Why Can Ovarian Cancer Cause Leg Pain?

Ovarian Cancer Can Cause Leg Pain, but Why?
One of the symptoms of ovarian cancer can be leg pain.
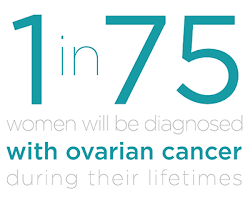
Ovarian cancer is the deadliest of all gynecological cancers, though it kills 14,000 to 15,000 women in the U.S. every year, striking about 20,000 women per year.
Ovarian cancer has been nicknamed the silent killer because often, symptoms don’t start presenting until this malignancy has spread outside the uterine cavity, sometimes not until it has spread to organs or distant sites in the body such as the breast.
Ovarian cancer’s symptoms are frequently misdiagnosed for more benign ailments such as gastrointestinal disturbances, the aches and pains of getting older, a musculoskeletal injury and even stress.
As for the leg pain being a symptom of ovarian cancer, I asked Randy Fink, MD, Director of the Center of Excellence for Obstetrics & Gynecology in Miami, FL.
He explains: “Presumably, growth of tumor in the pelvis may cause compression on one or more nerve groups.
Leg pain can be associated with any process that has potential to cause pelvic pain: uterine fibroids, benign ovarian cysts, ovulation, endometriosis, or even just routine period cramps.”
In addition to leg pain, the symptoms that have been caused by ovarian cancer are (no particular order):
Abdominal bloating (increase in size)
Sensation of abdominal bloating
Suppressed appetite or feeling full after small meals
Back pain
Stomach pain or upset
Pelvic pain or discomfort
Feeling of heaviness in the pelvic area
Unexplained weight loss
Unexplained fatigue
Constipation and diarrhea, especially alternating
Feeling the urge to void though nothing comes out.
Though about 90 percent of women with newly-diagnosed ovarian cancer are over age 50, younger women should have their ovaries examined if they present with the previously mentioned symptoms.
If you’ve been experiencing any of those symptoms for longer than a few weeks, see your gynecologist and request to have a complete exam of your ovaries.

The premier ovary exam is the transvaginal ultrasound. Shutterstock/Doro Guzenda
Some young women, who’ve had ovarian cancer, were told by their doctors that they couldn’t possibly have this disease because they were “too young.”
This statement assumes that 100 percent of newly diagnosed ovarian cases occur in older women.
Women in their 20s can get ovarian cancer, though this is rare.
In fact, here is the age bracket breakdown for the period 2002-2006 (National Cancer Institute):
Average age of diagnoses: 63
Dx over age 85: 7.6%
between 75-84: 19%
between 65-74: 19.9%
between 55-64: 22.3%
between 45-54: 18.9%
between 35-44: 7.4%
between 20-34: 3.5%
under 20: 1.3%
It’s impossible to say that leg pain can ever be the only symptom of ovarian cancer.
A woman with these symptoms that persist should have a thorough gynecological exam.
Creating an environment where the very best of medicine and gentle gynecology are practiced and where patients come first has always been Dr. Fink’s goal.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Albina Glisic
Should You Be Scared when Your Heart Flutters?

When the heartbeat does what you’d describe as flutters, these are “usually called palpitations, which represent an awareness of our heartbeat (it may be described as an irregular beat, a forceful beat, or a rapid beat),” says Teresa Caulin-Glaser, MD, a cardiologist and senior vice president with Service Lines, OhioHealth.
A fluttering heartbeat can be frightening, even if you’re young and athletic, but especially when you’re not so young anymore and not in the best shape.
Dr. Caulin-Glaser continues: “There are multiple causes of palpitations (arrhythmias, structural heart problems, medications, recreational drug use, caffeine, stress, metabolic disorders).”
If your fluttering heartbeat is being caused by anxiety or stress, worrying about this issue will likely exacerbate the fluttering, but this won’t cause any damage.
You’ll find that during periods when you realize your heart was not fluttering, you were calm, cool and collected, and the issue was the furthest thing from your mind.
Exercise is a great way to subdue general anxiety.

