Can Running Cause Hip Bursitis (Trochanteric)?

Dr. Bright explains, “Trochanteric bursitis is very common among runners. In order to understand trochanteric bursitis, it is important to have an understanding of what a bursa is.”
If you suffer bursitis hip pain from running, here are some excellent exercise treatments that are recommended by a sports medicine doctor.
“Trochanteric bursitis is very common among runners,” says Darrin Bright, MD, who specializes in sports medicine and family medicine with OhioHealth Physician Group.
“In order to understand trochanteric bursitis, it is important to have an understanding of what a bursa is.
“A bursa represents a fluid filled sack that allows structures to glide smoothly over other structures. Bursitis occurs when the bursa becomes inflamed from repetitive movement or excessive pressure.”
Right off the bat, you see how running or jogging can easily be a cause of hip bursitis, what with all of the repetitive movement going on in the hip joint.
Dr. Bright continues, “In this case, the greater trochanteric bursa lies on top of the hip bone, allowing the iliotibial band to glide smoothly over the hip bone.
“Running results in repetitive movement of the IT band over the bursa, which may result in greater trochanteric bursitis.
“Similarly, if the IT band is tight it will exert excessive pressure on the bursa, resulting in greater trochanteric bursitis.”
What kind of exercises are therapeutic for bursitis of the hip caused by running?
Dr. Bright says, “Physical therapy (PT) is an integral part of the recovering from greater trochanteric bursitis.
“PT is directed at stretching the iliotibial band as well as strengthening the gluteus medius and other hip external rotators.”
Here are a few exercises for strengthening the gluteus medius and gluteus minimus, which are responsible for external hip rotation (the major “butt muscle,” the gluteus maximus, enables hip extension).
#1. The hip abduction machine at your gym. This isolates the hip rotator muscles.
#2. Get on all fours. Keeping one knee on the floor, lift the other leg (think of how a male dog lifts one leg to relieve itself) so that the inner thigh is parallel with floor, but lower leg bent so that there is a 90 degree angle at the knee. Thighs are perpendicular to each other. Then lower.
Do repetitions this way. You should feel the outside of your hip and upper thigh working. This exercise will fatigue the hip rotators quickly. Switch sides.
#3. Inline skating, especially up hills, will target the hip rotators. (If this aggravates hip bursitis pain, then don’t do it.)
#4. Stand with feet shoulder width apart. Lift one leg into a high-march position, but don’t extend lower leg.
Now rotate upper leg to the side so that the knee is to your side, maintaining the high-march position, then return to starting high-march position.
Repeat for reps, keeping knee high. This will tire you quickly if you’re not used to doing isolation work for hip rotators. Switch legs.
If someone has hip trochanteric bursitis, how long should they avoid running?
Dr. Bright explains, “Recommendations regarding running with greater trochanteric bursitis will vary depending on the degree of injury.
“I usually recommend using pain as your guide. If the pain is affecting your gait or you are limping, then you should not run.
“Otherwise if you aren’t limping try some easy running and see how it goes. Avoid hills and up-tempo or faster running.
“Icing after activity and again at bedtime can help with the inflammation in the bursa.”
Don’t let your hip bursitis make you lose hope with your running program.
 Dr. Bright gives special focus to comprehensive care for runners, triathletes and cyclists, overuse injuries, stress fractures and active release technique (ART).
Dr. Bright gives special focus to comprehensive care for runners, triathletes and cyclists, overuse injuries, stress fractures and active release technique (ART).
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
Lamictal Rash Side Effect: Causes and Prevention

