Ankle Swelling in the Elderly: Causes & Solutions

Though the site of swollen ankles in elderly people is quite common, this commonality does not rule out a potential life-threatening cause of this symptom.
Ankle swelling in an older person can mean a very serious medical condition.
“If the swelling is new and only in one ankle, especially if the calf or back of the thigh is tender, see your physician to rule out a blood clot,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
Another Serious Cause of Ankle Swelling in the Elderly
If both ankles are swollen, this could mean heart failure.
Dr. Teitelbaum explains, “This is usually associated with shortness of breath, which gets worse after you have been lying down for a while, as well as shortness of breath with exertion.”
An elderly person may assume that shortness of breath is a normal part of aging and not see it as a sign of something more serious.
“Heart failure is a common cause of unnecessary deaths,” continues Dr. Teitelbaum. “Why do I say unnecessary?” he adds.
“Because simple natural therapies are dramatically effective at improving heart failure.
“Your physician, sadly, will likely not have seen this research because these treatments are generally low cost and therefore not profitable for the drug companies to advertise.”

Shutterstock/AppleDK
Dr. Teitelbaum’s Recommendation for a Healthier Heart
“I find that a recipe of ribose (10 g a day), coenzyme Q 10 (200 mg a day), magnesium orotate (3,000 mg a day), acetyl-L-carnitine (1500 mg a day), plus a good B complex vitamin with 200 mg of magnesium (The Energy Revitalization System vitamin powder) will dramatically improve heart failure and other cardiac symptoms within six weeks – and has also been shown to prolong life.”
Innocuous Cause of Ankle Swelling in Elderly Men and Women
“If it is mild swelling that occurs at the end of a long day and was gone by the time you wake up in the morning and occurs in both legs, this is most often simply the effect of gravity,” says Dr. Teitelbaum.
“It helps to prop your feet up on a pillow while you’re resting at the end of the day,” explains Dr. Teitelbaum “so the fluid drains out of your legs before you go to bed.
“Otherwise it will do so while you are sleeping, and you’ll have to wake up to go pee. Varicose veins or venous insufficiency can also cause this.”
Kidney disease, liver cirrhosis and tight socks can also cause ankle swelling (and this is not limited to the elderly).
Additional causes of edema swelling in the ankles of an elderly person: kidney or liver disease, low thyroid, celiac disease and excessive salt/sodium intake.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Toa55
Is Twitching in the Bottom of Your Foot Scaring You?

If the twitching in the bottom of your foot is driving you mad, this article is a must-read.
Twitching in the bottom of the foot may at first seem innocent enough, and at the most, just a nuisance.
It may be most prominent while you are seated in a relaxed position, or reclined in a comfortable chair.
The problem with twitching in the bottom of your foot occurs when you decide to search the Internet about this, and are led astray by ALS sites or even multiple sclerosis sites.
Though you learn that muscle twitching (called fasciculations) can have quite a few benign causes, for some reason you zero in on what’s actually the least likely cause: ALS.
You zero in on this because it’s also the deadliest cause. This is how the mind can work.
YOU ARE NOT ALONE.
I was once reading a forum thread regarding the issue of fasciculations.
This phenomenon is often referred to as benign fasciculation syndrome when it becomes frequent and annoying enough.
People with benign fasciculation syndrome may spend too much time perusing the ALS sites and even reading the forums on these sites, going as far as registering and getting involved to collect more information.
Every time they have a fasciculation, the fear ALS. In that forum I had once read, somebody summed it up beautifully: “This thing really messes with your head.”
So what can be causing the twitching in the bottom of your foot?

Shutterstock/Pamela Au
“There are many causes for muscle twitching, most of which are benign,” explains neurologist Dr. Mary Dombovy, a neurologist with Rochester Regional Health in New York.
Dr. Dombovy continues, “Most people will have at least some episodes of muscle twitching during their life and if it is isolated to one area and not associated with other symptoms and goes away in a few hours or days, you don’t need to see a doctor.
“Some common causes of muscle twitching include exercise, particularly prolonged exertion, electrolyte abnormalities, muscle or nerve injury, muscle or nerve disease (most of which is not ALS).”
Massage the bottom of your foot if it continues to twitch, and curl the toes in and release them, alternating this way, to give the foot some exercise.
Drink plenty of water, as dehydration can also be causing the fasciculations.

