Fever Feeling with Fibromyalgia: Causes, Treatments

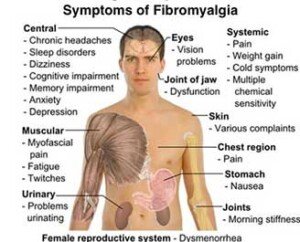
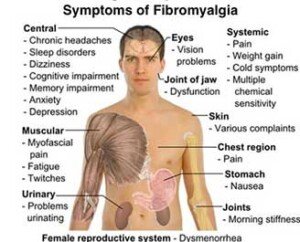
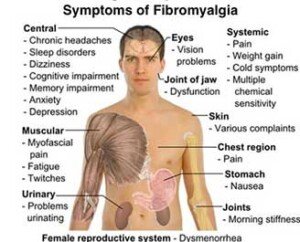
Many with fibromyalgia experience a fever-like feeling, but there is something you can do to help alleviate this.
If you have fibromyalgia and feel like you have a fever, this doesn’t mean you actually have a fever.
“Although people with fibromyalgia often feel feverish, they normally have low temperatures under 98,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“I consider anything over 98.6 to be a fever in fibromyalgia,” he continues. “If chronic persistent temperatures over 98.6 are present, I look for evidence of infections (e.g., sinus, dental, lung or bladder).”
You can have one of these infections and not even know it, other than being aware of the fever feeling.
“For sinusitis, treatment with antifungals are necessary, as this is the root cause of sinusitis,” says Dr. Teitelbaum.
In people with this pain disorder who feel as though they have a fever, there is usually no infection source to be found, adds Dr. Teitelbaum.
“In these cases I do recommend an empiric trial of the antibiotics doxycycline or Zithromax for six weeks to see if it helps the fibromyalgia.
“Also, have you ever had a course of antibiotics that also improved your fibromyalgia symptoms?
“I am amazed at how often the answer is yes, but then the doctor refuses to repeat the antibiotics.”
For these particular cases, Dr. Teitelbaum prescribes an extension for the antibiotic that had improved the symptoms of the mysterious pain disorder.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
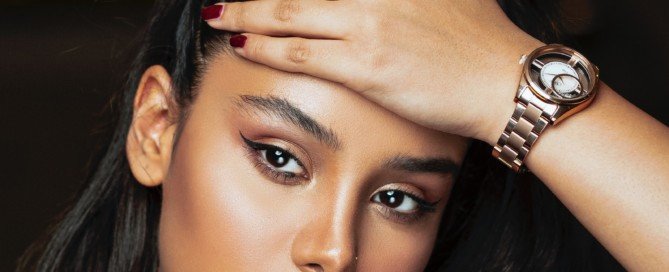
Why Fibromyalgia Can Cause Scalp Pain; Treatment
It’s no secret that fibromyalgia can cause pain in your scalp, and many frustrated patients suffer with this problem.
The pain of fibromyalgia is body-wide, so it shouldn’t be surprising that it extends to the scalp. Nevertheless, why does this occur?
“This often comes from the scalp muscles being tight if it’s diffuse,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“…or can be referred to the top of the head from neck muscles where they attach to the skull,” he continues.
“In addition, allodynia is another kind of pain that may be present in fibromyalgia.” Allo means other, and dynia means pain.
“Allodynia refers to when light touch on the skin is painful,” adds Dr. Teitelbaum.
“It is associated with increased activity of a neurotransmitter called NMDA, and generally responds to overall treatment of the fibromyalgia.”
So what treatment is best if you have scalp pain coming from fibromyalgia?
Dr. Teitelbaum recommends the low cost generics Ultram and Neurontin over the pricey and, as he says, less effective Savella, Cymbalta and Lyrica.
He also recommends End Pain by Enzymatic Therapy, and Curamin by EuroPharma.
For both of these, take two caps three times daily, over six weeks to reap the full effect. Then the dose can be lowered.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Difficulty Breathing, Tight Chest & Fibromyalgia: Solutions

Fibromyalgia may actually be the cause of your shortness of breath and tight chest, so here’s what a top FMS doctor says you can do about it.
“Shortness of breath, or a sense of breathlessness, sometimes associated with chest tightness is a common symptom in fibromyalgia,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
There are three main categories of breath shortness in ibromyalgia, says Dr. Teitelbaum:
Exertion-caused shortness of breath and/or chest tightness
This may be angina and thus requires testing by a cardiologist. “Once heart problems or lung problems are ruled out,” says Dr. Teitelbaum, “then treatment with ribose, coenzyme Q 10, and acetyl-L-carnitine can help.”
Feeling like you can’t take a deep enough breath, with no accompanying anxiety or dizziness?
“This is very common and likely comes from tight muscles in the chest,” says Dr. Teitelbaum.
“An excellent study over 15 years ago by the acupuncturists and physician Neoh Aum Choo, MD, showed that three acupuncture points at the base of the skull on each side could relieve this sense of breathlessness in fibromyalgia,” continues Dr. