twitching muscles when they are at rest, such as at a computer or when watching TV.
Somehow, some way, they come up with the idea that multiple sclerosis often, or just sometimes, starts out with these kinds of muscle twitches.
If you’re still worried that your muscle twitching signals an early symptom of MS, then here are the limb/muscle-related symptoms of this neurological disease (no particular order):
Weakness or numbness in at least one limb. Typically this happens on one side of the body at a time.
(Weakness and numbness are not to be confused with twitching muscles, and keep in mind that many, many conditions can cause numbness and especially weakness.)
Tremors. A tremor is not the same as a fasciculation-type muscle twitch. A tremor is a kind of shaking or trembling.
Tingling or pain in portions of the body, and/or fatigue that can’t be explained away by exercise, stress or side effects of a medication.
 Dr. Blitz-Shabbir is also the medical director of rehabilitation with Holy Name Medical Center MS Center.
Dr. Blitz-Shabbir is also the medical director of rehabilitation with Holy Name Medical Center MS Center.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: vecteezy.com
Source: mayoclinic.org/diseases-conditions/multiple-sclerosis/basics/symptoms/con-20026689
“My Giant Life”: Super Tall Women Nothing to Feel Sorry For

We all have struggles, and many people wish their biggest problems were finding jeans that are long enough and trying to squeeze into an airplane seat.
Meanwhile, I’ve always wished I were six feet, and envy women who are even taller than this (though my preferred height isn’t exactly “giant” caliber, yet at the same time—a little bit of me envies the women of “My Giant Life.” I don’t feel sorry for these super Amazons, especially since two play my sport, volleyball).
TLC’s “My Giant Life” focuses on four women ranging from 6-6 to 6-9, though one of the “women” is actually a 16-year-old girl who, at 6-6, may still grow another several inches.
“My Giant Life” is sure to be a hit show. What’s always stunned me is how women who are only (yes, “only”) 5-9 can feel self-conscious about their height.
I don’t get this. I was at the gym today. Even though I’m 5-8, I was dwarfed by one man after another in the free weight area. I don’t mean by muscle size, but by height.
So if a woman is 5-9, even close to six feet…she wouldn’t exactly stand out—at least not from where I come from.
And by the way, if someone asks if you play basketball because you’re so tall, don’t be a schmuck and ask them if they play miniature golf.
This is as old as the hills, and if it ever was a clever come-back, it certainly lost that zing decades ago. Be a good sport and give an honest answer.
If someone comments, “Gee, you’re so tall,” don’t be snarky by saying something like, “Oh, thank you for pointing that out; I had no idea!” After all, even very tall women are capable (as is the rest of the population) of pointing out the very obvious.
If you’re blessed with generous height, have you never pointed out the obvious before? Perhaps you commented to a stranger in the supermarket line with her preschooler, “Wow, your daughter has such curly hair!”
Chances are, you’ve said the following to at least a dozen women: “Oh, you’re so thin!”
Maybe you’ve said to someone in the park or on the sidewalk in your neighborhood, “Gee, your dog is huge!”
These are all examples of pointing out the obvious. Here’s another one that you may be guilty of: “Wow, your eyes are so blue!”
Yes, it could get very annoying, but that’s no reason for being a schmuckaroo. After watching “My Giant Life,” you’ll have a new perspective on your height.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Muscle Twitching: Is It ALS, Anxiety or BFS? Best Information!