The Lamictal rash, a side effect of this drug, is well-known in the community of Lamictal users.
And this rash isn’t pretty at all.
Is there a way to prevent this side effect?
And what causes the Lamictal rash in the first place?
In fact, the Lamictal rash can be much more than nasty; the website for this prescription drug states:
LAMICTAL may cause a serious skin rash that may cause you to be hospitalized or to stop LAMICTAL; it may rarely cause death.
For this article I asked Dr. Oanh Lauring, MD, founder of Lauring Dermatology in Nottingham, MD, how it is that this serious skin rash can develop from taking Lamictal. She explained:
“The mechanism is unknown and approx 20 percent of patients can develop some type of a rash, but it is rarely life threatening. It usually presents as hives, itching or red blotchy patches all over the body.”
In other words, if you develop the Lamictal rash, there is no need to fear for your life. The drug’s Website further explains:
There is no way to tell if a mild rash will develop into a more serious reaction. These serious skin reactions are more likely to happen when you begin taking LAMICTAL, within the first 2-8 weeks of treatment.
But it can happen in people who have taken LAMICTAL for any period of time. Children between 2 to 16 years of age have a higher chance of getting this serious skin reaction while taking LAMICTAL.
Is there a way to prevent the Lamictal rash?
Dr. Lauring says no. She explains, “Other more well-known anti-epileptics such as phenytoin, phenobarbital, primodone are more likely causes of life threatening rashes like Steven-Johnsons syndrome (patients have sloughing and bleeding of their mucosa such as the mouth, gut and groin), or toxic epidermal necrolysis (patients can slough off their entire skin within hours to a few days).
“These rashes represent an autoimmune hypersensitivity response that is purely genetic-based and therefore you cannot prevent it.
“If any family members are allergic to a specific class of medications, then they should use these meds with caution.
“If someone has a clear-cut severe itchy rash to a drug (and I have excluded infection), I may treat them with oral antihistamines and topical or oral steroids depending on the severity.”
According to the Website, your risk of getting a rash from using Lamictal increases, if you are also taking Depakene or Depakote (anti-seizure drugs).
Another factor that increases risk of this situation is if you take a higher starting dose than what your physician has prescribed for you.
Finally, a third variable that raises the risk of this skin rash is if your dose of the drug is increased at a faster rate than what has been prescribed.
 Dr. Lauring is former chief of dermatology at Mercy Medical Center. Lauring Dermatology provides medical and cosmetic services including for skin cancer, acne, psoriasis, hair and nail problems, and skin rejuvenation.
Dr. Lauring is former chief of dermatology at Mercy Medical Center. Lauring Dermatology provides medical and cosmetic services including for skin cancer, acne, psoriasis, hair and nail problems, and skin rejuvenation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Seborrheic Keratosis Turn into Skin Cancer?

Seborrheic keratoses can look like melanoma, the deadly skin cancer.
These benign lesions can come in a variety of colors, sizes and shapes, and can raise concern if you just happen to discover one or a few on your skin.
Seborrheic keratoses can easily be identified by a dermatologist and have several classic features.
One such feature of seborrheic keratoses is that it can resemble skin cancer, including melanoma.
There are two questions to consider.
1 Can skin cancer or melanoma arise from the cells of a seborrheic keratosis?
2 Is a seborrheic keratosis more likely to develop into melanoma when compared to regular areas of skin?
“Seborrheic keratoses represent a normal thickening of the skin,” says Adam J. Mamelak, MD, a board certified dermatologist and founder of Sanova Dermatology in Austin, TX.
They can appear to be stuck onto the skin in the way that a little speck of dirt or clay can be stuck on. But not all appear that way.
They may resemble warts, but a seborrheic keratosis does not contain the virus that causes warts, the human papilloma virus.
A seborrheic keratosis that develops or progresses can begin to look like a wart, with a lot of unsightly texture.
On the other hand, some can appear like glossy tiny droplets, which can be flesh colored, pinkish or some shade of brown, with a smooth surface.
Seborrheic keratosis
These lesions may, or may not, itch. You may never know you have them unless you just happen to visually discover them upon, for example, adjusting your bra strap in the mirror, and you see a few speckles on your skin that you didn’t notice before.
They can appear just about anywhere and usually begin appearing after age 40.
“Their development is most often genetic,” says Dr. Mamelak. “If your parents have them, there’s a good chance you’ll get them as well.
“Often called age or liver spots, seborrheic keratoses are completely benign.” In short, their cells are not atypical.
But we need to dig deeper here. The cells that make up a seborrheic keratosis are perfectly normal — but can they ever become cancerous?
Dr. Mamelak explains, “The skin cells that make up a seborrheic keratosis can become malignant, just as they can in normal skin.
“That is, a skin cancer can arise within a seborrheic keratosis the same way it can arise in normal-appearing skin.”
This shouldn’t be surprising, because these benign skin barnacles are MADE UP OF SKIN.
As for their likelihood of turning cancerous when compared to surrounding skin, Dr. Mamelak says, “The risks for a skin cancer arising anywhere are the same: history of excessive sun exposure and sunburns, fair skin and complexion, personal and/or family history of a skin cancer.”
If one of these skin growths is scratched, it can bleed. Do not take this to mean a sign of melanoma or other cancer.
“And while some consider them unsightly, or they can catch or rub on clothing and become painful and irritated, there is no reason to treat them unless they become symptomatic,” says Dr. Mamelak.
“Just as you should be mindful of a non-healing or changing lesion on your skin, if a seborrheic keratosis starts to change in appearance, bleeds or changes color, it should be evaluated.”
Otherwise … you may as well just leave them be, unless the itching gets annoying; they interfere with clothes; or they become a cosmetic issue. They can be removed via liquid nitrogen by freezing.
A scar may result from the new skin, growing in after the removal, having different pigment concentrations than the original skin.
If you are not sure you have a seborrheic keratosis, and keep wondering if it might be melanoma or some other kind of skin cancer, make an appointment with a dermatologist. The peace of mind will be worth it.
 Dr. Mamelakfocuses on the full breadth of dermatologic care, from cosmetic skin solutions to advanced skin cancer removal. He’s founder of the Austin Mohs Surgery Center, which is dedicated to the treatment and management of skin cancer.
Dr. Mamelakfocuses on the full breadth of dermatologic care, from cosmetic skin solutions to advanced skin cancer removal. He’s founder of the Austin Mohs Surgery Center, which is dedicated to the treatment and management of skin cancer.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: James Heilman, MD, CreativeCommons
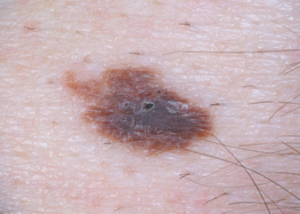
When an Itching Mole Begins Bothering You