Freepik.com
Anxiety can aggravate this symptom. Try to relax, meditate, strike some yoga poses, relax in a hot tub, listen to some soothing music – anything to calm your nerves and restore some positive thinking.
Like that one forum participant said, an obsession with fasciculations can really mess with your head.

Dr. Dombovy completed her neurology residency at Mayo Graduate School of Medicine. She is board certified in both neurology and physical medicine and rehabilitation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/cunaplus
Why Does Anxiety Cause Muscle Twitching?
Anxiety can cause muscles to twitch, and this includes stressing over this very situation.
It’s common for a person, who’s been experiencing twitching muscles, to notice an increase in frequency and/or a “spreading” of the fasciculations in relation to increased anxiety over this.
How is it that anxiety, even if it’s about finances or workplace security, can cause muscles to twitch?
“Persons with anxiety or panic attacks have higher levels of excitatory neurochemicals such as epinephrine and norepinephrine,” explains neurologist Dr. Mary Dombovy, a neurologist with Rochester Regional Health in New York.
“In essence they are having a ‘misdirected’ fight or flight response. These neurochemicals cause the feeling of anxiety, increased heart rate, increased blood pressure and tremors or twitching.
“When one is in this state, they are also hyperalert, and external stimuli such as a sudden noise may cause a startle response.”
The Fight or Flee Response
This is the body’s way of preparing for … a fight or flight … to a perceived danger.
We inherited this reaction from our primitive ancestors, who needed this response to survive in the harsh wilderness with wild animals.
In a modern world, we continue to perceive threats that trigger this survival response.
Except the threats aren’t dangerous and thus don’t require a fight or flight, such as being stuck in a traffic jam, trapped in a stressful business meeting or stressing about mounting debt.

Freepik.com
The body doesn’t distinguish between facing a wild animal and balancing the checkbook.
Stress causes the increased heart rate and blood pressure, and the muscle twitching.
The fasciculations are the body’s way of revving up for the fight or flight.
Anxiety over this will almost always intensify the twitching. Stress management is key to subduing this annoying reaction to a perceived threat.
The best way to battle stress is with regular rigorous exercise.
Intense exercise causes increased production of hormones that counteract another hormone that we’ve all heard of: cortisol, the “stress hormone.”
Exercise also promotes changes in the brain that lead to a mellowing effect and clearer thinking.

Freepik.com, javi_indy

Dr. Dombovy completed her neurology residency at Mayo Graduate School of Medicine. She is board certified in both neurology and physical medicine and rehabilitation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Twitching Arch of Foot: Causes, and Should You Worry?

If the arch of your foot has been twitching lately, you need to read this information.
Twitching in the arch of the foot can be very annoying and distracting, but this doesn’t mean it more likely is a serious problem than is not a serious problem.
Have you been reading too many ALS sites and are now scared you might have this deadly disease, since muscle twitching (fasciculations) can be a symptom?
“There are many causes for muscle twitching, most of which are benign,” states neurologist Dr. Mary Dombovy, a neurologist with Rochester Regional Health in New York.
“Most people will have at least some episodes of muscle twitching during their life, and if it is isolated to one area and not associated with other symptoms and goes away in a few hours or days, you don’t need to see a doctor.”
The thing about fasciculations in the arch muscle of your foot is that this location makes the experience particularly bothersome.
But just because something is bothersome doesn’t mean you should worry about it.
What could be the cause of the twitching in the arch of your foot anyways?
Many things could explain it.
Dr. Dombovy says, “Some common causes of muscle twitching include exercise, particularly prolonged exertion, electrolyte abnormalities, muscle or nerve injury, muscle or nerve disease (most of which is not ALS).”
Shutterstock/ Phase4Studios
Though “muscle and nerve disease” are mentioned here, this does not mean that these are the most likely causes of your situation.
They are in the list because these conditions can cause fasciculations. So can Lyme disease, which is caused by getting bitten by a tick.
The arch of the foot takes a good beating every day; all your body weight is on it as you walk and especially as you exercise. This area is subject to plenty of fatigue.

Shutterstock/zoff
Don’t forget that inadequate water intake can also cause fasciculations, and so can insufficient potassium and magnesium, two important minerals.
The key is if you have other symptoms such as weakness, numbness, cramping or pain.
However, cramping could be the result of an overworked arch muscle or even improper footwear.
Pain can be from plantar fasciitis, a benign but sometimes very painful condition. If discomfort is troubling, see a doctor.
“Neurologists have the expertise to sort out the cause by taking a complete history, performing a clinical examination and often performing nerve conduction studies/electromyography, and blood tests,” says Dr. Dombovy.
“If the cause is benign and the symptoms quite bothersome, there are also medications that can help decrease the twitching.”