Do twitching muscles have you terrified of ALS?
Then you need tons of reassurance, and I have it for you: a collection of the best muscle twitching articles that cover everything imaginable to help you through your ALS panic, fear, anxiety and sleepless nights.
This superb collection of muscle twitching articles was written by me, based on my own experience with a brief bout of muscle twitching fear that was brought on after I googled the wrong words and ended up reading some scary information on an ALS site.
The articles INCLUDE STATEMENTS FROM DOCTORS WHOM I INTERVIEWED.
Because I’m a writer by profession, I decided to write all about muscle twitching, benign fasciculation syndrome (BFS) and the accompanying ALS anxiety and panic.
Muscle twitching is technically known as benign fasciculation syndrome (BFS) if the twitching is accompanied by other symptoms such as tingling, cramping and soreness.
Twitching muscles, in isolation, are known as fasciculations. These fasciculations are not to be confused with restless leg syndrome, even though some types of muscle twitching can be described as “creepy crawlies” under the skin.
Everyone experiences muscle twitching, by the way. The difference between the people who are consumed with fear they have deadly ALS, and everyone else, is that, by sheer freak chance, on a bad day, the people in the first group googled “twitching muscles” or something similar, and found themselves glued to an ALS site.
The ensuing fear of having ALS can happen to just about anybody.
You CAN overcome it!
Read every one of my well-organized articles to help with your recovery. You will be so very reassured.
And if you have relapses, each will be less disastrous than the last, until eventually, relapses last only for 10 minutes, until finally, you’ll no longer have them!
I’ve reached a point where I just LOVE the feel of muscle twitching in my right hamstring, because one of the muscles has a slow-healing, running-related injury.
The “fascs” literally give it relief and feel like a mini-massage.
Any time you need reassurance that you don’t have ALS, refer to the information below for the specific assurance you seek.
You can once and for all conquer your fear of a disease that’s very rare.
Anxiety over having the beginning signs of ALS can be overwhelming, especially if you’re not sure how to visually identify atrophy of the muscles.
Another source of anxiety is that of twitching occurring in the same spot over and over and over.
This often involves an eyelid, but it can also involve a lip or an area near the lip, somewhere on the quadriceps (front of the thigh), the hamstring area (back of the thigh), and a thumb or calve.
A particular area that has many men and women scared out of their wits is their tongue.
Have you gone down a rabbit hole of fixation over your tongue, examining it througout the day?
Do you stop at every mirror you ever pass to inspect your tongue?
Do you try to hold it as still as possible but still see it twitching?
Does chewing food seem a bit difficult lately? How about forming words?
Are you constantly worrying that you have the bulbar form of ALS? Here is some reassuring information that you can really use!
The Thigh Dent
Here is yet another specific area of fear that some people have.
Somehow, someway, an individual has become overly focused on what appears to be a dent or indent in one of their upper legs.
It could be on the front or the side, and what’s alarming is that something similar is not on the other leg.
This is one of the most frightening symptoms for anyone who’s in the throes of ALS anxiety.
Knowledge of the facts is an unbelievable weapon against this type of anxiety.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
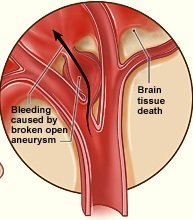
Chest Pain, Swallowing Hurts: Heart Attack or Esophagus Spasm?

