Melanoma: Blistering Sunburn & Family History Biggest Risks

A dermatologist answers the questions you have about melanoma including appearance and vaccines.
I asked Ellen S. Marmur, MD, Chief, Division of Dermatologic & Cosmetic Surgery at Mount Sinai Hospital in New York, the following questions about melanoma, which kills close to 10,000 Americans every year.
Name the two greatest risk factors for melanoma.
Dr. Marmur: Family history (defined as greater than two first degree relatives with melanoma) and sun exposure (blistering sunburns in childhood).
Other risk factors: many moles; lots of sun-tanning; living at high altitudes; fair complexion, especially “peaches and cream” tone/blonde or red hair, blue eyes

We are always told to pay attention to the ABCDE’s of mole checking (asymmetry, border, color, diameter, and evolving).
This implies that a mole or body mark that’s smaller than a certain diameter isn’t anything to be concerned about.
The ABCDE’s have been a guideline for patients and doctors for many years.
Studies are showing that even regular-appearing moles can be more dangerous than irregular ones.
New or changing lesions (ulcerating, bleeding, itching) are the most suspicious. Continue using the ABCDE’s when doing self-skin exams—it’s still helpful and the routine of self exams is invaluable.
What percentage of melanomas spring up from pre-existing moles?
Unknown, probably the majority.
It is said that most DNA damage from the sun occurs before age 18.
Is this because it’s assumed that people get most of their sun exposure as children playing for hours in the sun, while as adults they are cooped up all day indoors?
Or is it because a child’s DNA is more vulnerable to damage than is the adult’s DNA?
Both, due to the amount of sun damage accumulated as children, plus the mechanism of carcinogenesis—which requires several insults to the DNA before it leads to unregulated cell growth.
The body is constantly holding these bad cells in check, using the immune system. Sun exposure impairs the immune system.
A sun damaged adult who gets more sun damage might lose the ability to fight off melanoma formation; whereas, a sun damaged adult who is careful might successfully fight off the melanoma.
Suppose a person has one blistering sunburn before age 18. Aside from that, only a few burns and as an adult, minimal sun exposure.
Is this person at all “screwed” just from one blistering event? How much risk can that one incident have in this particular case?
Unknown! Here is also where genetics probably plays a big role. Some people get skin cancer with very little sun exposure compared to others.
Though melanoma can appear anywhere on the body, does a blistering sunburn on one side of the body, increase melanoma risk on the other side that wasn’t exposed to the sun?
Probably, because that event causes full body immunosuppression. But unlikely.
What percentage of melanoma patients have darker skin?
More and more patients with skin of color are developing all forms of skin cancer.
Is it true that once melanoma reaches a certain size, it’s going to have a lot going on with it, like crusting, bleeding, oozing, weird colors, etc.?
Or can a melanoma be 5 millimeters and not have much visible abnormality to it?
New studies show that small size and regular colors and borders may still be high risk melanomas.
Large size however reflects a radial growth phase that is thought to precede the vertical, or invasive, growth phase.
It’s recommended that people do a mole check every month. How much can a melanoma change in appearance, from month to month?
The kinetics of melanoma growth are just being described. Monthly checks give the patient time to have a spot biopsied and treated hopefully before it becomes dangerous.
Once a person gets melanoma, will he or she likely be getting them all throughout the rest of his/her life?
One skin cancer (including basal cell and squamous cell carcinomas) means an exponentially higher risk of developing other skin cancers. Rarely is it a singular event.
There are cases in which a person was “cured” of melanoma, but then some years later, it “came back,” killing the patient. How is this possible if the patient does monthly self-exams?
The #1 site of origin of metastatic melanomas of unknown origin is the uvea inside the eye. Skin exams are necessary. Eye exams are necessary.
It is said that, if caught early, melanoma is 90-95 percent curable. What about the other 5-10 percent of early catches? Why would they be fatal?
Early melanoma is defined by its depth of penetration in the skin. In situ melanomas have a 100 percent cure rate at five years.
Minimally invasive melanomas may have single cell metastasis that are undetectable at the time of excision.
These have already started to circulate away from the skin and rely on the body’s immune surveillance system.
This is why a melanoma vaccine would change the world. When I worked on the melanoma vaccine I had the idea that if we could “personalize” vaccines for each person using their own cell “fingerprints,” it would be successful. Some researchers are attempting to perfect this idea, but it is for patients who already have melanoma.
Some dermatologists recommend that moles at least 5 millimeters in diameter be electively removed. Why doesn’t this recommendation begin at, say, 3 millimeters?
Sounds logical, but it would be a huge cost to insurance companies, and it may not pick up the small ones that look normal but are aggressive melanomas.
 Dr. Marmur has received rewards for outstanding research in melanoma vaccines.
Dr. Marmur has received rewards for outstanding research in melanoma vaccines.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sore Abs After a Workout: Three Things You Should Know

Just because your abs didn’t get sore, doesn’t necessarily mean that you didn’t work them effectively.
You may have worked them quite efficiently, but … due to these muscles being adapted to the routine, they didn’t respond with any soreness.
So how important is it for abs to get sore after an abdominal workout?
If your abs are sore after a workout that targeted these muscles, then this is a good indication that, indeed, you succeeded at targeting these muscles, and in a challenging way.
However, what if your abs don’t get sore after a workout (“after” meaning the day following)?
- Did the routine used to make your abs sore?
- And now they don’t get sore? Yes, the muscles have adapted.
It’s time to up the ante with the routine if you’re not satisfied with the results.
On the other hand, what if a workout has never made your abdominal muscles sore?