Freepik.com, prostooleh
Dr. Caulin-Glaser explains: “Most often palpitations are not a concern and are a result of premature heartbeats.
“The heart feels like it is flip-flopping in the chest, sometimes with a sensation that it has paused.
“This sensation is the result of the premature beat causing a brief pause in the heart rhythm.
“If the symptoms are frequent, increasing in duration, associated with symptoms, they should be evaluated.
“This would initially involve a very careful history, physical exam, 12-lead ECG, labs and ambulatory monitoring of the rhythm.”
If your fluttering heart is accompanied by symptoms such as feeling like you’re about to pass out, lightheadedness or chest pain, you should schedule an appointment with a cardiologist.
It would also be a smart idea to keep a log of your heart fluttering episodes.
This way you can determine if there is any pattern, such as the problem occurs only when you are experiencing substantial anxiety; during or shortly after physical exertion; or whenever you take a certain drug, such as diet pills, cold and cough medications, amphetamines and cocaine.

Dr. Caulin-Glaser is an experienced physician, teacher and researcher in the specialty of cardiovascular disease, and formerly the system vice president for Heart & Vascular Services at OhioHealth.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Monster e
Does Slow Resting Heart Rate Mean Low Heart Disease Risk?

Does a slow resting pulse mean you don’t have heart disease?
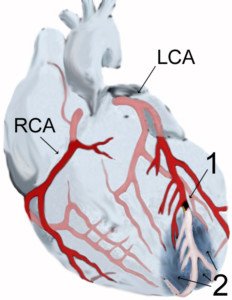
Think again if you believe your slow resting heart rate means you can’t possibly have heart disease – even severe heart disease, also known as coronary artery disease (CAD).
A heart with heavily clogged arteries can still have a consistent beat of 60-something or 70-something per minute.
“A low resting heart rate does not preclude CAD, nor does a low blood pressure,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“The vast majority of coronary disease patients are hypertensive (high blood pressure), but those with normal or low blood pressure are not protected.”
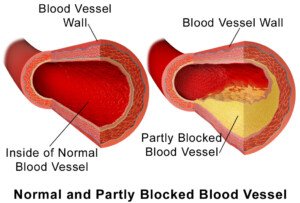
BruceBlaus
I’ve witnessed this myself, in that my mother’s resting heart rate was consistently in the high 60s, sometimes into the 70s, yet she ended up needing quintuple bypass surgery after a catheter angiogram revealed five major coronary arteries to be almost completely blocked.
She had the “slow” resting heart rate right up to the time of surgery.
Almost daily she’d take her blood pressure at home with a little device, and it would show resting heart rate. Her blood pressure was also consistently in the normal range.
Between the slow or “normal” resting heart rate, and the normal blood pressure, my mother was convinced she couldn’t possibly have heart disease.
Dr. Fiocco explains, “Although a low resting heart rate has in the past been a marker of someone who was healthy and fit, a much better measurement is what is called your recovery heart rate.
“In other words, how quickly your heart rate returns to normal after maximum exercise.

Freepik.com ijeab
“If your heart rate drops more than 30 beats, and in the most fit, 50 beats, within two minutes of stopping max exercise, you are considered healthy and at low risk for CAD.”
My mother’s resting heart rate was slower than mine, but pre-surgery she’d get audibly out of breath simply by hurrying to answer the phone in another room; whereas I could sprint across a parking lot in the rain, my baseline heart rate faster than my mother’s.
Yet at the conclusion of the sprint, my heart rate would hardly be elevated and I would not be out of breath.
“Back to the low or normal blood pressure patients,” continues Dr. Fiocco.
“Most are taking better care of themselves, and are less likely to have CAD.
“But there are exceptions and we see patients all the time with normal blood pressure who smoke and have diabetes or a strong family history of CAD, who themselves have CAD.”
Don’t let that slow resting heart rate or low blood pressure fool you; this does not mean you can’t have heart disease!

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image credit: Szlomo Lejb
sscpywrt26
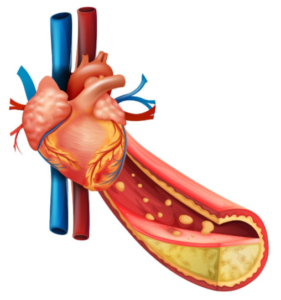
How Much Coronary Artery Blockage Causes Angina?
How much blockage in the coronary arteries is needed to cause angina?
You can have sludge built up in your arteries and not know it.
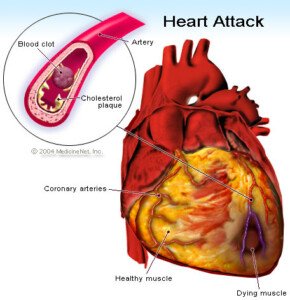
Angina is chest pain from blocked coronary arteries, which restrict blood flow (and thus oxygen) to the heart.
I wondered, however, just how blocked that coronary arteries need to be, in order to cause the symptoms of angina.
“The amount of blockage in an artery needed to cause angina is complicated due to flow dynamics and how the narrowing is measured,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Simplistically, anything over 50 percent is significant and may cause angina with exertion.
Source: vecteezy.com
“Once the narrowing reaches 75-80 percent or more, angina may occur at rest (known as unstable angina). Again this is a general rule and is different from person to person.”
Have you had chest pain during working out or immediately after, that very rapidly disappears?
This can be caused by inflammation of the cartilage in the rib cage (costachondritis).
It can also be caused by the effects of momentary exertion of the chest muscles, such as in a hardcore set of pushups or flyes.