Dr. Dombovy completed her neurology residency at Mayo Graduate School of Medicine. She is board certified in both neurology and physical medicine and rehabilitation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Pamela Au
Tiny Red Bumps on Neck: Causes, Solutions
Are you flustered over all those tiny red bumps on your neck and wondering what’s been causing them?
If you have a situation on your neck that can be described as “tiny” or “small red bumps,” this has several possible causes.
“Bumps on the neck are often caused by ingrown hairs resulting from having the neck or head shaved,” says Glenn Kolansky, MD, with Advanced Dermatology Surgery & Laser Center of NJ.
Continues Dr. Kolansky, “This is especially common in patients with curly or coarse hair that grows under the skin.
“Treatment options include topical antibacterial agents and prescription cortisone to decrease the inflammation. The best treatment is to stop shaving the areas involved.”
If you must shave the affected area, make sure that it is thoroughly moisturized first with a cream or shaving gel, and make sure that it isn’t the shaving medium that’s causing an allergic reaction.
Experiment with different brands, and then shave as gently as possible with a clean new blade.
Other causes of little red bumps on your neck
Two more possibilities are bacterial or fungal. Bacteria can build up as a result of carbuncles, boils and acne.
Treatment is antibiotic creams and in more severe cases, laser, draining or surgery.
Another possible cause is a fungal infection. There will also be itching and likely discoloration. Topical anti-fungal creams are the treatment.
Let’s not forget that contact dermatitis can cause little red bumps on the neck.
This condition can be triggered by irritants or allergens like cosmetics, strong soap, chemicals and even clothes.
Treatment is corticosteroids, antihistamines and of course, removing the offending agent.
Dr. Kolansky has received the Physician of Hope Award presented by the American Cancer Society and has lectured at local and national meetings.
has received the Physician of Hope Award presented by the American Cancer Society and has lectured at local and national meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com/wayhomestodio
Neck Rash: Many Causes and Many Treatments
What looks like a neck rash may not even be a rash and instead be skin cancer.
You’ve developed a neck rash and it may seem like nothing more than an annoyance, but it can have many different kinds of causes.
A true neck rash develops rather suddenly; it’s quite visible when just last week, the area looked perfectly fine.
Chances are very tiny that something that presents like this is skin cancer, since non-melanoma skin cancer grows very slowly.
What is the most likely cause of an actual neck rash?
It “can often be caused by a reaction to clothing or starch or sizing in shirts,” says Glenn Kolansky, MD, with Advanced Dermatology Surgery & Laser Center of NJ.
“It also can be an allergic reaction to type of product placed on the neck including cologne or aftershave.”
How is this type of neck rash treated?
“First is to try to figure out the agent causing the problem,” says Dr. Kolansky. “Treatment is often a topical cortisone agent, over the counter hydrocortisone. If that does not work, a prescription strength product may be required.”
What else can cause a rash appearance on the neck?
Squamous cell carcinoma, a skin cancer that kills about 3,500 Americans every year. The skin cancer can resemble a rash (when it’s not ulcerating,), but it’s not a rash.

Squamous cell carcinoma, ulcerating
Basal cell carcinoma. The same goes for this skin cancer as far as what it may resemble.
It grows extremely slowly and doesn’t metastasize, but it should be treated if you don’t want local destruction of tissues.

Basal cell carcinoma. Shutterstock/Dermatology11
Actinic keratosis. This is sun damage and only looks like a rash. It must be treated or it runs a 5-10 percent change of morphing into squamous cell carcinoma.
Treatment options for the cancer: surgery, topical prescription cream (basal cell); for the actinic keratosis, treatment is either liquid nitrogen or a prescription topical cream.
Actual rashes on the neck other than contact irritation
Eczema, candida fungus infection, viral infection, poison ivy, bug bites, acne, perfume allergy and atopic dermatitis (image above).
Careless shaving can also cause a rash on the neck. If you nick your skin, bacteria can take up residence and inflame the hair follicles (folliculitis).
Avoid shaving against the grain of the hairs to minimize this problem.
The inflammation may be treated with corticosteroids or antibiotics.
Dr. Kolansky has received the Physician of Hope Award presented by the American Cancer Society and has lectured at local and national meetings.
has received the Physician of Hope Award presented by the American Cancer Society and has lectured at local and national meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Beet Red Stools vs. Poop Stained with Menstrual Blood