Shutterstock/FXQuadro
This often (but not always!) means that the workout was never effective in the first place. You chose an exercise routine that was never challenging.
In my case, I never experienced sore abs after doing cable crunches, yet this particular routine is amazing and gave me definition within 30 days.
So here was an exercise that never made my abs sore, yet produced results within a month.
And it continued producing more definition thereafter, plus greatly increased core strength. The cable crunch (when done properly) is probably the best exercise for the abs.
Do cable crunches right, and it doesn’t matter if you get sore.
If you’re not satisfied with your abs, then shock them with a routine that your body isn’t used to.
Force your body to re-adapt by imposing a movement or volume that the muscles aren’t familiar with.
You can up the ante by holding the sticking point for a 2-count before releasing.
If you do crunches on a bench, keep your hands off the bench for a change.
If this is too easy, place a light dumbbell between your feet, or a medicine ball between your lower legs, and see how the crunches feel.
Tuck in all the way; squeeze tightly into a crunch position before each release.
If you spend a lot of time working your abs, they probably won’t get sore.
You don’t need to spend a lot of time on abs to bring out definition and even a six-pack.
Overall-body training, with sound nutrition, will keep body fat stripped down low enough to reveal your ab muscles.
You can keep ab routines at the top of the training pyramid and still maintain core toning and strength.
Bottom line: Sore abs post-workout are not a marker for eventually developing a six-pack, and lack of soreness is not an indicator that you’ll never get that dream midsection, either.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/CHAjAMP
Treatment for Night Rotator Cuff Pain
Night pain from rotator cuff problems can be ugly, definitely enough to awaken people and keep them awake much of the night.
Certainly there has to be something you can do to minimize night pain from rotator cuff issues.
Night pain from rotator cuff problems is common, says Edmond Cleeman, MD, a board certified orthopedic surgeon who specializes in sports medicine and arthroscopic surgery of the shoulder, knee and hip.
“We tell patients to try not to sleep on that shoulder,” he explains.
“My experience has been that most patients are aware that they are sleeping on the bad shoulder, but habit makes it difficult to change.” Sleep on your back as much as possible.
Do not sleep on your stomach, as this is the worst position for the rotator cuff and is likely to bring on pain during the night.
“Most pain is if sleeping on injured shoulder, and when sleeping on stomach when arm is in a position over the head, such as arm under pillow.”
If you are unable to psych yourself into staying on your back, then position some pillows on either side of you that will prevent you from rolling over. Another option is to sleep on a couch or very reclined chair.
Keep your palms up, facing the ceiling, while in bed. To ensure they stay that way, tuck part of your palm-up hand under a pillow.
“The palm-up position leaves the joint space in the shoulder open, freeing up irritated rotator cuff tendons, giving them more room,” says Dr. Cleeman, founding member of TRIARQ, a community of orthopedists and physical therapists.
“Palms down reduces space in the joint cavity and can bring a frayed tendon in contact with bone.”
Night pain from rotator cuff problems can be minimized also by what you do for the shoulder during the day.
“Controlling the inflammation in the bursa can be achieved with anti-inflammatory medications (NSAIDS) or steroid injection,” says Dr. Cleeman.
“Some patients may not be able to take these medications and should check with their physician.
“Steroid injections can be very helpful and usually start working within a week.
“The steroid, a strong anti-inflammatory medicine, is injected into the inflamed bursa.
“Too many injections are to be avoided because it can weaken the remaining rotator cuff tendon tissue.”
In addition, if you’re struggling with rotator cuff pain in the middle of the night, then seek treatment from an orthopedic physician whose specialties include the shoulder. The doctor should prescribe physical therapy.
Rehab exercises should involve both stretching and strengthening, which your doctor or physical therapist can show you.
Furthermore, “A home exercise program is also essential,” says Dr. Cleeman.
“Using a heating pad before stretching or doing the stretches in a warm shower can help.”
 Dr. Cleeman is a highly experienced orthopedic surgeon and sports medicine specialist at Manhattan Orthopedics. He is committed to performing advanced minimally invasive procedures, allowing his patients to go home the same day.
Dr. Cleeman is a highly experienced orthopedic surgeon and sports medicine specialist at Manhattan Orthopedics. He is committed to performing advanced minimally invasive procedures, allowing his patients to go home the same day.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Ovarian Cancer Symptoms: Q & A with Doctor

Got questions about ovarian cancer you can’t find online the answers for?
Ovarian cancer is known as the “stealth killer,” because it silently stalks its victims without even giving the courtesy of an early symptom warning.
Today’s medical technology fails to effectively screen for this most deadly of all gynecological cancers.
Classic symptoms of ovarian cancer are: bloating, feeling full after small meals, gas, indigestion, low back pain, sometimes even leg pain, and weight loss but a growing stomach.
For this article I interviewed Dr. David A. Fishman, MD, a gynecological oncology surgeon with Weill Cornell Medicine in NYC.
Questions Answered about Ovarian Cancer Symptoms
When a woman begins developing symptoms of OC, is it possible she can be experiencing only one symptom for quite a while, or will multiple symptoms begin appearing at the same time?
Dr. Fishman: That’s a great question. Unfortunately, every woman will experience a different set of symptoms, and the question that arises is, “Are there symptoms that are unique to early stage cancer, versus early symptoms of advanced stage cancer?”
As we know, not all women have the same symptoms when they ovulate – it’s the same for ovarian cancer.
The problem we have is in determining if there are unique symptoms associated with only advanced stage ovarian cancer, or if there is a subset of symptoms associated with early stage cancer.
Is it possible to rank the symptoms of OC, in order of most common to least common?
It is possible to rank symptoms, but the symptoms are so varied, and the consistent symptoms that all would agree on are seen with advanced stage disease.
The majority of the symptoms that are consistent with cancer are due to tumor masses causing pressure, and associated signs and symptoms such as fluid in the abdomen, abdominal bloating, and weight loss.
My suggestion is that any woman experiencing abdominal discomfort for more than 5-7 days should have a thorough medical evaluation. In the course of the evaluation, the question should be asked: “Are my ovaries ok?”

Shutterstock/Emily frost
Many people will be seen by their family practitioner, gynecologist and internist, and each physician brings a different skill-set and focus on patient care.
If the cause of the discomfort is not found, I don’t think it’s inappropriate for a patient to ask, “Are my ovaries ok?”
Different doctors have a different focus. The best care a person can receive is by being a knowledgeable health care consumer and also being aware of their own body and what feels right and doesn’t feel right.
If their doctor can’t determine the problem, they certainly will be able to refer to the appropriate health care provider.
Would the symptoms necessarily be near-constant, continuous? Or can they be intermittent? Can they come and go, with days of normalcy in between?
The symptoms can be extremely variable and do not have to be persistent. It can be such a stealth disease – both to the patient and the healthcare provider.
It comes, it goes, it can be persistent, it can be intermittent, and it is almost always highly variable.
By the time a woman has symptoms, she usually has an advanced stage of the disease.
In the National Cancer Early Detection Program, we have found women who had no symptoms of cancer and had advanced disease.
I’m not saying that the symptoms don’t exist, but they can be extremely variable. Awareness is critical. If you don’t feel right, your ovaries must be formally evaluated.