Here’s what a dermatologist says about itching moles.
If you’re concerned about an itching mole (could it be melanoma?), first make sure that the itching is coming from the actual spot itself, rather than nearby skin.
Sometimes it’s difficult to tell precisely where the itching is coming from.
With that said, assume that you have an itching mole. According to dermatologist Alan Rockoff, MD, a suddenly-itching mole probably means trauma to the little spot – rather than cancer or melanoma.
A woman complaining of an itching mole wrote in to medhelp.org.
She says there is a tiny darker spot on an otherwise symmetrical, brown mole, and the mole had been there “forever.”
However, it is located beneath where her bra strap normally lies.
A few days before she wrote in, the spot began feeling weird.
When she touched it, it became sensitive, as though being poked with a little needle.
She wanted to know if it was possible to have an itching mole that was not melanoma or another form of cancer.
Dr. Rockoff, with the Rockoff Dermatology Center in Brookline, MA, explains, ”When a mole starts to bother you suddenly, that invariably means not cancer, but minor trauma.
“I’m sure that when you see the doctor, the dark spot — if it’s even still there — will be diagnosed as a small scab from the mole’s rubbing on your bra.
“The needle sensation is also almost certain to be from the rubbing.
“Just keep the mole covered so it doesn’t run, and don’t freak out — just see the doctor for reassurance and you’ll be fine!”
The patient described her problem in fine detail. But had she simply said, “I have an itching mole,” and said nothing more, this likely would have altered Dr. Rockoff’s response – because melanoma can indeed cause a mole to itch.
The patient is being smart by planning on seeing a doctor. And that’s exactly what you should do if a spot on your skin becomes worrisome.
Some people are mole hypochondriacs and create needless anxiety.
On the other hand, around 8,000 U.S. people die every year from melanoma.
Many would still be alive if they, too, were hypochondriacs – or, to put it another way, hyper-vigilant about skin surveillance for suspicious changes.
Melanoma is a ruthless cancer once it spreads. However, it is one of the most curable forms of cancer when caught early.
With vigilant surveillance, the layperson can catch melanoma early.

