Does TIA health anxiety have you crippled with fear? Is every little headache, tingling or stumble a sign of a transient ischemic attack?
Learn how to conquer this.
You just had a sudden pain in your head that lasted a few moments. Right away you fear it was a TIA.
Or maybe every so often you feel tingling in some fingers, your forearm, your foot or in the back of your leg – and your mind always swings towards TIA territory.
Maybe earlier that day while in conversation you suddenly couldn’t think of the word you were trying to find.
You keep studying your face in the mirror to make sure one side isn’t drooping.
The list goes on and on. You know you’re gripped in the claws of TIA health anxiety.
TIA Health Anxiety
“Health anxiety is a huge issue, and I’ve always found it one of the most difficult problems to manage in primary care,” says Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
“Specific anxiety pertaining to TIA is not particularly common — much less common than cancerphobia or cardiac neurosis,” continues Dr. Beatty.
But it does happen, especially since nearly everyone has known someone who’s had a transient ischemic attack or stroke – and many have even witnessed the event.
For instance, my grandmother had a stroke while in my parents’ kitchen.
I’ve also witnessed a suspected TIA in my father twice.
For the first one he said it felt as though his body was pulling to one side as he walked, and he kept walking around the room, trying to figure out what was wrong. This sounded like the “one-side heaviness” that can be a TIA.
The next time, he had sudden double vision. Both events lasted only minutes.
And then I’d heard that my sister-in-law’s father had had a stroke.
Thankfully, I’ve never developed TIA anxiety, perhaps because I don’t have the risk factors for a transient ischemic attack or stroke.
However, even a person with healthy lifestyle habits can still fall prey to severe TIA health anxiety.
“Ninety percent of TIA’s affect the carotid artery distribution of the brain,” says Dr. Beatty.
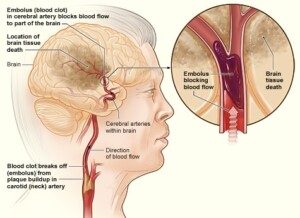
A TIA is a harbinger of a stroke. The American Stroke Association says that 9 to 17 percent of people who have a TIA will have a stroke within 90 days. Image: National Heart Lung and Blood Insitute
“TIA’s here will usually give symptoms of a ‘typical’ TIA — with weakness and/or sensory disturbance affecting a limb or the face. Partial visual loss may also feature.
“Seven percent of TIA’s affect the vertebrobasilar artery, which supplies the back part of the brain.
“The symptoms may be the same, but other less specific problems can occur.
“Vertigo, double vision, slurred speech, amnesia, confusion or loss of consciousness may feature.
“There are many other medical problems that can cause these symptoms, so they aren’t specific for a TIA.”
How is a TIA diagnosed?
“A TIA is usually diagnosed on the history — the patient’s testimony or the story given by a witness,” says Dr. Beatty.
“By the time a doctor attends, there’s often been a full recovery.
“There’s no test that will always definitely diagnose a TIA.
“Brain scans are often normal because the temporary blockage to the artery has cleared by the time the scan is done.
“It’s crucial for the doctor to get the best possible history with the timing and severity of any symptoms.”
Someone with true anxiety over transient ischemic attacks will likely already be documenting every symptoms, when it occurred, how long it lasted, etc.
“The patient should be asked what their ideas, concerns and expectations are,” continues Dr. Beatty.
“If these aren’t clearly stated, the consultation can be completely dysfunctional.
“The patient may be worried about a TIA when the doctor is talking about something else altogether.
“Once the concerns are identified, the doctor can target those concerns.
“It may be that the symptoms are common niggles that we all get from time to time.
“Many patients are just seeking reassurance from their doctor.”
How to Combat TIA Fear
“A good examination is reassuring. Blood pressure should be checked,” says Dr. Beatty.
Blood pressure at a doctor’s office may be higher than average due to anxiety.
You should take regular blood pressure readings at home with a home device.
“A normal heart rate and rhythm excludes atrial fibrillation (one cause of TIA and stroke).
“A normal sounding heart, free of murmurs, makes valvular heart problems less likely.
“Listening over the carotid arteries might pick up a bruit [pronounce brew-ee]– this is a noise associated with a buildup of plaque in the artery. Tiny pieces of plaque can flake off, causing a TIA.
“A full neurological exam will check whether there has been any residual neurological damage.
“A blood sugar check, to exclude diabetes, is worthwhile.”
Another avenue of reassurance is to go through a checklist of your actual risk factors, if any.
Also go through a list of all the good things you do for your body, such as regular structured exercise, low salt intake, high fiber intake, keeping a healthy body weight and not smoking.

It’s never too late to begin an exercise program. Freepik.com
What else can those symptoms be?
“It’s fairly common for people with high anxiety levels to keep returning to their doctor or move on to be seen by other doctors,” says Dr. Beatty.
“Many will be referred up for specialist assessment, and many will end up having investigations which they don’t really need.
“A normal brain scan doesn’t exclude a TIA, but it’s reassuring to exclude other problems.
“Up to 50% of suspected TIA’s have a different diagnosis.”
• Periodic waves of dizziness can be from BPPV: benign positional paroxysmal syndrome.
• The occasional tingling in a foot can be from a tight shoe.
• Tingling and numbness down the arm and into the hand can be from a compressed ulnar nerve (cubital tunnel syndrome) or median nerve (carpal tunnel syndrome).
• Occasional weakness in one arm and hand can be caused by a “pinched” nerve in the neck.
• Bell’s palsy could cause weakness or paralysis on one side of the face.
• Clumsiness on one side (e.g., your left foot missed a step on the staircase) can be an illusion: You simply missed a step; happens to everyone.
• That sudden loss of word you had when speaking to your sister-in-law? Your brain got transient sensory overload by being distracted by her eyes.
Of course, someone who’s at high risk for a TIA or stroke will find it more difficult to shake the ongoing anxiety.
If this describes you, then start working to eliminate the modifiable risk factors such as obesity, a sedentary lifestyle, smoking, high blood pressure, a poor lipid profile and use of illegal drugs,
Coronary artery disease is another risk factor.
To combat this, keep sodium intake to under 2,000 mg/day. Cut back on processed foods. Eat more fresh produce, nuts, seeds and fiber.
Another risk factor that actually gets less attention is untreated obstructive sleep apnea.
“There are lots of situations in medicine when there is a degree of uncertainty, and we all have to live with that,” says Dr. Beatty.
“If someone is struggling with that, then their anxiety levels can be assessed using the GAD questionnaire. GAD means generalized anxiety disorder.
“Those scoring highly on this might need to address the management options for their anxiety.
“All in all, a very difficult problem for patient and doctor.”
 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.