Shutterstock/Olena Yakobchuk
We have evaluated over 8,000 women in our high-risk program with normal ultrasounds and normal examinations.
They were having prophylactic surgery (surgery done to prevent disease) because of their genetic predisposition placing them at a higher risk than the general population, which is a highly selective group.
Yet we found four women who had microscopic cancers in stage 1. These women had no symptoms, and two had cancer of the ovaries and two had fallopian tube cancer.
In our program, over 99% of women were normal, even in the very high risk group. We did multiple surveys to discuss various symptoms.
Surveys can be highly problematic, as there is a tremendous recall bias.
We found that most women with normal sized ovaries with early stage disease had no symptoms. Not even all women with advanced stage had symptoms.
But symptoms didn’t always correlate with the volume of disease. Some women can have horrific disease and feel fine, while others can have several small 1 cm nodules and be very symptomatic. The variability in symptoms is quite large.
The take-home message is if you don’t feel right, go seek appropriate medical care and ask your physician to include an evaluation of the ovaries, fallopian tubes and uterus.
Lower back ache is an OC symptom. Is there data out on what kind of pain this feels like (short of asking an ovarian cancer survivor)? There are different kinds of back “pain.”
Does it resemble menstrual lower back ache? Or more so the pain from a strained lower back from improperly lifting something? Or some other kind of pain?
If you have a mass pressing in your pelvis on the nerves, backache can be a vague symptom of the mass.
The ovaries in a pre-menopausal woman are about 2 inches in size – they are almond-shaped.
Also, inside the abdomen and pelvis are 23 feet of small bowel lying right on top of the ovaries, 9 feet of colon lying adjacent to the ovaries, and a uterus that is the size of a fist.
In the abdomen and pelvis, your ovaries are the smallest organ in size. Just by virtue of what’s in that area, ovaries are the hardest to detect.
That’s also why it is so common to misinterpret ovarian cancer symptoms for GI problems.
The pelvis is a bowl and the ovaries are very small. You can see why it can be such a diagnostic dilemma.
There is no specific type of back pain that I can tell you to look out for – the pain can be the result of poor posture, kidney stone or infection. It’s nondescript.
What percentage of OC patients experience vaginal bleeding?
Very few. Vaginal bleeding is not a symptom that is consistent with ovarian cancer. It is consistent with cancer of the cervix or uterus.
What kind of symptoms would a woman specifically have, that early OC would give off? I know that there have been a few studies focusing on “early” symptoms.
Yes, there are certainly symptoms – abdominal discomfort, frequent urination, change in bladder and bowel habits, losing weight while the abdomen is getting bigger, not being able to eat that much, fatigue, leg swelling – these are all signs of advanced stage disease.
The real question is, “Are there symptoms that are unique to early stage cancer?” We would make a tremendous difference in outcome if we could identify women with early stage disease.
Are there symptoms associated with helping us detect early stage disease before it spreads throughout the abdomen? The answer to that is, “I don’t know.”
The symptoms can be so varied and so subtle that the key is really being aware of your body, and if you don’t feel right and it persists for more than 5-7 days, go seek formal medical evaluation and make sure that includes a formal gynecological evaluation of the ovary.
That may be performed by a pelvic recto/vaginal examination or diagnostic imaging using a pelvic ultrasound, CT scan, MRI, whichever imaging study the healthcare provider feels would be the best evaluation for the symptoms.
The symptom of weight loss is a never quite clarified. Is the weight loss the result of the suppressed appetite? Or can it happen even if the woman continues to eat as she always has?
This is caused by the cancer itself; as it becomes more numerous, the tumor cells produce factors that suppress appetite, such as cachexia (weight loss in someone not trying to lose weight) factors. Factors from the tumors themselves suppress a person’s appetite.
Also, weight loss occurs, but the belly gets bigger. This is a symptom of advanced cancer.
Does the appetite suppression come on overnight, boom, like that? Or is it insidious?
None of these will “boom” overnight. Cancer is a living entity, and the symptoms are often a reflection of the volume of cancer growing in a person, none of which occur overnight.
Just as the cancer doesn’t become a detectable mass overnight, it can easily take several months to over a year before it is appreciated.
None should be an acute change. Some women come in and they’ve often had symptoms for a year, but they may perceive it as having happened over the course of 24 hours.
This disease is an act of God, not a disease that one can create. It’s not like smoking where you increase your risk…it’s a horrible disease that at present is not preventable, short of surgical removal of the ovaries as in prophylactic surgery. Unfortunately, as of today, it’s purely luck when you find it early.
Does the “bloating” sensation symptom ever occur in the upper abdomen? Or is it necessarily always in the lower abdomen?
No; the abdomen and pelvis are one giant cavity. The symptoms in the lower abdomen affect the upper abdomen. Imagine your belly having 7 liters of fluid – when you stand up it goes down and when you lay down, it goes up.
This is the symptom of fluid in the abdomen. There are many different symptoms while you are standing up and lying down.
Is there anything about OC symptoms that makes them uniquely different than symptom groups of other conditions whose symptom groups can mimic OC, such as irritable bowel syndrome?
If a woman has irritable bowel syndrome or diverticulitis, that makes it even harder to attribute her symptoms to ovarian cancer.
It could be a flare from GI disease or advanced ovarian cancer, and the symptoms can be similar.
Ovaries need to be included in the abdominal workup, and leave it up to your health care provider to determine the best tool.
I think even the most healthcare educated person who is the most knowledgeable about her body can easily be fooled by the symptoms of ovarian cancer.
That’s what makes this so difficult – none of the symptoms are distinguishable…where a patient can say, “I should’ve known,” when diagnosed in the late stage.
The main message is that if something doesn’t feel right, you should receive formal medical evaluation.
Is fever ever a symptom?
Fever can be a symptom associated with advanced disease.
Is there any medical impracticality or medical risk, for a woman, who’s not in a high-risk group, to have prophylactic ovary removal, so that she never has to worry about OC?
Assume she already has had children, or doesn’t desire any.
This is a highly controversial question. Certain women who are at very high risk due to inheritance of genetic mutations predisposing them for the development of breast, ovarian, colon and other cancers, may benefit from prophylactic surgery — but at what age?
This question must be answered on an individual basis with appropriate expert medical consultation.
The answer for some will be yes and for others will be no. It’s not an easy question to generalize.
Why is it so important that women be aware of the symptoms of ovarian cancer?
If symptoms are made more commonly aware, women can become better healthcare consumers. If you don’t feel right, make the ovaries part of the medical evaluation.
When a physician orders a CT scan of the abdomen and pelvis, the radiologist evaluates all components and organs; they look at everything.
The bottom line is that healthcare providers can provide much more effective medical care if they are aware of the symptoms associated with diseases.
If you feel fine, and a doctor does an exam and everything feels normal, it would be unlikely that a doctor would offer a CT scan.
However, if the patient’s complaints were not explained by the exam, further imaging studies would be suggested.
It needs to be a two-way discussion between the doctor and patient, where the healthcare provider and patient are working together as a team.
Hopefully, we can stimulate unification of patient and physician so ovaries are considered a routine part of the evaluation for abdominal/pelvic discomfort.
Our bodies are fascinating. As we develop new cancer specific blood tests, anything abnormal within our body produces unique proteins in the blood; which may be a new key to early detection.
We need further research and support to develop new techniques and validation of these tests to save lives.
Symptoms are wonderful at telling us there is a problem, but it would be far better to detect precancerous changes such that no one would develop ovarian cancer.
And that’s the goal of our program and the National Cancer Institute, to find changes before it becomes cancer, and save lives.
 Dr. Fishman is an internationally recognized gynecologic oncologist known for innovative research on the regulation of ovarian metastasis and the development of new methods for risk assessment and detection of early stage ovarian carcinoma.
Dr. Fishman is an internationally recognized gynecologic oncologist known for innovative research on the regulation of ovarian metastasis and the development of new methods for risk assessment and detection of early stage ovarian carcinoma.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Rocketclips, Inc.
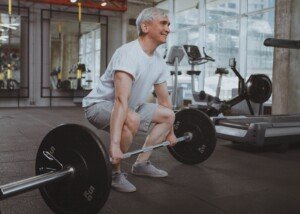
Why Can Fat People Lift Heavier Weights than Skinny People?