Finally, what can be described as chest pain during or immediately following a sprint or other brief burst of maximal activity could be chest muscle fatigue or soreness from strained, deep inhalations.
This can also happen as a result of arguing if it involves a lot of tension-filled deep breaths in between a hollering match during a heated argument.
But this isn’t chest pain per se, but rather, a sensation of chest fatigue or mild soreness.
Can you have a coronary artery blockage of over 90 percent and yet experience no angina upon exertion?
Dr. Fiocco explains, “Yes, and many people do. If the artery occludes over a long period of time, your heart and body adjust and no symptoms, sometimes even if the artery is occluded.
“Collateral circulation, small capillaries which enlarge and reverse flow, will get some blood to the compromised [heart] muscle to keep it alive and prevent angina.
“This system of collateral circulation will not suffice when more than one artery becomes narrow.”
Can you have a coronary artery blockage of under 50 percent, say, 40 percent, yet experience angina upon exertion?
“No. Either the ‘angina’ is coming from another source, or it is truly angina and the degree of narrowing is being underestimated.”

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
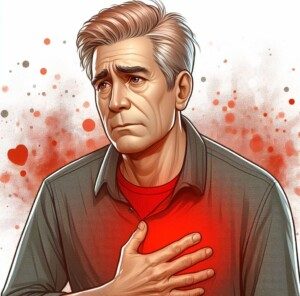
How Not to Miss Warning Signs of Future Heart Attack

You’d better believe that warning signs almost always exist for future heart attack.
The warning signs are there; you just have to know how to spot them!
A heart attack is serious business; how could this not have warning signs?
Is calling coronary artery disease “the silent killer” misleading and inaccurate?
Here is what a doctor says, regarding warning signs of a future (not imminent) heart attack:
“Not 100 percent, but 98 percent of people are getting warnings they ignore,” begins Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Short of breath, shoulder pain, fatigue, etc., are what we call ‘angina equivalents.’ The human brain has a remarkable ability to deny.
“Can’t tell you how many patients I ask if they have had any chest pain who say, ‘No,’ who five minutes later will say, ‘Well, I did have some tightness,’ or, ‘I did have some pressure,’ but it wasn’t chest ‘pain.’”
Some warning signs that a heart attack lies in wait down the road may seem quite innocent, while others are scary, like chest pain and shortness of breath.
However, denial is rampant even among, as Dr. Fiocco says, people with chest discomfort.
If you’re tuned into your body, you should be able to detect when something isn’t right.
If you’re familiar with all the possible warning signs of future heart attack, then your coronary artery disease won’t be so “silent.”
Did you know that shoulder pain can be a warning sign of future heart attack? Few people make this connection.
But what about the more obvious, like shortness of breath and fatigue?
Well, there’s a problem here, too: These are built-in symptoms of aging in a person who doesn’t exercise!
My brother’s coworker, for several years, had noticed a decline in energy, increased fatigue, and shortness of breath. The middle-aged man chalked it up to getting older and lack of exercise.
He never considered that these symptoms were warning signs of a future heart attack. He had the heart attack and underwent quadruple bypass.
Fast-forward well-beyond total recovery: This man scuba dives and says he feels 20 years younger!
Did you know that insomnia or trouble sleeping in older women can be a warning sign of future heart attack?