Can a woman tell the difference between stools that have beet juice mixed in them and poop that has menstrual blood mixed in?
I’ve got this down, having ingested my share of beets, and of course, being a menstruating woman.
I am no stranger to closely inspecting my stools; I don’t get grossed out cutting them apart with a spoon and getting up close.
I began doing this when I developed microscopic colitis, and since then, I have no problem doing this.
Menstrual blood can easily get mixed in with stools, especially soft poop or diarrhea.
Red stained cervical fluid can make contact with stools as both exit a woman’s bottom at the same time.
The result is red or pinkish/brown gobs of mucus on the poop that seem part of it.
Menstrual blood is often in clot form.
Either way, it is a dark red with absolutely no hint of magenta or fuchsia, as is the case with beet juice.
Now note the fuschia color in the image above of the beet juice.
Since beet juice is pervasive and easily diffuses, it can find its way into cervical fluid that just might happen to drip out at the same time as a bowel movement.
Menstrual blood that’s mixed with stools will not easily stain a napkin or toilet tissue if you place the poop on the paper and break it apart.
However, beet juice will; it’s thin and instantly diffuses into the paper, staining it a magenta-red or fuchsia-red.
A woman may be far from her period, but upon seeing that tinged cervical fluid, might conclude there’s blood coming out of her vagina.
In reality, of course, the “blood” is beet juice that got mixed in with the cervical fluid.
Mucus also comes out with a bowel movement; this fluid helps with transit.
Beet juice doesn’t discriminate; it will find its way to intestinal mucus, so that you end up seeing tinged mucus with your stools.
Because intestinal mucus and cervical fluid look so much alike in the toilet water, one can easily mistake beet-juice-tinged intestinal mucus for blood-tinged cervical mucus. This is scary.
Keep track of when you eat beets. Don’t be afraid to get familiar with what stools and mucus look like close up.
There are telltale differences between menstrual blood and beet juice.
NOTE: Whenever in doubt, consult with a physician.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Red Stools from Beets vs. from Blood: Comparison

If you had beets several days ago and are now wondering if the red in your stools is blood, there are some signs to look for that distinguish beet red from blood red in your poop.
Men are at a disadvantage here, because they don’t have the experience that women have at seeing a lot of blood in the toilet bowl (from menstruation).
But even a woman can have difficulty telling the difference between beet red from blood red in her bowel movements.
How to Tell the Difference Between Red Poop from Beets and from Actual Blood
Fresh blood on toilet paper in pure form (as would be from rectal/anal bleeding) is solid bright red. Think of how Kleenex looks when you hold it to a bloody nose.

Shutterstock/Parinya Art
From my experience with beeturia (undigested beet juice in stools, though this term usually applies to urine), the juice that appears on the tissue paper is very diffuse, creating a very light reddish-magenta or very light reddish-fuchsia.
It’s a color that menstruation just does not produce.
Again, a man can’t make the comparison unless he has a history of hemorrhoid bleeding.
In all my years of menstruating, I’ve never seen even the slightest fuchsia or magenta tinge to any amount of blood on the tissue paper.
When it’s mixed with cervical mucus, however, it’s dark pink, but a dull pink, with no hint of magenta or fuchsia, and usually, the pink has a tinge of tan.
Blood in a toilet bowl will not diffuse as much into the water as will beet juice because it’s heavier and tends to aggregate.
Have you ever had a drop from your nose or a cut fall into some water?
It does not stain the entire contents, but stays rather localized, suspended in a glob.
I’ve had rectal bleeding after a colonoscopy, and trust me, pure fresh blood dripping into a toilet bowl does not disperse and dye the water; it remains suspended, aggregated, in ” liquid clumps.”
Beet juice is too thin to do this and will stain the water bowl pinkish if there’s enough of it.

Beet juice. Shutterstock/Africa Studio
However, in smaller amounts, it will remain concentrated around your stools—at least in my case it does.
Sometimes beet juice will form ribbons or rings that hover or float around poop. Actual blood in poop will be literally mixed in with it.
Beet juice tends to hover around stools like a halo, and in the water, it is crimson when it does this.
If you flush poop that’s red from beets, the juice will easily billow out into the water bowl, coloring it pink, red or reddish brown (if the poop is soft enough to mix with it).
Another test to tell the difference between beet red and blood in your stools.
Place several chunks of the colored stool on several layers of tissue paper or napkins, then roll them over to see what kind of stain they leave.
If it’s beets, the stain will be markedly magenta or fuchsia.
If you see a stain that resembles this color on your toilet paper, chances are extremely high that it’s from beet juice.
I hope this provides reassurance about beet poop vs. bloody poop.
This color will match the color the beets left behind on your cutting board or paper plates.
If it’s blood (from the lower intestinal/rectal/anal region) it will be pure red or red with a tinge of dark orange. It will retain this color when it dries.
Beet juice will quickly change to a light brown or dark gold or golden-brown.
“All stool that is black, maroon or red does not necessarily represent a gastrointestinal bleed,” says G. Shelton McMullan, MD, board certified gastroenterologist with Capital Digestive Care in MD.
“What we have recently eaten or ingested is often the culprit, and this needs to be considered before becoming alarmed.
“There are a host of foods that can make our stool red as well, including red Jell-O and beets.
“To err on the side of caution, it is recommended that you let your healthcare provider know if your stool remains discolored, however.”
 Dr. McMullan has published numerous medical abstracts and presented posters related to the management and treatment of inflammatory bowel disease and other gastroenterological conditions.
Dr. McMullan has published numerous medical abstracts and presented posters related to the management and treatment of inflammatory bowel disease and other gastroenterological conditions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Timolina
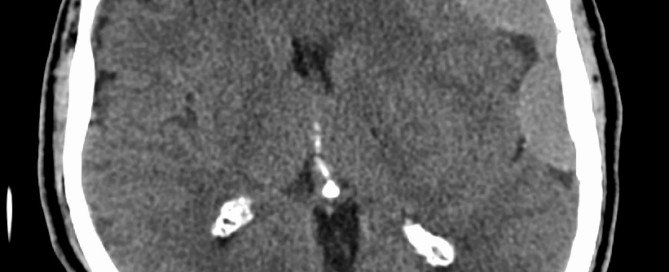
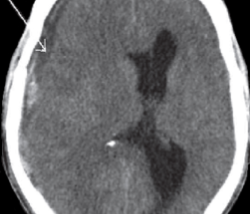
Normal CT Scan After Hitting Head: Brain Bleed Can Still Occur
A negative CT (CAT) scan after hitting your head doesn’t guarantee that bleeding in the brain won’t eventually result.
It still might, and when it does, it’s called chronic subdural hematoma (cSDH).
This happened to my mother who hit her head on a bathtub after passing out while standing.
You can imagine how hard she hit her head, since she wasn’t conscious to try to break the fall a little.
Several hours later she had a CT scan that looked perfectly normal.
She was kept for overnight observation. I was told that if her brain began bleeding, there would be neurological signs of this, that would be evident when nurses would give her neurological checks every so often.
Next morning she had another CT scan, and it was perfectly normal.
I asked the doctor about the possibility of bleeding still occurring in her brain, at some point down the road, since I had read reports in the past that getting hit in the head can cause delayed bleeding in the brain …
… up to two months later.
The doctor said there was a very tiny chance of this occurring, but that chances are, it wouldn’t, since the second CAT scan was completely normal.
My mother was discharged and I forgot about the possibility of delayed bleeding in the brain.
Six weeks later she awakened with a blazing headache and profound weakness in her legs, which I thought was a stroke.
I didn’t even think about that she had struck her head six weeks prior.
I kept thinking stroke because she had been taken off a blood thinner, Coumadin, which was prescribed for stroke prevention as a result of undergoing mitral valve replacement. The Coumadin prescription was for 90 days.
Shortly after hitting her head in the bathroom, the surgeon recommended that she cease the blood thinner because she was at risk for falling, due to unexplained orthostatic hypotensive episodes.
So she ceased the Coumadin after only 60 days. The morning she awakened with the headache and weakness was day 90 from the valve replacement surgery.
So I thought that the mitral valve replacement, in the absence of the 90-day Coumadin treatment, had resulted in a minor stroke.
The ER doctor assessed my mother and concluded that it was probably a small stroke.
Interestingly, the ER doctor never thought to ask if my mother had recently hit her head!
Because a stroke was suspected, my mother underwent a CT scan with contrast dye.
The ER doctor came back with the results and admitted being surprised at the findings: no stroke, but … bleeding in the brain.
Only then did the ER doctor ask if my mother had hit her head recently, and I was flabbergasted that all this time, I had etched the bathtub incident out of my mind.
Some of the blood in her brain was “old,” and some was “fresh.”
The diagnosis was a chronic subdural hematoma – a slow brain bleed whose primary cause is getting hit in the head.
“Elderly have weaker everything due to age,” says Danielle DonDiego, DO, a family physician with SteadyMD, an online program where patients can call, text or video chat with their doctor anytime.
“They are much more likely to have a brain bleed due to fragility from age.
“Also, many elderly are taking aspirin or a stronger blood thinner for health purposes, and this alone puts anyone at a higher risk.”
At the time my mother had hit her head, she was on the Coumadin as well as a daily aspirin.
Not Elderly?