Here’s a reason why it seems that the fat people at a gym can lift heavier weights than the thinner people.
I was inspired to write this article after reading a question in a fitness forum that read something like, “Why do fat people lift more weight than skinny people?”
The answers were interesting, but nobody nailed what’s really going on here.
I’m a former certified personal trainer and have some answers.
It’s too general to outright state: “Fat people can lift more weight than skinny folks.”
To put it this generally implies that heavy individuals have much more overall physical strength than do lean people. This simply is not true.
First of all, the type of lift has to be considered.
Based on my experience as a personal trainer, very overweight individuals tend to lift more weight than skinny people, when they are matched for other variables such as experience in strength training, gender and age range:
- Leg press
- Lat pull-down
- Seated row
- Seated chest press
Other personal trainers may think the bench press belongs on the list, but if a person is overweight enough, the excess girth in their midsection will reduce the range of motion of the pressing movement.
This will allow them to handle more weight (the bar won’t come down as far because their large girth will get in the way).

Shutterstock/LightField Studios
I’ve also seen overweight women bench pressing the same amount of weight as thinner women — fatiguing at the same rate.
When a person is fat, their body is forced to work against this extra resistance just in the activities of daily living.
If someone is 100 pounds overweight, think of what the bones and muscles/tendons of their legs must put up with day in and day out.

All that extra poundage forces their legs to become more efficient at handling resistance.
Exceptions are the so-called “Walmart fat” people who appear to struggle with basic ambulation.
They are usually not much stronger than their smaller sedentary counterparts.
But for more active obese people, particularly younger, there is a carryover to the leg press movement.
The same principle applies to the lat pull-down, seated row and seated chest press.
So why doesn’t it apply to the barbell squat and deadlift?
Laura Phelps Sweatt is one of the strongest powerlifters around, yet has a low body fat percentage.

Laura Phelps Sweatt: Insanely strong, anything but fat.
Standing 5-5, she has competed in the 165 pound weight class as well as 181 pound.
But check out photos of her and see if you can find any excess fat on her body.
Many male and female competitive powerlifters with ridiculously heavy lifts to their credit are not fat.
Though the heaviest power lifts are never performed by “skinny” athletes, they aren’t what you’d call “fat,” either.
When Laura Phelps Sweatt weighs in at 181 pounds, she hardly looks like the average 5-5, 180 pound woman off the street. Nothing near it.
The strongest male powerlifters DO seem to have a noticeable amount of excess bodyfat, but keep in mind that in order to develop their strength (train like demons and grow super strong muscle fibers), they must EAT.
Unlike bodybuilders, they’re not concerned about their appearance.
To gain extraordinary strength they must ingest a caloric surplus.
But let’s get back to ordinary people working out in a gym.
Fat people struggle with many moves, but this doesn’t mean they can’t train hard, lose some fat in the process and become very good at powerlifting.
Some fat man or woman will struggle with the squat and deadlift because these are done while standing and require particular form.
Often, an obese man or woman has issues with their low back, which is another reason the deadlift and squat can be troublesome when attempting a heavy weight.
The farmer’s walk is no picnic, either. Hamstring curls and leg extensions are comparable to what skinny (but not malnourished) people can do, and in fact, fat trainees are more likely to have problems with their knees.
I recall two husky 20-something men I had as clients; both could barely press 15 pound dumbbells in each hand overhead for 15 reps.
Obese individuals do no better than thin or straight-size people when it comes to weightlifting moves such as lateral raises, frontal raises and triceps push-downs.
Barbell and dumbbell curls don’t stand out much either.
If you notice that the strongest people in the gym are fat, take a closer look.
The strongest people may be big, but that doesn’t mean Walmart fat, though that isn’t to say they can’t stand to lose some pounds in their guts.
Perhaps you’ve heard that “mass moves mass,” but at the same time, there are a LOT of obese and morbidly obese people out there who struggle just to carry the garbage to the trash bin, or carry a child to the car and then put the child in a carseat.
Another possibility is that an overweight person may passionately take up strength building simply because it puts them on an even playing field with thin people.
It offsets any despair they may have with their performance on a treadmill, on a hike, in a step aerobics class or a yoga class.
They’re under no perceived pressure to lose pounds if they take up weightlifting.
Their commitment pays off in the form of impressive lifting.
A very large lower body can also act as a more solid base of support for Olympic style lifts as well as the deadlift and back squat.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Source: atlargenutrition.com/athletes/lauraphelpssweatt
Why Bodybuilding Is NOT Bad for Your Heart