Shutterstock/Supawadee56
Few people make this connection. Feelings of impending doom (for no apparent reason), plus panic attacks, can also signal a future heart attack in women.
Coronary artery disease does not progress overnight.
Because of the slow progression, it mimics the aging process, especially in people who already know they’re out of shape due to lack of exercise, overweight or smoking.
Of course I’m short of breath, the obese person or smoker might think, or someone who never exercises will conclude.
Of course I’m short of breath, a 60-year-old may reflect while huffing and puffing up a short hill. I’m not as young as I used to be!
Chest pain has many causes including indigestion. A person with a big appetite may easily pass chest pain off as heartburn.
A chronically stressed-out individual may attribute chest pain or tightness to anxiety, especially since anxiety and stress are common causes of chest discomfort.
So how do you differentiate warning signs of future heart attack, from normal signs of aging, stress or effects of overweight, smoking or indigestion?
A soft-plaque rupture; can cause a heart attack. Shutterstock/Diamond_Images
The person with unhealthy lifestyle habits really can’t, if the symptoms are things like:
- Shortness of breath (which can be caused by gastroesophageal reflux disease)
- Fatigue
- Chest discomfort
- Shoulder pain (which, if caused by coronary artery disease, can easily masquerade as a rotator cuff problem or arthritis in someone with past legitimate shoulder problems).
It’s much easier to realize that something is wrong with your body if you’ve always performed strenuous exercise, and then for no apparent reason, find your performance deteriorating.
But the more out-of-shape you are, the more that warning signs of future heart attack will fade into your profile and be camouflaged by the aging process, stress, excess weight, poor sleep (of course I’m tired all the time!), etc.
Make an appointment with a cardiologist and tell the doctor your symptoms, no matter how trite they may seem.
Inquire about imaging tests and stress tests.
A cardiologist cannot rule out imminent or future heart attack based on only an EKG, stethoscope exam, feeling your chest, blood pressure reading, heart rate, absence of family history of heart disease, absence of personal history of smoking, or some questionnaire about your eating and exercise habits!

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: Shutterstock/igorstevanovic
Thumping Heartbeat Causes, Solutions, When to See Doctor
Is your thumping heartbeat scaring the daylights out of you?
Does your heart go ba-ba-BOOM, ba-ba-BOOM for no apparent reason?
Ask yourself these questions:
Does the thumping, extra or irregular heartbeat usually come when you’re not exercising?
Are there no other symptoms with it?
Do you feel fine otherwise?
And, do you find that you are most aware of a thumping or extra heartbeat when you start thinking about it?
If so, anxiety is usually to blame.
Nevertheless, heart health should always be taken seriously, which is why I asked questions about thumping heartbeats to Dr. Frederick Ehlert, MD, cardiologist with the Cardiac Electrophysiology and Pacing division at ColumbiaDoctors Eastside, NYC.
Is there a way to tell when a “thumping” heartbeat is stress related, versus indicative of a serious condition?
Dr. Ehlert: It’s hard to know what is meant by “thumping,” and the context of the sensation is also important.
a) It could simply mean feeling your heart beating. This assumes the heartbeat is the normal one, at normal rates, but that the person simply feels the heart beating in the chest.
This could be due to a heightened awareness of the heartbeat or the heart contracting more vigorously than usual given the person’s level of activity (i.e., it would not be abnormal to feel this after physical exertion.) This would not be dangerous.
b) It could mean the sensation of a skipped or irregular beat, sometimes described as a “thump.”
As stated, these extra beats come early, arise from either the top (atria) or bottom (ventricles) chambers of the heart. As isolated phenomena these are not usually dangerous.
c) It could mean the sensation of a rapid abnormal heartbeat called an arrhythmia.
An arrhythmia, like the isolated extra beats, can arise from either the top or bottom chambers of the heart.
Depending upon where they arise, what sort of heart disease (if any) they are associated with and what symptoms occur (in addition to the sensation of “thumping”), some arrhythmias can be dangerous.
None of these are what is typically called “having a heart attack,” which is associated with blockages in the arteries supplying the heart with blood.
The symptoms associated with a heart attack can be pain (usually in the chest but occurring anywhere from the jaw to the belly button), nausea, sweatiness, and/or shortness of breath.
Why is it that a person, under stress, is more likely to experience the thumping and skipping, while seated and at rest, versus while moving around, especially exercising?