Shutterstock/G-Stock Studio
The takeaway message here is that if you hit your head, record the date this happened, even if you’re young.
Not being elderly does not make you immune to bleeding in the brain after striking your head.
The other two types of subdural hematoma are “sub-acute” and “acute.”
Sub-acute is when the bleeding in the brain occurs three to 21 days after getting hit in, or falling on, one’s head.
The acute form has a very high mortality rate.
A normal CT scan shortly after hitting your head is always reassuring, but it doesn’t mean you’re out of the woods.
 Dr. DonDiego, who’s also a certified personal trainer, focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
Dr. DonDiego, who’s also a certified personal trainer, focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image credit: James Heilman, MD
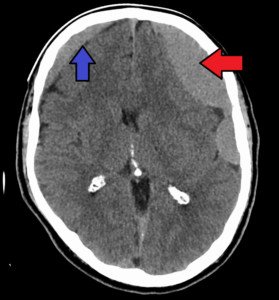
Burr Hole Subdural Hematoma Drain and Headaches, Neck Pain

Burr hole drainage is a standard treatment for chronic subdural hematoma, but what if the patient then complains of frequent and/or really bad headaches, or even nasty neck pain?
How common are headaches or neck pain after burr hole draining of a chronic subdural hematoma?
“Headache is a fairly common complaint after a burr hole washout of a subdural hematoma,” says Kangmin Daniel Lee, MD, a neurosurgeon with New Jersey Brain and Spine.
“Pain fibers are carried in the dura, and since the dural covering is opened to drain subdural hematomas, this can be one source of headache.
“Also, if there has been incomplete evacuation of the hematoma, this can also be a source of headache.
“Finally, there is often incisional pain which can be disguised as a headache.”
My mother had a burr hole drainage of her chronic subdural hematoma.
That day, following the surgery, and for a few days after, she complained of headaches.
But they weren’t nearly as bad as the headache (from the chronic subdural hematoma) that she suffered prior to the surgery.
I assumed it was only natural to have a headache after surgery on the head.
I’d ask my mother to place her fingers where the headache hurt the most, the “epicenter” of the headache pain, and she’d always place her fingertips smack on the incision area.
A few days after the burr hole drainage, my mother experienced sudden-onset neck pain.
The first time was in the morning, when I wasn’t there to observe it.
The second time, in the evening, I observed it. She was in agony, writhing and sounding as though she were in labor.
So how was this neck pain associated with the burr hole draining of the chronic subdural hematoma, if at all?
Dr. Lee (who was not my mother’s neurosurgeon) says, “Neck pain is not common, but would not be unusual, as headaches can be associated with neck pain frequently.”
One nurse suggested that the way my mother had been positioned on the operating table had caused a muscle to spasm in her neck.
Another nurse suggested that the neck pain was caused by my mother’s ongoing bed rest in virtually the same position.
I didn’t believe these were causes of neck pain that was agonizing enough to make a woman appear that she was in the process of giving birth.
The first nurse then suggested that the neck pain was caused by nerve endings from the brain being fired off from the burr hole draining procedure, and that these nerves extended into the neck.
The neck pain, both times, had been subdued with a hot pack and Vicodin.
Postoperative headaches, then, are to be expected, following burr hole drainage of a chronic subdural hematoma.
But beware if the headaches start becoming worse and more frequent.
This could signal a recurrence of the chronic subdural hematoma (there is a 15 percent recurrence rate).
This happened to my mother; she had a recurrence, and at some point on the headache continuum, the cause of the headaches transformed from postoperative and incisional, to a recurrence of the chronic subdural hematoma.
Ten days after the burr hole drainage, the headache pain was so unbearable that she couldn’t sleep through the night.
A few other new symptoms were present, convincing me she had a recurrence of the chronic subdural hematoma (or, to put it another way, perhaps the burr hole draining wasn’t complete, and residual fluid and leaking continued to build up).