Ever wonder if bodybuilding is bad for the heart?
Some people believe that bodybuilding, or getting “too much” muscle, is bad for the heart.
But next time you see a man or woman with muscles big enough to make you stare…you must first wonder if it’s really possible that all that muscle mass could — for instance — cause plaque buildup in their coronary arteries.
If they have a lot of FAT with that muscle, then the problem is the fat, not the muscle. This is common in the world of competitive powerlifting.
Nevertheless, there are those who believe that the heart can be harmed by large amounts of muscle alone.
For purposes of this article, “bodybuilding” refers to lifting weights to add muscle mass, NOT the extreme preparations for cutting up for contest form (which involve severe dehydration and caloric restriction).
This article also EXCLUDES bodybuilders who take performance enhancing drugs.
This is about “natural” bodybuilders and other athletes who, via only natural means, have built significant muscle mass.

Are there studies that show that lifting weights is beneficial to the heart? Yes!
A report in Circulation: Journal of the American Heart Association says that lifting weights improves heart health.
The study’s lead author, Barry Franklin, PhD, states in the paper:
“We now have increasing evidence that weight training can favorably modify several risk factors for heart disease including lipids and cholesterol levels, blood pressure, body fat levels and glucose metabolism.”
You might be thinking, Okay, this refers to merely lifting weights.
- But what about bodybuilding?
- What about getting huge muscles?
The American Heart Association Science Advisory’s protocol for weightlifting is as follows: one set of 8-15 reps, involving 8-10 different routines, 2-3 times per week.
A devoted bodybuilder will work out a lot more than this, especially in terms of number of sets.
However, if the AHA protocol is followed at a very intense level, a person (if genetically endowed and on a supportive diet) can become quite muscular.
If a person chooses a weight load that makes 8-15 reps moderately difficult, he’s not going to develop the muscle that he would if he chose a resistance that makes 8-15 reps almost impossible.
Furthermore, rest time between sets, which has not been established in this AHA report, plays a key role in muscle development.
But no matter how intense someone adheres to this protocol, he will not become freakishly huge, though he may become quite muscular, enough to make a skeptic think that all that muscle is bad for his heart.
Another study shows that weight workouts lower resting blood pressure (Hypertension: Journal of the American Heart Association).
Lead author George A. Kelly, DA, says in the paper, “Even though these reductions in resting blood pressure are small, they still can decrease an individual’s risk for heart disease and stroke.”
Though these studies did not analyze bona fide bodybuilding regimens, one can deduce that taking strength training a few steps further into the bodybuilding realm will not cause damage to the heart.
This assumes that the individual does not have a congenital structural or electrical problem with their heart, or some pre-existing condition for which straining with heavy weight could cause a serious complication.

Shutterstock/Artem Furman
Smoking After a Workout
The idea by skeptics is that the substantial muscle mass adds so much weight to the body that these extra pounds will eventually strain the heart.
But remember, with the weight of lean muscle tissue from hardcore workouts also comes strong bones and joints and a sturdy back — to help support this weight.
A morbidly obese and sedentary person doesn’t have this advantage.

Body composition must be considered, not just absolute body weight. Shutterstock/Aleksei Zakirov
And just a reminder: The degree of muscle mass in question is that which can be attained via natural means, rather than with anabolic steroids.
Furthermore, what about the heart damage from smoking?
No joke, I have seen men smoking right outside the gym after a workout.
There’s death by smoking and death by obesity, but death by bodybuilding is unheard of — unless someone loses their grip on a 400 pound bench press…
Remember, excess body fat, a junk food diet, an inactive lifestyle and smoking are all major risk factors for heart disease. Any pamphlet in a doctor’s office will tell you this.
If you research risk factors or causative agents for coronary artery disease and congestive heart failure, you won’t find “bodybuilding” or “large amounts of skeletal muscle mass” in the lists.
Dr. Franklin says in the paper, “The more muscle you have, the higher your metabolic rate and the more calories you will burn each day.”
When low body fat is combined with muscle, it creates the illusion of more muscle than what’s actually there.
This makes details of their muscle more visible, creating the illusion in even milder bodybuilders that they have “too much” muscle.
Low body fat (in the “athletic” range) will not cause cardiac problems.
Who should avoid conventional weightlifting?
If you’ve been diagnosed with unstable angina, uncontrolled arrhythmias and uncontrolled high blood pressure, you’ll need to discuss strength training guidelines with your cardiologist.
People who’ve been diagnosed with spinal pathology, as well, should discuss weightlifting restrictions with their physician.
According to the American Heart Association, here are the risk factors for heart disease:
• Obesity
• Smoking
• Hypertension
• High “bad” cholesterol
• Hyperlipidemia (excess fat in the blood)
• Diabetes
• Chronic mental stress
• High fat diet
• Family history
• Lack of exercise
Additional Risk Factors
• High sodium (salt) diet
• Regular consumption of trans fats
• Untreated sleep apnea
• Insulin resistance
• Insomnia
• Sleeping under six hours a night
Where does bodybuilding, or having “too much” muscle, fit in here?
A lot of muscle does not lead to any of these risk conditions.
Men and women who work hard to get a lot of muscle are very conscious of healthy eating.
Though they’ll plan “cheat” meals, the bulk of their diet tends to be clean, that is, whole foods rather than refined, with substantial restrictions on white sugar, white-flour-based foods, saturated fats, trans fats and other junk ingredients.
If you’re still worried that bodybuilding is bad for your heart, even if your cardiologist has told you that your heart is in perfect shape, and everything else also checks out great — it would be wise to present details of your weightlifting regimen and goals to your doctor for a discussion.
2025 Study Links Sudden Cardiac Death to Male Bodybuilding
Sudden cardiac death (SCD) is emerging as a significant cause of mortality among male bodybuilders, particularly professionals, according to research published in the European Heart Journal (2025).
The study, led by Dr. Marco Vecchiato from the University of Padova in Italy, investigated the incidence of death and SCD among 20,286 male bodybuilders who had competed in International Fitness and Bodybuilding Federation events between 2005 and 2020.
This research is the first to quantify the frequency of sudden death within the bodybuilding world and shows that these athletes, especially professionals, are more than five times as likely to die from sudden cardiac events than their amateur counterparts.
Dr. Vecchiato notes that while bodybuilding promotes fitness and strength, it also involves potentially harmful practices.
These include extreme resistance training, rapid weight loss through dehydration and severe calorie restriction, and widespread use of performance enhancing drugs.
These behaviors, especially over long periods, can severely stress the cardiovascular system.
Of the 121 documented deaths in the study, the average age of death was 45. SCD accounted for 38% of these.
Additionally, around 15% of the deaths were classified as “sudden traumatic deaths,” including car accidents, suicides, murders and overdoses.
This suggests psychological stress and substance misuse may be contributing factors in the bodybuilding community.
Importantly, Dr. Vecchiato stresses that the findings are not a condemnation of strength training or fitness culture.
In fact, when approached responsibly (no PEDs, no dehydration, no starvation diets, no sodium depletion), strength training offers major health benefits including boosted immune function, a much lower risk of age-related bone fractures and a lower risk of some cancers, among so many more.
- To say that building muscle directly damages the heart is wrong.
- It’s the accompanying harmful behaviors that come with bodybuilding competition, particularly professional, that can cause cardiac damage.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ALL best fitness is HERE
Source: my.clevelandclinic.org/heart/prevention/exercise/strengthtraining.aspx
Quadriceps Tendonitis from Leg Extensions: Treatment