Shutterstock/Prostock-studio
An uptight person will feel the thumping while watching TV or at the computer, but it won’t be there while they’re walking up a hill.
I am assuming that “thumping” refers to either a or b above. This occurs under stress because levels of adrenaline (and substances like it) can go up with stress.
Adrenaline can make the heart beat more vigorously, hence the sensation of feeling it beat, or may trigger the extra beats referred to above.
Several things can explain the phenomenon described in the question.
Often, when a person is sitting still, they are more likely to experience thumping because their mind is not focused on other things.
In addition, with exertion the heart should beat more vigorously, so a person is less likely to feel abnormal.
Also, extra beats may be suppressed when the normal heartbeat goes faster (as it does in exercise).
When someone has a thumping heartbeat, what would have to signal that it’s time to make a doctor appointment (short of the jaw pain, sweating, etc.)?
Is there a type of thump that means heart ailment?
The symptoms I described above that are frequently associated with a heart attack, should be evaluated immediately.
In addition, associated lightheadedness, dizziness, fainting or near-fainting should also be evaluated.
If the “thumping” is troublesome, occurring frequently or impacting the person’s ability to work or play as they wish, they should probably be evaluated in a non-emergent fashion.
A physician will try to identify the heart rhythm underlying the person’s symptoms of “thumping” and institute some form of treatment (cardiac or otherwise).
The premature heartbeat can also be triggered by nicotine, caffeine, gas and fatigue.
A thumping, fluttering, extra or “skipped” heartbeat can also be caused by (no particular order): mitral valve prolapse, hyperactive thyroid, electrolyte disturbances, smoking, alcohol, lack of sleep, and this can’t be said enough: anxiety, especially over a thumping heartbeat.
 Dr. Ehlert’s areas of expertise include sudden cardiac death and heart rhythm disorders. He has authored over 40 peer-reviewed papers, reviews and book chapters in electrophysiology.
Dr. Ehlert’s areas of expertise include sudden cardiac death and heart rhythm disorders. He has authored over 40 peer-reviewed papers, reviews and book chapters in electrophysiology.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Top image: ©Lorra Garrick
Chest Pain & Shortness of Breath: When to Visit ER
Having chest pain and shortness of breath and wonder if this is an emergency?
Chest pain and shortness of breath can signal an impending heart attack.
Chest pain and shortness of breath can also be symptoms of panic or anxiety attack, or gastroesophageal reflux disease.
Chest pain and shortness of breath may also mean asthma, bronchitis, inflammation of the lining of the lungs, allergies, sleep apnea and more.
So when should you make a trip to the emergency room if you’ve been feeling chest pain and having shortness of breath or labored breathing?
Let me tell you about my mother, who underwent quintuple bypass surgery the day after going to the emergency room with chest pain and shortness of breath.
Obviously, it would be impractical, and a sorry life to live, if every single time you had chest pain or discomfort, you zoomed to the nearest emergency room.
Chest pain can also be caused by damage to rib cartilage, which can also make breathing uncomfortable.
For over a year my mother had periodically been reporting “labored breathing.”
We thought it was either panic attacks (which she definitely had), anxiety attacks (which she definitely had), and perhaps some of this was side effects from narcotic painkillers (difficulty breathing is a well-established possible side effect of these drugs).
After going on Cymbalta, my mother rarely reported bouts of labored breathing; it was no coincidence (it seemed) that once she was on this antidepressant, the panic and anxiety attacks ceased.
Thus, it was no mystery what had happened to the breathing problems.
Fast forward about 12 months. My mother has been free of anxiety and panic issues for all this time, but one morning, out of the blue, is weeping because she’s having trouble breathing.
Because I had seen this behavior so many times before while my mother struggled with clinical depression (secondary to eventually-diagnosed low thyroid) and severe anxiety, I thought it was just a renegade anxiety attack that slipped through the cracks.
(I had been staying with my parents for about a week at this point, to help my father recover from back surgery).
However, my tune changed when my mother began vomiting about 20 minutes later.
She had had nothing unusual to eat the day prior. Vomiting was not normal for my mother.
Nevertheless, I still attributed this to a sudden panic attack – panic attacks can cause vomiting.
I knew that she had recently weaned completely off the antidepressant/anti-anxiety drug Effexor, and this reinforced my assessment that she was simply having an anxiety attack.
But then I began thinking: My mother had had multitudes of panic episodes, and not once had ever vomited.
I also knew that an impending heart attack can cause someone to vomit.
I took her to the emergency room where three troponin tests, plus a CAT scan of her heart, were normal. So was her pulse and blood pressure, plus a stethoscope exam.
An EKG was indeterminate. She was sent home with a diagnosis of gastroesophageal reflux disease.
The next morning my mother felt perfectly fine. The next morning I was awakened at 7 am by the sound of my mother’s stressed breathing, and she said since 5 am her chest had been hurting.
I knew something was wrong and told her she was going back to the emergency room. But 30 minutes later, when she felt perfectly fine, she refused to go.
“Finding out what’s really wrong can be frightening, but never knowing can kill you.”
“I feel fine,” she insisted. And she looked fine, too.
But I said, “We have to find out what’s wrong. This isn’t indigestion. Finding out what’s really wrong can be frightening, but never knowing can kill you.”
We went to the emergency room and the new troponin tests were slightly elevated, and because of this, the doctor recommended she be admitted overnight. The next day she had an echocardiogram: abnormal.
Following this was a catheter angiogram: Her coronary arteries were almost completely blocked, and two hours later, she was undergoing quintuple bypass surgery – the cardiothoracic surgeon had informed me that a heart attack could occur at any moment.
I can conclude, then, based on retrospect and logic, that an impending heart attack resulted in the difficulty breathing a few days prior, plus the chest pain, and the vomiting.
Trust your gut instinct, especially if something is different about the picture, a symptom that was never there before.
And remember the following if you’re in the ER:
An EKG, stethoscope, blood pressure reading, a doctor feeling your chest and abdomen, feeling your pulse, and troponin tests cannot rule out severely blocked coronary arteries!
A recent heart attack can be ruled out — but these tests absolutely cannot rule out an imminent heart attack!
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: Freepik.com, jcomp
Heart Palpitations During Weightlifting: Causes, Solutions