Chest pain with painful swallowing can mean a number of things including heart attack in progress, heart attack in the near future and benign esophageal spasms.
About 200,000 people in the U.S. every year suffer from some kind of non-cardiac chest pain that may be accompanied by other symptoms like discomfort swallowing.
Dr. Ron Schey, a gastroenterologist at Temple University Hospital, recommends a specific treatment for chest pain that results from an issue with the esophagus rather than the heart: dronabinol.
Dronabinol is a drug that historically has been used for nausea and vomiting that result from chemotherapy.
Dr. Schey had a small group of people with non-cardiac chest pain (which can mimic a heart attack and cause severe anxiety) take five mg of dronabinol two times a day for four weeks, while other patients took a placebo.
Those on the dronabinol did better with tolerating their chest pain, and it was less intense and less frequent. Plus, there were no notable side effects.
Because this study was small, it’s not possible to compare how this drug works for non-cardiac chest pain vs. the current therapies.
Dr. Schey explains in his study report that dronabinol likely works by activating cannabinoid receptors in one’s esophagus, thereby reducing sensitivity. A larger-scale study is planned.
If you’ve been experiencing chest pain, even if there is some kind of difficulty or discomfort with swallowing, you should get a thorough evaluation at the ER to rule out a heart attack (a blood test will do this).
However…the blood test (which checks for leakage from damaged cardiac muscle of an enzyme called troponin) does NOT detect the presence or absence of clogged arteries!
“Troponin is a protein in the heart involved with contraction and relaxation of the heart muscle,” says Jack Wolfson, DO, FACC, a practicing cardiologist in Arizona, author of The Paleo Cardiologist: The Natural Way to Heart Health.
He continues: “If troponin is elevated, it is a sign of heart muscle damage. This is obviously not a good thing.
“But millions of people are walking around with extensive blockages, yet troponin is normal if checked.
“Again, elevated troponin is a sign that you may be having a heart attack.”
“Thus, if this blood test comes out negative, you should then follow up with your cardiologist.
“If all is fine, then the next step might be with a gastroenterologist to see if there’s an issue with your esophagus (which could be a spasm or acid reflux, among other issues) that’s causing the chest symptom.”
 Wolfson Integrative Cardiology specializes in functional medicine and provides treatment plans for out-of-town patients.
Wolfson Integrative Cardiology specializes in functional medicine and provides treatment plans for out-of-town patients.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/ShotPrime Studio
Source: sciencedaily.com/releases/2014/10/141021135018.htm
How Many Whole Eggs Are Safe to Eat Per Day?
A cardiologist explains how many whole eggs you can confidently eat in a single day.
Is it unhealthy to eat five whole eggs a day? Bodybuilders swear by eating lots of whole eggs, but what about cardiologists? Can too many whole eggs a day raise your bad cholesterol numbers?
“Eggs are one of nature’s perfect foods,” says Jack Wolfson, DO, FACC, a practicing cardiologist in Arizona, author of The Paleo Cardiologist: The Natural Way to Heart Health.
“It is like a multivitamin, containing everything a chicken needs to come to life,” continues Dr. Wolfson. “Hundreds of studies have proven eggs to be safe. In fact, eggs raise the beneficial HDL cholesterol.” HDL stands for high density lipoproteins.
Dr. Wolfson continues, “Eggs were vilified for many years because they contain cholesterol. But humans need cholesterol and it is beneficial to consume it. Times are changing, but many hospitals and doctors do not allow eggs for cardiac patients.”
This is so true. After my mother had her heart bypass surgery, I noticed that she was barred from ordering real eggs off the hospital menu.
The dietary staff knew which orders were being called in from the cardiac unit. Cardiac patients were permitted only the “Egg Beaters” type eggs—which actually is a synthetic goop that (in my opinion) hardly tastes like the real thing.
Hospitals, says Dr. Wolfson, instead serve pancakes with sugar-free syrup. “This is the source of the problem, and this lack of understanding keeps people coming back for more stents and surgeries.”
Pancakes are loaded with refined carbohydrates. These promote inflammation throughout the body and in the coronary arteries.
The body responds to this inflammation by building plaque in the arteries. The onslaught of sugars erode the inner wall of the coronary arteries. In simple terms, think of the repair process as the body shellacking these erosions—the shellac being plaque buildup!
“I recommend rotating foods, so every 3-4 days I will have 3-4 eggs as an omelet, scramble, egg salad and even raw. I always add plenty of herbs and spices when cooking to counteract any damage from cooking the eggs.
“Boiling eggs would not have a much oxidative damage from the heating process. And don’t forget, all of the nutrition is in the yolk.
“Those who order egg-whites only are depriving their body of precious nutrients and may actually be causing harm from doing something so unnatural.”
So back to the original question: How many whole eggs can you eat every day, then, since the cholesterol in them isn’t what actually harms the heart?
Dr. Wolfson explains, “A dozen eggs per week is not a problem according to most published studies. Therefore, 3-4 eggs per day however you like to prepare them is not a problem.
To avoid developing a sensitivity or allergy, I recommend eating eggs only 3-4 days per week at most.”
So there you have it: Enjoy your king-sized omelets (but spare the white flour and add in more vegetables like onions, peppers, mushrooms and spinach. Add in chopped walnuts for a unique addition of flavor and boost of nutrition.)
 Wolfson Integrative Cardiology specializes in functional medicine and provides treatment plans for out-of-town patients.
Wolfson Integrative Cardiology specializes in functional medicine and provides treatment plans for out-of-town patients.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Heart Palpitations During, After Eating: 6 Causes