I injured the tendon that joins my quadriceps to my kneecap when I was doing ultra-heavy leg extensions.
I also figured out how to cure the “pain” at the junction of the tendon and quad muscle.
I didn’t go see a doctor because it wasn’t serious pain. As a former personal trainer, I was absolutely sure that it involved the patellar tendon. This tendon is used in the leg extension (“leg lift machine”).
So I self-diagnosed myself as having an injured quad tendon. The location of the funny discomfort was a dead giveaway to what was wrong.
The location was right where the tendon would be. Tendons join muscles to joints.
Secondly, I can differentiate between tendon pain and muscle pain. If you’ve ever had strained or injured tendons, you know what I’m talking about. The discomfort is unique, nothing like muscle discomfort.
It’s Easy to Overload Knee Joint with Heavy Leg Extensions
A common way of injuring a tendon is to overload it during weightlifting, which is exactly what I did.
As I was bringing my leg up during the extension, I suddenly felt this pain.
It wasn’t sharp like a knife, but it was very noticeable, and concentrated in a small area just above my kneecap.
Quadriceps muscles are very durable and strong. This was no quad injury. It was clearly the tendon.
When you injure a tendon, you almost always know it at the time of injury.
But when you strain, pull or over-work a muscle, oftentimes, you don’t feel it right away.
Guidelines for Healing and Restoring 100% of Your Tendon; Never Have Pain Again

Freepik
1) Initially you must avoid the activity that caused the injury. Take a few weeks off from it.
2) However, after a few weeks, return to the activity.
3) Be patient. It took three years for my injury to heal 100 percent. What this meant was that it stopped acting up — zero acting up.
The “pain” was more of a funny annoying feeling that would come during some activities.
But over a three-year period, the intervals between “acting up” times got longer and longer.
Currently, there is no activity that brings on the funny feeling and this includes heavy leg extensions. It’s all history. EDIT: Nine years after this post, there’s still no sign I ever had quadriceps tendonitis.
But this wouldn’t be possible had I not done certain things to heal it.
Realize that the best way to heal a tendon is to do the very thing you’d never think of doing: Resume the very activity that caused the injury in the first place: leg extensions.
However, resume it at a fraction of the resistance. When I resumed leg extensions, I used much lighter weight.
I used weight light enough such that it did not provoke the tendon or bring out that funny feeling.
I normally did leg extensions once a week, so my therapy, then, was once a week.
It’s possible the healing rate would have been faster at twice a week, but I opted to do the leg extensions only once a week.
Over a long period of time I increased the weights.
You might also note that every time you do the activity that caused the injury, you can feel the pain.
If the pain is dull and not that bad, use a lighter weight and gently work through it.
When I did this, the discomfort actually disappeared at some point during the workout.
If I had discomfort before the leg extension workout, then when I was finished, the discomfort was completely gone.
I surmise this was because the workout pumped up blood circulation and loosened things up. Inertia is the last thing you want to do.
My advice pertains to relatively minor tendon injuries. Obviously, if you think you’ve torn a tendon and there is swelling, you should see a sports med doctor. I had no swelling, redness nor acute pain.
Returning to the offending activity, but with lighter weights (and VERY light if necessary), high reps and patience, is the way to go.
Foot Position Is Important
Make sure your feet are always at a 90 degree angle, rather than “floppy” or relaxed when using the leg press equipment.

Note the foot position here; it’s incorrect. This can add strain to the knees. Toes should be pointed to the ceiling at the top of the movement. At the bottom of the movement, toes should be pointed slightly upward to ensure that at least a 90 degree angle is maintained. Freepik/jcomp
And when doing leg extensions, make sure the pad isn’t against your instep; this puts more stress on the knee joint.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Jasminko Ibrakovic
Shoulder Pain While Barbell Squatting: SOLUTIONS

There are different kinds of shoulder pain that can be associated with squatting with a barbell across one’s back.
The first type is a strained feeling, which may occur in one or both shoulders, soon after beginning the sets of squats.
It can be a sharp or pinching type of pain that tends to radiate down the medial (middle) deltoid.
The origin of this discomfort is a problem with the rotator cuff, a structure of four small muscles and tendons that is prone to injury from lifting weights, as well as from awkward positioning.
Though I’ve been a personal trainer, teaching the barbell squat, I have come across this problem only a few times — including with myself. But with myself, I found a solution.
Solution: Before you do barbell squats, stretch both shoulders by using the bar of a Smith machine.
Place it one increment higher than the height you’d normally use, if you were to do your squats on a Smith rack.
This height is important because it works perfectly for stretching the shoulders.
Position yourself beneath the bar as though you’re preparing to squat (even though the bar is one notch too high for your height).
Place hands as far out as possible on the bar. Place one foot ahead of the other as though you’re about to lunge, and lean body forward to generate a stretch in the shoulders. Hold for 30 seconds.
Rest from this stretch by doing anything (bodyweight squats, jumping jacks, sitting on bench, quad stretches, etc.).
However, after this 30 second break, you will start another 30-second stretch to help loosen up the rotator cuff.
Don’t force or yank the stretch; be gentle while you hold the position. Do four sets of 30-second stretches.
The joints should now be loosened up, and you can begin squatting (free or Smith).
Another possible cause of shoulder pain while squatting is that your hands are close to each other on the bar.