Melanoma. Shutterstock/Krzysztof Winnik

Melanoma. CreativeCommons/Hans677

Melanoma. Cancer.gov
To help catch melanoma early, it’s important to conduct monthly skin checks.
If you have moles in difficult to inspect areas such as your back, you can have a dermatologist inspect them every six months; this will provide you peace of mind and extra surveillance.
Just because your insurance won’t cover elective screening like this doesn’t mean you shouldn’t invest in it.
If you keep scratching a mole, it is likely to continue itching, just like any other area of the skin that you keep scratching, since repeated scratching produces histamines that cause even more itching.
 Dr. Rockoff is a clinical assistant professor of dermatology at Tufts University School of Medicine and has taught senior medical students for 30+ years. His publications have appeared in numerous journals.
Dr. Rockoff is a clinical assistant professor of dermatology at Tufts University School of Medicine and has taught senior medical students for 30+ years. His publications have appeared in numerous journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ivan_kislitsin
Can a Changing Mole Be Benign or Is It Always Melanoma?

We’ve been scared by the media about changes in moles, and skin cancer, a la, “If you notice any changes in a mole, see a doctor immediately, as this could mean skin cancer.”
And you should, because ruling out skin cancer is very easy for doctors to do. Usually, a changing mole, or one that appears to have changed, is not skin cancer.
I’m telling you this so that if you notice a changing mole, you don’t panic and think you’ll die.
But again, I stress, if a mole has changed, see a doctor as soon as possible, just to play safe.
The procedure to determine skin cancer is so easy to perform, that there really is no excuse for skipping the doctor appointment. Changes in a mole have a variety of causes.
“Irritated moles commonly change,” says Jason R. Lupton, MD, board certified dermatologist practicing in the San Diego, CA area.
“They may get irritated from clothing, rubbing on waistbands for example, rubbing on surfboards! (common here in San Diego), rubbing on jewelry — these may get irritated and itchy and become red or crusted as a result.”
(A red or “crusting” mole can also be a sign of skin cancer.)
Dr. Lupton continues: “Also, moles in areas like the axilla (underarms) may become irritated form rubbing/friction.
“Moles may become ‘halo nevi’ — these are moles that develop a ring of light color around them. Although most are benign, these should always be evaluated to ensure they are not melanomas.”

Halo nevus (mole)
If you are pregnant, moles may “may become darker or larger as a result of hormonal changes, or from stretching of the skin — due to growth or an enlarging abdomen,” says Dr. Lupton.
“Typically good signs are if multiple moles are getting darker/bigger simultaneously rather than just one particular mole.”
Do you have acne? Dr. Lupton explains, “Patients with acne may have moles that ‘appear’ to change — either from an underlying cyst or pimple that imparts a swelling or redness to the mole temporarily.
“This can be differentiated from a changing mole due to the relatively short time period of change.”
Moles have a life span, and over a long period (years), they may “simply change and evolve over time — become smaller, lighter and some actually seem to disappear.”
Finally, Dr. Lupton says, “Contact causes for ‘mole changes’ are also quite plausible, as certain chemical or caustic contacts may impart irritation or redness to the area, making a mole look different.”
 Dr. Lupton specializes in skin cancer prevention and treatment plus minimally invasive cosmetic procedures including mole removal, skin rejuvenation, wrinkle reduction and acne treatment.
Dr. Lupton specializes in skin cancer prevention and treatment plus minimally invasive cosmetic procedures including mole removal, skin rejuvenation, wrinkle reduction and acne treatment.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/wavebreakmedia
Do the Big Moles on Your Child’s Back Have You Worried?

Lots of big moles on your child’s back can be intimidating to look at.
With all the heightened awareness over the past decade of moles, melanoma and skin cancer, it’s only natural that you’d be unsettled at all the large moles on your child’s back.
Your worry, unfortunately, is not unfounded.
Your fear that one of those weird looking moles on your child’s back might turn into cancer (melanoma) is, unfortunately, legitimate, especially if there is a large number of them.
Leading dermatologist Dr. Joshua Fox discusses moles in children, including big ones on their backs.
Are you worried about all those big moles on your child’s back? Most people are born without “birth marks.”
Research shows that every beach vacation gives rise to a 5 percent increase in the appearance of small moles on a child.
Dr. Fox says, “The development of new moles is of concern, because the higher the number, and the more irregular moles, the greater the risk for developing melanoma, the most dangerous of the skin cancers.”
What about big moles on my child’s back?
Dr. Fox is founder and director of New York and New Jersey-based Advanced Dermatology P.C.
I asked him (for purposes of this article) specifically about large moles all over a child’s back: Does this reflect excessive sun exposure?
My teen nephew has many big, funny-looking moles all over his back, and he is almost always shirtless on summer lake vacations and tropical vacations.
Dermatologists call moles “nevi” (rhymes with Levi, as in Levi jeans), and the singular form of nevi is “nevus.”
Odd looking or atypical nevi are called dysplastic nevi, and they can resemble melanoma. Having dysplastic nevi is a risk factor for melanoma.
Dr. Fox says that most nevi are not worrisome, but as a parent you should monitor your child’s skin for any changes in nevi or new nevi. This will be challenging if your child has a lot of spots, like my nephew.
If your child has a lot of moles on his back or elsewhere, it would be very smart to pursue serial digital dermoscopy as a way of tracking all the nevi.
Relationship between moles on child’s back and sun exposure?