“Many patients note heart palpitations after meals,” says Chester M. Hedgepeth, III, MD, PhD, Executive Chief of Cardiology at Care New England.
“The most common reason for this is dietary caffeine intake during mealtime which is found in many drinks, including coffee, tea, soda, and energy drinks and chocolate.
“Alcohol consumption during mealtime, especially if in moderate of high levels, can be associated with heart palpitations.”
Dr. Hedgepeth further explains, “Some patients may also have sensitivity to a particular food, or food additive like monosodium glutamate (MSG).
“Heartburn caused by eating spicy or rich foods can lead to heart palpitations.
“If you have heart palpitations after eating, it may not be directly related to the food but to the mealtime experience.
“Palpitations can be triggered by the simple act of swallowing, or if your mealtimes are a source of anxiety or stress.”
That last point is very compelling. For many people, mealtimes are a time of stress.
If you’ve been experiencing heart palpitations while you eat or “from” eating…take note of the conversation and emotions that take place during the meal.
Do arguments usually ensue?
Do the discussions revolve around stressful topics such as budgeting and saving money, negative experiences at the workplace or the in-laws’ upcoming visit?
Of course, if you have heart palpitations while eating alone, you may still want to assess your thought processes during this time.
When you eat by yourself, is this also the time that you worry about all sorts of things?
Can heart palpitations after eating mean anything bad?
“Usually, the palpitations after mealtime are not associated with any pathology and resolve on their own,” says Dr. Hedgepeth.
“Rarely, these palpitations can be associated with a cardiac arrhythmia.
“Progressive palpitations which are increasing in duration or which are associated with chest pain, shortness of breath or fainting should be evaluated by a physician.”
Preventing Palpitations “from” Eating
“The key to preventing the symptoms is to try identifying what the trigger is for them to occur,” says Dr. Hedgepeth.
“Certainly, reducing caffeine and alcohol intake will help prevent mealtime associated palpitations.
“Also, eliminating foods for which the patient may have a sensitivity or which contain additives (e.g., MSG) may help.”
MSG (monosodium glutamate, common in processed and restaurant foods) is a sodium salt, and consuming it in large amounts will contribute to increased sodium intake.
High sodium levels can affect blood pressure and heart rate, potentially leading to palpitations in sensitive individuals.
 Dr. Hedgepeth also serves as a physician in the cardiovascular division and arrhythmia service at Brigham and Women’s Hospital, plus is an instructor of medicine at Harvard Medical School.
Dr. Hedgepeth also serves as a physician in the cardiovascular division and arrhythmia service at Brigham and Women’s Hospital, plus is an instructor of medicine at Harvard Medical School.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Monster e
Acid Reflux: Chest Tightness vs. Angina, Heart Attack

Acid reflux or GERD can cause chest tightness, but how does this compare to that caused by a heart attack or angina?
“GERD is a disease where the esophagus is exposed to abnormal amounts of acid which is not designed to tolerate,” explains Jay Desai, MD.
Dr. Desai specializes in colon cancer screening, upper endoscopy and consultative gastroenterology with New York Gastroenterology Associates.
“The most common symptom is a burning sensation in the chest, which can also manifest as a tightening sensation.”
This sensation of tightness in the chest would, understandably, be quite frightening to anyone who knows that “tightness in the chest” is typically listed as a symptom of heart trouble, particularly that of a heart attack.
Dr. Desai continues, “It is important to note that this is just a symptom; the chest does not actually physically tighten.
“GERD symptoms can be confused with a cardiovascular event. Patients who are at risk for cardiovascular disease, i.e., people over age 50, tobacco smokers and those with family history of heart disease, should be evaluated for heart disease if they have these symptoms.
“If cardiovascular disease is ruled out, a trial of antacid medication should be initiated to see if it improves symptoms.”

A wedge pillow for acid reflux
GERD can also occur overnight or even shortly after going to bed.
What works for many people is that of elevating the upper body with a wedge pillow (one style is shown above), to help keep the stomach acids from creeping up the esophagus.
There are different styles of wedge pillows, and you may have to experiment with several before finding the one that’s the most comfortable for your sleeping habits.
You may also want to consider sleeping in a recliner chair.
Mattresses have not been proven to be the best sleeping surface for every single individual, and their horizontal shape is the last thing that someone with overnight acid reflux needs.

Board certified in internal medicine and gastroenterology, Dr. Desai provides a wide range of GI services including for bacterial overgrowth, constipation, acid reflux and GERD, IBS, incontinence and small bowel disease. Twitter handle: @NYGADocs
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.