Place them further out. In fact, the further out they are, the less strain on the shoulder joints.
After the first set, you should do another 30-second stretch as described above.
In fact, after the first three sets of squats, do these stretches. By then, the joints should be thoroughly loosened up.
Another cause of shoulder pain during squats is that the bar is pressing down on the trapezius muscles.
This discomfort, for people who experience it, will be more pronounced during free barbell squatting versus that with the Smith machine.
The heavier the bar, the more pressure you’ll feel on your frame. However, make sure that the bar is truly across the shoulders, rather than resting upon your cervical discs!
If the bar rests on your neck, you’re asking for some deep trouble.
To avoid shoulder pain while doing barbell squats, 1) Decide you are going to take the time to conduct the stretches as described here, 2) Keep hands placed wide on the bar, even as wide as possible, and 3) Make sure the bar rests on the shoulders, not the neck.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/B-Media
Knee Pain & ACL Injuries: More Often in Women than Men

A doctor explains all a woman needs to know about knee pain, which affects women differently than it does men.
• Do you have a dull but annoying ache just underneath your kneecap?
• Does it worsen after jogging or going up a flight of stairs?
• Do you especially feel it when you lock out your knee?
• Do you feel the pain when you sit on the floor, leg straight out in front, and press your hand down on your kneecap?
• When you bend your knee, do you hear “grinding”? Do you feel a grinding sensation?
• Does jumping bring it on?
You just may have chondromalacia patella, a fancy name that means wearing down of the cartilage underneath the kneecap.
It’s common among fitness enthusiasts and sports participants who engage in jogging, running and jumping activities. Wear and tear from such activities causes the cartilage to soften up.
It then breaks down, causing irregularities along the joint surface, says Michael A. Schwartz, MD, an orthopedic surgeon with White Plains Hospital Physician Associates in NY.
“I usually describe to patients that normal articular cartilage is like the Teflon coating of our pots and pans, as it allows for the smooth gliding of our joint surfaces as we move them,” explains Dr. Schwartz.
“The condition of chondromalacia is similar to when the ‘Teflon coating’ wears off, and the gliding is less smooth.” This condition can affect other joints, but is most common in the knee joint.
Though people over 40 can get it as cartilage deteriorates with normal aging, younger people beware:
This condition can strike 22-year-olds, as the result of trauma to the knee sustained in something as simple as slipping on grass slippery from a recent rainfall, from playing volleyball or from jogging for exercise.
“It can occur in younger, otherwise healthy and athletic people,” says Dr. Schwartz, “when the articular cartilage softens in response to excessive pressure on the cartilage.
“Running and other joint-loading activities are often implicated. Chondromalacia usually develops over time, but it can also be precipitated from an acute injury.
“During such an injury, opposing cartilage surfaces can impact, or bang against each other, which undoubtedly causes some type of damage to the lining articular cartilage.”
A classic symptom of chondromalacia is pain right beneath the kneecap upon locking the knee out straight.
If you suspect chondromalacia, sit on the floor with both legs perfectly straight out in front of yourself so that you can’t even slip a piece of paper beneath your legs.
Place your fingers on the kneecap in question, and press down, as though attempting to hyperextend the leg.
If you have chondromalacia, the pressing-down will almost always cause pain. But if you don’t feel pain, this doesn’t mean you don’t have the condition.
It’s best to seek medical consultation just to be sure the pain isn’t from something more serious.
Treatment for chondromalacia is simple: leg extensions. They work absolutely wonders.