Have you noticed a fluttering heartbeat or heart palpitations during your weight workouts or shortly after?
Should you be unnerved about this experience?
“Weightlifting due to the muscular exertion delivers an increased return of blood to the heart due to the pumping effect of skeletal muscle,” says Dr. Ronald Scheib, MD, cardiologist, past Medical Director at Pritikin Longevity Center & Spa in Miami.
“By abruptly increasing the volume of blood returning to the heart chambers, it will increase the pressure and produce dilatation [dilation] of the chambers that are involved in controlling heart rhythm,” continues Dr. Scheib.
“As a consequence, abrupt lifting weight can produce transient arrhythmias.”
Don’t let the medical lingo frighten you; this occurrence is benign.
If you’re having heart palpitations seemingly related to lifting weights, there’s yet another possible cause.
And that’s anxiety, which can be about anything in a person’s life — including your weightlifting regimen itself.
For example, you may be worried that your imminent set will trigger an old injury or make an existing injury worse.
You may have anxiety going on about failing to perform as well as you did the preceding week.
In between weightlifting sets you may find yourself worrying about something in your personal life, such as a relationship or job situation, and as a result, you have palpitations.
The weightlifting didn’t cause the palpitations in these examples, but the lifting of weights just happens to be the activity you were doing shortly before you felt the irregular heartbeats.
The mix of increased blood volume and mental stress can bring on heart palpitations for sure.
However — these benign scenarios don’t mean that you can’t have an actual pathology that needs treatment.
You need to pay attention to when your heart has palpitations and see if there’s an associated pattern, particularly one involving feelings of anxiety or stressing out about something.
You should see a cardiologist and ask about tests to make sure all is fine with your heart.
 Dr. Scheib passed away in 2018. To the Pritikin Center he brought a career in cardiology spanning four decades, including Miami Heart Institute Chief of the Section of Cardiovascular Medicine, and President of the Medical Staff.
Dr. Scheib passed away in 2018. To the Pritikin Center he brought a career in cardiology spanning four decades, including Miami Heart Institute Chief of the Section of Cardiovascular Medicine, and President of the Medical Staff.
 Lorra Garrick has been covering medical, health and security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE certified personal trainer.
Lorra Garrick has been covering medical, health and security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE certified personal trainer.
Top image: Shutterstock/eggeegg
Can Impending Heart Attack Be Misdiagnosed As GERD (Heartburn)?
GERD specialist Dr. Carson Liu says that imminent heart attack symptoms can mimic heartburn.
Have you been sent home from the ER with a GERD (gastroesophageal reflux disease) diagnosis as a result of chest pain or difficulty breathing, even though this could actually mean an impending heart attack?
“Chest pain and pressure is an emergency symptom,” says Dr. Carson Liu, MD, who specializes in treating upper gastrointestinal medical conditions, including GERD.
“It’s the one thing people should relay to the triage nurse in the ER department to get moved to the front of the waiting room in a busy ER.”
Don’t pass this off as, “Oh, it’s only indigestion.” This can be a fatal mistake. My mother complained of difficulty breathing one morning, and shortly after vomited.
My father asked her what she ate the day before. I bypassed that thinking and wondered about the vomiting.
Looming Heart Attack: the Great GERD Mimicker
Vomiting and shortness of breath are classic symptoms of an imminent heart attack. They can also be caused by GERD: gastroesophageal reflux disease.
Dr. Liu explains, “I definitely think heartburn can mimic cardiac disease as well as the reverse.
“The message would be not to ignore symptoms of chest pressure, burning, indigestion, because either GERD or heart disease is a serious matter.
“Heart disease can take one’s life immediately, while GERD can take one’s quality of life away, not to mention increase the risk of esophageal cancer.”
I took my mother to the ER where she had a chest X-ray (normal), EKG (atypical) and blood test (normal) — none of which can detect severely blocked coronary arteries.
The ER physician asked about her symptoms (chest pain and chest pressure that she’d been having on and off for several weeks, and difficulty breathing), and concluded that she most likely had GERD and discharged her.
Two days later, following a second trip to the ER, an abnormal blood test, and hospital admission, my mother was on the operating table for quintuple bypass surgery and mitral valve replacement.
What went wrong in the ER that first visit?
Dr. Liu explains, “GERD is usually the diagnosis only after excluding cardiac ischemia or aortic dissection.”
In the ER, people with chest pain are given a blood test at least twice to measure an enzyme called troponin, which damaged cardiac tissue leaks into the bloodstream.
If the level is within a normal range, it’s determined that you did not have a heart attack.
However, this test cannot determine that you’re about to have a heart attack — only if you already had one or are in the process of having one.
(A few hours before my mother’s surgery, the surgeon informed me that a massive heart attack was imminent).
For the first ER visit, significant coronary blockage was not ruled out. Only after she was admitted to the hospital after the second ER visit, was this diagnosed via catheter angiogram.
My mother wasn’t even given a CT angiogram in that first visit, despite her elderly status and report of chest pains over the past several weeks.
The CT angiogram has been shown to be a highly effective tool at detecting patients at high risk for imminent heart attacks (Hollander et al, University of Pennsylvania School of Medicine).
Thoracic aortic dissection (tear in inner aortic artery wall), which causes wrenching chest pain, is quickly ruled out with an ultrasound.
“Cardiovascular problems are fixable if caught early, but devastating if missed,” says Dr Liu.
“The ER department will usually order a 12-lead EKG which will show if there are any ischemic changes occurring at the time of the chest pain symptoms.
“If the patient doesn’t have pain when the EKG is performed, then the EKG might be normal.
“So the EKG should be done while the patient still has symptoms of chest pain or pressure.”
My mother’s EKG showed a “left bundle block,” which the doctor said interfered with an accurate interpretation.
“Anyone with a history of hypertension, hypercholesterolemia needs to have cardiac ischemia ruled out first, as this is the most common and dangerous thing,” says Dr. Liu.
My mother always had normal blood pressure, but her records did show very high triglycerides.
She was given a GERD information sheet and a prescription to a GERD drug.
The information sheet, however, urged patients to go to the ER if they had ongoing chest pain and other heart attack symptoms.
“Usually the ER doc will give a cocktail of lidocaine, Mylanta by mouth, and if this resolves the heartburn issues, it is probably GERD,” says Dr. Liu.
My mother was in the ER that first visit for many hours and was never given any GERD medications.
Warning
If the troponin test, chest X-ray, EKG, blood pressure and heartbeat are normal and you’ve been diagnosed with GERD based on a questionnaire … insist upon further tests to absolutely rule out significantly blocked arteries, even if it means having to be admitted.
Being awakened at 5 a.m. with chest pain that lasts two hours, which happened to my mother, is likely not a symptom of GERD.