Shutterstock/ Guenter Albers
“Many dysplastic nevi seem to occur in areas in which the child received severe sunburn on one or more occasions,” says Dr. Fox. “It often matches the clothing distribution.
“In addition, there is a genetic relationship to melanoma. Only about 1 percent of infants are born with a mole.
” For those children who have many nevi, we encourage parents to check their child’s moles monthly to detect changes.”
If you notice a new “birth mark” on your child, keep visual track of it. “Normal looking new moles are not suspicious,” says Dr. Fox. About one-third of melanomas arise in a pre-existing nevus.
“By the time most people reach adulthood, they have between 10 and 40 moles,” says Dr. Fox.
A lot of sun is another risk factor for melanoma, and maybe as a parent you’re not overly concerned about your child developing melanoma since this is extremely rare in kids.
However, older age is a risk factor for melanoma, and childhood sun exposure can lay the groundwork for melanoma risk decades later!
In other words, parents should see the big picture: Their child’s risk of melanoma when their “kid” is 40 years old!
If you’re inspecting your child’s back moles (or elsewhere) for the first time and notice that some look funny, this doesn’t mean melanoma.
Get familiar with the nevi so that you can detect a changing or evolving nevus.
Follow your gut feeling and make an appointment with a dermatologist if your child has a suspicious looking skin lesion.
Concerning signs include irregular shape, jagged edges, red portions within the nevus or varying colors, larger than a pencil eraser, and of course . . . changing.
How often should I check the moles on my child’s back?
Every month, and inspect any area exposed to sun including the scalp and behind ears.
Draw a mole map and take photos and compare every month.
If this is overwhelming, pursue serial digital dermoscopy, which is ideal for kids and adults who have many moles on their back.

In 1987 Dr. Fox founded the AAD Melanoma and Skin Cancer Prevention Program in Queens, NY. He has been chief of dermatology of several major teaching hospitals including Mt. Sinai Hospital of Queens.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Albina Glisic
Are Most Funny Looking Moles Normal & Benign?
A dermatologist speaks about strange or weird looking moles.
Have you discovered a funny looking mole on your body and wonder if it’s melanoma?
The aggravating thing about finding a strange looking spot is when you’ve never done a skin exam for cancer before, and thus, you have no idea if the “birth mark” has always looked funny.
So now, you study the strange mole every day, wondering if it’s in the process of changing.
“Generally speaking, when moles have the following qualities, it can raise a concern for melanoma,” says Andrea Cambio, MD, board certified dermatologic surgeon, and medical director of Cambio Dermatology in Florida.
Asymmetry. One half of the lesion does not match the other in terms of color, size or shape.
Border irregularity. The border is jagged, scalloped, notched or not smooth, or “bleeds” into the surrounding skin.

Dysplastic mole. Cancer.gov
Color variation. It has different shades of blue, black, brown or red.
Diameter. Greater than that of a pencil eraser (6 mm).
Evolving. It is changing; it may be crusting, bleeding, itching, elevating, changing colors or getting darker (or lighter).
What if you’re viewing a funny looking mole for the first time? Has it always been that way? What did it look like a year ago? Was it even there a year ago?
What should you do?
Live in fear for the next few months as you keep an eye on the strange looking mole, wondering if it’s in the process of evolving?
Dr. Cambio explains, “Any mole can have one or more of these qualities and still be benign. A board-certified dermatologist is skilled at evaluating moles.”
If the spot appears suspicious to the physician, “it may need to be removed and sent for biopsy to differentiate a benign mole from a pre-cancerous or cancerous one.”
For peace of mind, it’s perfectly okay to request that the spot be biopsied. This can be a partial biopsy or removal of the entire lesion.
Don’t worry about scarring; it’s negligible and may be less noticeable than the pigmented growth that was removed.
A dermatologist may feel very certain that a strange mole is benign, but remember, absolute proof of this can only come from a biopsy.
Dr. Cambio adds, “The more atypical (dysplastic) moles an individual has, the more likely they are to develop a melanoma in their lifetime.”
These are funny or “ugly” moles that typically appear on a person’s back.