George Stepanek
Ice and rest provide only temporary relief, and do nothing to “train” the knee joint to be more reliable and efficient. But leg extensions will work magic.
“The worn-down cartilage cannot grow back and become smooth again,” says Dr. Schwartz.
“But the exercises strengthen the surrounding knee muscles, which can help in alleviating the pressure on the cartilage surfaces.”
If you’ve been diagnosed with chondromalacia, you must make leg extensions and other leg weight routines a permanent part of your life in order to keep the pain at bay.
And that’s not so bad a deal, because along the way, you’ll get toned, stronger legs that will always come through for you.
Preventing Chondromalacia
At first, you will need to minimize or even avoid joint-pounding activities, says Dr. Schwartz.
Activities that can aggravate or cause the condition include “running, especially on hard, unforgiving surfaces, squatting, kneeling, stairs and hill running.
“If one likes to do these activities for their conditioning, I always recommend cross-training, or varying one’s sports.
“With this, running should be alternated with swimming, elliptical machine work, bicycling, etc.”
Over time, as the knee’s surrounding soft tissue becomes stronger, it’s reasonable to expect a full absence of chondromalaciar discomfort. Other sports that can bring it on are soccer, lacrosse and field hockey.
Beginning-rehab Exercises
If you’ve never done leg extensions before, and you have this knee problem, then find a chair that’s high enough off the floor so that when you sit on it, your feet dangle.
Straighten the leg with the painful knee so that it is parallel to the floor, but avoid a full lock-out.
Hold for two seconds and lower. Repeat 10 times, three sets, three times daily. If both legs have the condition, you can extend both legs simultaneously.
Do this for several weeks, then graduate on to a weight stack machine, using the lightest weight possible. Gradually increase weight over time, and never quit these exercises.
If you quit, thinking you’ve “cured” the problem, don’t be surprised if within a few weeks, the pain pushes its way back into your life. Leg extensions with weights will keep the pain deactivated.
Exercise protocol for weights: 8-15 repetitions, 4-5 sets, twice a week. Never lock out knees.
Keep feet at a 90-degree angle to the shins at all times.
Do not let feet just flop around while performing the extensions.
Women far more likely than men to suffer ACL injuries.
Chondromalacia involves cartilage, a soft tissue that provides shock absorption for joints. On the other hand, ligaments connect bone to bone.
The ACL—anterior cruciate ligament—connects the thigh bone to the shin bone, and this ligament is somewhat shaped like a cross, hence its name, “cruciate” (think: crucifix).
ACL injuries aren’t just caused by a disastrous ski tumble. The ACL can be damaged from athletic maneuvers involving a sudden change of direction while the foot is planted, such as in volleyball, basketball and softball, even dancing or aerobics class.
Landing from a jump can also cause injury. ACL tears often require surgery—followed by up to nine months of rehabilitation.
It’s suspected that the way a female holds her trunk/hips during running and jumping activities, contributes to the higher rate of ACL injury.
Women tend to maintain a more erect posture than men, while running and jumping.
The next theory is that male athletes, more often than female, place their bodies in a protective squat-like position during athletics. Playing in a more erect position makes the ACL more vulnerable to harm.
Why men are more likely than women to do this isn’t clear, but female athletes should be trained to assume squat-positions more often during sports performance.
And if you’re not an athlete? You still should get in the habit of lowering your center of gravity during physical activities such as inline skating, trotting down staircases, hiking and even playing Frisbee.
A lowered center of gravity, while maintaining vertical spinal alignment, creates a protective effect against joint injuries and falling.
(Have you ever seen a skier standing erect while whooshing downhill? Have you ever seen a ski jumper land with straight legs?)
According to the American Academy of Orthopaedic Surgeons, here are a few explanations for why women suffer a higher percentage of ACL injuries:
- Biomechanical factors. Women tend to rely more upon their quadriceps during sports activities. A shift to more hamstring involvement can lower ACL injury risk. Women also more often than men land flat-footed rather than on the balls of their feet.
- Environmental factors. Shoes with high surface traction can increase injury risk.
Women will lower risk of ACL damage by learning more efficient techniques for landing, jumping and positioning their bodies during physical activities.
An exercise program that emphasizes upper leg strength and endurance will help the active female sustain the protective squat-like stance while engaged in sports or other pursuits such as trotting down a mountain trail.
Risk factors for knee problems in general:
- Overuse and/or improper biomechanics. This can occur from squatting excessively during gardening, for example. Prolonged kneeling with hamstrings against calves can also hurt the knee.
- Weak muscles and/or lack of flexibility.
- Mechanical problems like flat feet, misaligned knees, and one leg shorter than the other.
- High-risk activities like Alpine skiing.
It’s time to seek medical advice when the pain won’t go away despite rest and ice; the pain is severe; the knee is swollen or red; appears misshapen; and you can’t bear weight on the knee.
 Dr. Schwartz has previously worked as a team physician for high school, college and professional sports, and is the author of numerous scholarly research articles and chapters in orthopedic surgical textbooks.
Dr. Schwartz has previously worked as a team physician for high school, college and professional sports, and is the author of numerous scholarly research articles and chapters in orthopedic surgical textbooks.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Strengthen Your Ankles 10 Ways; Best Way to Treat Ankle Sprains

There are 10 distinct ways to strengthen the ankles — and the stronger your ankle joint the less likely you’ll suffer a sprain or weakened ligaments.
As a former personal trainer, I wasn’t just helping people lose weight and build muscle. I also showed many clients how to strengthen their joints, from neck to ankle.
10 Best Ways to Strengthen the Ankles
1. Walk forward and backwards on the balls of your feet.
Turn your toes inward as well.
You’ll actually feel this in the sides of your thighs, but you are also working the ankle joint, strengthening the ligaments that bind it together.
Go 50 steps forward, and 50 backwards. Do not hold onto anything when you go backwards. Just make sure you won’t bump into anybody.
2. Pedal a stationary bike with just the balls of your feet. Do not use the foot straps.
3. If you use an elliptical trainer, pedal with just the balls of your feet, and turn your feet inward a little.
4. Do seated calf raises with light weights and many repetitions.
Shutterstock/Jasminko Ibrakovic
5. Walk backwards on a treadmill. Do not hold on. Start out very slowly at first.
If you hold on, you’ll cancel out the effect that the routine is supposed to have in the first place.
The ligaments in your ankles need to support your entire body weight in a natural motion — the natural motion of walking backwards without your hands holding anything for support.
6. Take up jogging.
7. Do brisk walks on uneven surfaces, such as grassy areas. Go hiking on trails that offer a variety of terrain.

8. Take step aerobics classes.
9. Take up inline skating. It’s best to do this after you’ve been exercising your ankles for a while, since this activity will make ankles ache in people who are not very conditioned.
10. “A precise ankle adjustment followed by proprioceptive neuromuscular facilitation (PNF) exercises/stretches — which are implemented in the Power Kinetics® Home Exercise Program —may be the single most important factors in restoring optimal functionality and strength to your ankle/foot complex,” explains Eugene Charles, DC, Diplomate of applied kinesiology and author of “Journey to Healing: The Art and Science of Applied Kinesiology.”
How should you treat a simple ankle sprain?
“The number one way to treat ankle sprains — and the most overlooked — is that you must have the ankle bone (talus) realigned by a doctor of chiropractic or osteopathy,” says Dr. Charles.
“When you sprain an ankle your talus bone usually slips out of alignment, and this explains why people usually have weak ankles form then on out.”
The Compression Bandage
I have had superb results with using a compression bandage.
It’s amazing how effective these can be. I ice the ankle, if it’s swollen, several times a day for 20 minutes.
Do not ice for longer than 20 minutes, and let at least two hours go in between ice treatments.
Keep foot elevated as much as possible. And keep the compression bandage on at all times.
The kind I use is tight enough to force me to remove it after a few hours. After my foot has a break from it, I put it back on again.
HOWEVER … if at any point you begin feeling tingling or numbness from the bandage, immediately loosen it. There’s also no need to sleep in it.
I have restored mildly sprained ankles in as little as three days with icing and the compressive bandage.
Another option is the air cast, shown below.

BruceBlaus/CC
For more severe sprains, you’ll want to consider talus bone realignment.
Strengthening the ankles should be a priority for any athlete and fitness enthusiast.
We all know how much a sprained ankle interferes with activities.
Dr. Charles has helped thousands of patients and taught over 1,200 doctors during his 30+ years of practice. He has also created the Power Kinetics® Exercise Program and line of nutritional vitamins and performance supplements. amazon.com/Journey-Healing-Science-Applied-Kinesiology/dp/0964421763
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.