Dr. Liu has conducted extensive research and is widely published in the fields of bariatric and gastrointestinal surgery.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: Shutterstock/fizkes
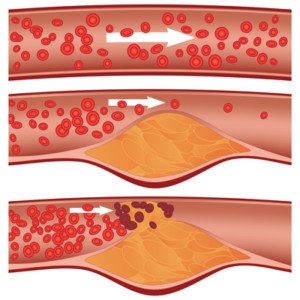
Chest Pain: Can Imminent Heart Attack Be Misdiagnosed in ER?
Imminent heart attack can be missed by ER doctors when it comes to your chest pain.
The ER doctor may misdiagnose your chest pain as GERD or acid reflux.
My mother went into the ER with chest pain and shortness of breath, and the ER doctor thought it was GERD after the second troponin test (like the first) came back normal.
A heart attack releases troponins – a protein that leaks from injured cardiac tissue – into the bloodstream.
He actually told my mother, “I don’t think you have a heart problem. This has a GI flavor to it.” Yes, exact words.
The ER doctor prescribed Prilosec, a heartburn drug. Less than 48 hours later, my mother was undergoing quintuple bypass surgery.
What on earth happened?
“The patient is probably having pain from ischemia (angina), but since there has been no tissue death, troponin won’t appear,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
“In theory anginal pain can come and go almost indefinitely, so these folks can have hours of pain with negative tests,” continues Hanifin.
“It’s just a matter of timing when the tissue finally starts to infarct [dies from obstructed blood supply]. Unfortunately for some folks, this is not until after discharge.”
# 1 depicts a blood clot. JHeuser [CC BY-SA 3.0]
Misdiagnosis of a Pending Heart Attack for GERD
My sister is a medical doctor. She flipped when I told her the ER doctor diagnosed our mother’s chest pain and shortness of breath as acid reflux.
My sister fumed, “Chest pain is so often misdiagnosed as GERD and patients are sent home and then have a heart attack!”
My mother didn’t have the heart attack. Two days later she was back in the ER with chest pain, and this time, a different ER doctor recommended she be admitted because her troponin level was elevated – not enough to diagnose heart attack, but enough to concern the ER doctor.
“When looking at a test like cardiac enzymes, it is important to consider that it is not really testing whether a patient is HAVING a heart attack,” says Hanifin.
“It is testing whether a patient HAD a heart attack over the previous several hours to days.”
The test does not tell if your arteries are clogged.
There was no further chest pain during her evening and overnight hospital stay, and even next day, no chest pain.
An echocardiogram was performed first (the next day) to see if it was safe to have a stress test.
The echocardiogram came back “abnormal,” and the cardiologist recommended the invasive catheter angiogram.