Dr. Cambio has extensive training and experience in all aspects of adult and pediatric dermatology, laser, skin cancer, dermatologic surgery and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Mikel Ugarte Gil
Trouble Breathing After Coronary Bypass Causes & Solutions

Trouble breathing or shortness of breath after coronary bypass surgery?
There are actually several causes for breathing difficulties following coronary bypass surgery (aka CABG).
“Shortness of breath is very common after coronary artery bypass grafting,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Primary causes include atelectasis (collapse of small air sacks in the lungs), and fluid within or around the lung.”
My mother, following her quintuple bypass surgery, had this exact problem.
The term “pulmonary effusion” came up when she was examined, and the fluid and partial collapse was detected with imaging tests.
She had bouts of “labored breathing” or “difficulty breathing,” that in part, could be explained by the atelectasis and effusion.
Dr. Fiocco continues, “Every patient has these issues after surgery to some degree. Atelectasis occurs due to poor inspiratory effort due to the pain of the incision.
“This improves with walking, deep breathing exercises and coughing.”
My mother was instructed to use a little gadget called an incentive spirometer.

BruceBlaus/CC
It’s not only given to coronary bypass patients, but anybody who needs bed rest following any kind of surgery … to encourage lung expansion, which will help prevent breathing difficulties and pneumonia.
The patient places the mouth on the spirometer’s mouthpiece and slowly inhales, while watching the device record a numerical value of how much air is being inhaled.
Coughing gets the lungs working; very important for coronary bypass patients to help with their breathing and prevent any problems.
A respiratory therapist will also visit the CABG patient, but despite these measures, the coronary bypass patient may still (and commonly) experience some trouble with breathing.
So what can be done, then, about the fluid buildup in the lungs after coronary bypass surgery?
Dr. Fiocco explains, “Fluid is removed with diuretics (fluid pill). They increase your urine output and draws fluid off the lungs.”
But what if the patient, following coronary bypass surgery, has renal failure?
My mother had “mild” renal failure, and hence, there was a period where she could not receive diuretics, because their effect (promoting urinary output) would stress the kidneys!
Solution? She was on fluid restriction until her creatinine level (measure of kidney function) was acceptable.
Over time the fluid buildup in her lungs disappeared, and her lungs eventually appeared normal on imaging.
A coronary bypass patient, however, can end up with so much fluid that it really makes breathing difficult, and frequently.
Dr. Fiocco says, “Occasionally, so much fluid accumulates around the lung that it must be drained with a catheter.”
My mother’s surgeon actually mentioned this as a plan if a follow-up CAT scan were to show that the fluid was still present.
“Rarely, fluid collections around the heart can cause shortness of breath requiring drainage,” adds Dr. Fiocco.
“Even more rare is a pulmonary embolus, or blood clot to the lung which is treated with blood thinners.”
Finally, a possible cause of trouble breathing after coronary bypass surgery, especially when the previous mentioned issues have been ruled out, is plain anxiety.
My mother’s cardiologist reported to me that there were a few instances in which she complained of labored breathing, and visibly had trouble with normal breathing,
But once the doctor had her engaged in conversation unrelated to her CABG, her breathing appeared perfectly normal. He told me this was anxiety related.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Diarrhea, Changes in Poop Appearance from Microscopic Colitis
“Change in bowel habits” is commonly listed as a symptom of colon cancer, but this doesn’t mean that microscopic colitis can’t also cause a change in poop habits and appearance.
Your stools and bowel habits can indeed change from microscopic colitis.
So if you’ve been noticing a change in bowel habits lately, sudden diarrhea or a change in the so-called stool caliber — don’t automatically fear this might be colon cancer.
It may very well be microscopic colitis.
“Typically patients experience watery, chronic diarrhea that can last for months or years.” Alan Gingold, DO, a board certified gastroenterologist with Central Jersey Ambulatory Surgical Center.
“It does tend to be intermittent, and the diarrhea can come and go.
“Why patients get diarrhea in this condition is not fully known, but likely the chronic lymphocytes or collagen deposition causes inflammation and scarring, which prevents adequate absorption of water from the colon — leading to diarrhea.”
I developed symptoms of microscopic colitis some years ago.
It first began with sudden-onset diarrhea. I didn’t think anything of it and didn’t even really look at it, because this began happening in the days leading up to my period, and I’ve had premenstrual diarrhea in the past.
However, I noticed that every time I had a bowel movement, it was in the form of diarrhea, and several times a day.
After my period started, I knew something else was going on, and being the health-conscious person I am, I became alarmed.
The diarrhea was liquidy and presented with a light brown color, sometimes with a greenish tinge.
Normally, my diarrhea is a milk chocolate color and colors the toilet water brown; it’s messy.
But this particular diarrhea was swift and “clean,” creating a pile of very loose, scruffy, flaky stools at the bottom of the bowl, sometimes a few pieces floating in the toilet water.
This diarrhea did not look like diarrhea I’ve had in the past.
It would be another 24 days before I was diagnosed with microscopic colitis. In the meantime, the diarrhea seemed to mostly be a reaction to eating.
Soon after eating, I’d feel a churning in my gut: the formation of yet more diarrhea.