Catheter angiogram is the gold standard for detecting blocked arteries, but it comes with the risk of stroke and heart attack — though this risk is very small. Shutterstock/MAD.vertise
“It’s unsafe to send you home,” the internal medicine doctor told her after she insisted she wanted to just go home.
All along, I had felt funny about that first ER diagnosis of GERD.
That first visit hadn’t been just for chest pain and shortness of breath.
My mother had also vomited that morning. The triad of chest pain, shortness of breath and vomiting can mean an imminent heart attack!
However, the first ER doctor was all too sure that the chest pain, shortness of breath and vomiting meant GERD.
What should’ve the first ER doctor told my mother?
He should have explained: “The negative troponin means you did not have a heart attack. We did not give you a diagnostic test for GERD — and this may very well be GERD, but … we also did not give you any tests to rule out severe heart disease, either.
“Though your symptoms sound like GERD, they also sound like extensive coronary artery blockage. I can’t send you home with a diagnosis of GERD.
“I am going to send you home with a diagnosis that you did not have a heart attack. But I can’t rule out that you won’t have a heart attack in the next 24 hours.”
The catheter angiogram revealed extensive coronary artery blockage, and the bypass surgery was begun only a few hours later.
Prior to surgery, I had asked the cardiothoracic surgeon, cardiologist and internal medicine doctor these exact words: “You mean, if my mother goes home without this surgery, she might have a fatal heart attack within a week?”
All three simultaneously said yes. That is the truth.
“Making medical decisions involves looking at probabilities,” says Hanifin. “A chest pain patient who has multiple negative cardiac enzymes, ECGs and a negative stress test has a very small likelihood that their pain is due to ischemia, but the likelihood is never 100% eliminated.”
Another issue is that emergency rooms do not provide stress tests.
The patient would either have to be admitted to get a stress test the next day, or, if the patient is sent home from the ER, it could be many days before they could get a stress test scheduled through their doctor. By then it could be too late.
“The decision to further evaluate a patient is therefore based on a person’s risk factors,” says Hanifin.
“Factors like diabetes, high blood pressure, smoking, a sedentary lifestyle and a family history of cardiac disease are all very troubling in a chest pain patient, even when their tests look good.”
 Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.