Shutterstock/George Rudy
At one point, within 20 minutes after eating a generous amount of brownie and milk, I let loose a lot of diarrhea, and it seemed as though the entire snack went right out the other end.
The diarrhea always contained particles of undigested food.
Spinach (a lot, actually); grapes; sunflower seeds; and different-colored particles such as bits of broccoli and tomatoes.
The diarrhea was more prevalent on days that I consumed a lot of juice and fruit.
I backed off on these, but the diarrhea persisted, though not as much.
Taking an anti-diarrheal drug resulted in two days of nothing, and then I had formed stools, but they looked funny: light brown, scruffy and containing undigested food.
After this bowel movement, the diarrhea returned, and I’d also have very loose stools. The color was always light brown/tan.
Most of the stool pieces sunk in the toilet water, but sometimes there were floating pieces.
At one point a whole mess came out and every chunk stayed on top of the toilet water.
The diarrhea pieces ranged from liquidy to small pieces to bigger chunks, that — when I poked with a Q-tip swab, dispersed rather than maintained their form.
After cutting out fruit, juice and vegetables entirely, I began having loose stools.
But they continued to contain a lot of undigested food: rice, lentils and bits of tomato.
The stools were formed enough to maintain their form when I lifted them out of the water with a plastic spoon.
But they looked very different: light brown, sometimes with a greenish tinge and sometimes with an orange tinge.
The layered stools were greasy looking and appeared to be composed of several different substances, rather than all one uniform substance.
They ranged from normal size to small pieces, and the normal sized stools were pointy on both ends.
Early on in the microscopic colitis, I’d feel the stools or diarrhea forming in my gut throughout the night, and there were times it felt I had to go right then and there, but I stayed in bed.
Soon after getting up for the day, I’d have to relieve myself. But as days went on, it would be around noon before I had a movement.
The movements dropped to 1-2 stool releases per day, still odd looking. With more time, there appeared to be less undigested food in the stools.
Over the next several weeks the situation spontaneously resolved.
Microscopic colitis can only be diagnosed with a colonoscopy.
The doctor must collect tissue from inside the large colon for analysis — and the colonoscopy allows them to do this.
Microscopic colitis in my case resulted in a change in bowel habits, mild abdominal cramping and thirst in the middle of the night.
Patients may also feel bloating, nausea, have weight loss and transient joint aches.
If you suspect microscopic colitis, then remember that only a colonoscopy can detect this.
 Dr. Gingold attributes his success to the extra time he spends with his patients. His areas of expertise include reflux disease, Barrett’s esophagus, capsule endoscopy, chronic liver disease and inflammatory bowel disease. Dr. Alan Gingold is board certified by the American Board of Internal Medicine in Gastroenterology
Dr. Gingold attributes his success to the extra time he spends with his patients. His areas of expertise include reflux disease, Barrett’s esophagus, capsule endoscopy, chronic liver disease and inflammatory bowel disease. Dr. Alan Gingold is board certified by the American Board of Internal Medicine in Gastroenterology
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, katemangostar
When Stool Color Can Mean Cancer
Ever had yellow, chalky, green or black stools?
What about reddish stools?
Do you ever even look at your BMs?
Certain colors of BMs or stools can be a warning sign of cancer.
“Brown, gray, tan or yellow are all caused by your environment – food you eat, beverages you consume and even the level of stress you are experiencing at that time in your life,” says Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
You should examine what’s in the toilet! It’s unsightly, but you need to know what your bowel movements normally look like in shape as well as color, since certain stool colors are associated with colon cancer.
The color of poop can indicate what’s going on in your body. Poop can come in a variety of colors.
Any Shade of Brown Stools
This is normal.
Green Poop

Normal. Don’t panic. It’s not cancer. Bowel movements actually start out as green.
There are two chief causes of green poop: green foods, and quick transit time of the stools through the large intestine.
Leafy green vegetables, cucumbers, green food coloring and iron supplements can turn poop green.

Freepik.com, 8photo
Quick transit time doesn’t give bile enough time to break down completely, thus retaining stools’ original green color.
Yellow Poop
It’s not cancer. It’s fat in your bowel movement. Fatty stools also float.
Light Colored or White Stools
This indicates lack of bile in the bowel movements, possibly caused by a bile duct obstruction.
Drugs for diarrhea can also cause a light color. But see a doctor, because a bile duct can be blocked by liver cancer.
Black or Tarry Stools
SEE DOCTOR. This can have serious as well as harmless causes.

Black or tarry stools
“If blood enters the gastrointestinal tract higher up in the stomach, small intestine or even higher up in the colon, the blood itself is digested before it exits the anus, and digested blood turns this tar or black color,” says Dr. Binderow.
“Black indicates blood being absorbed higher up in the gastrointestinal tract.”
Black bowel movements can mean a bleeding ulcer, gastritis or esophageal tear from vomiting.
On the other hand, iron supplements can blacken bowel movements.
So can anti-diarrheal drugs, black licorice and blueberries.
Red or Maroon Stools

SEE DOCTOR. This could mean several life-threatening medical conditions including colon cancer.
“Maroon is lower in the intestine, and red is even lower, but all need to be checked by a doctor,” says Dr. Binderow.
“There should be no blood in your stool. It could be hemorrhoids, but it could be more serious, so this should always be addressed with your doctor.”
Red in poop can also point to anal fissures, bleeding of the diverticuli, inflammatory bowel disease, and of course, colon cancer.
- If you see blood in your bowel movements, see a doctor promptly.
- Bleeding means something is WRONG.
However…your bowel movements may appear “red” and not have any blood in them.
Bright reddish stools can result from eating foods with red dyes like beverages, gelatin and popsicles.
Bright red poop can also be caused by red licorice, tomato juice, tomato soup and BEETS !

Shutterstock/Lepas
You wouldn’t think beets, with their dark purple color, could cause bright red stools.
But extracted beet juice is one of the brightest reds you’ll ever see.
Beets give BMs more of a crimson “ribbon” around them that intertwines with them, versus literally changing their color.
“Clay” Color
“If the clay is a red clay, this again could be caused by blood in the stool,” says Dr. Binderow.

Clay grey stools
Liver and pancreatic cancer, not just colon, can alter the color of stools, making them a “clay grey.” See a doctor rather than wondering about it!
By being visually acquainted with your BMs, you can learn to distinguish between food-color-induced redness, and blood-induced redness.
Dr. Binderow explains, “Screening with your doctor could be through colonoscopy.
“However, if you are averse to getting a colonoscopy, there is a new noninvasive stool DNA screening test that can be done in one’s home and is available by prescription.”

Cologuard
Cologuard is a non-invasive screening test for colon cancer that uses the latest advances in stool DNA technology.
And that is the detection of altered (mutated) DNA from abnormal cells in a stool sample which could be associated with cancer or precancer.































 Dr. Binderow
Dr. Binderow 







































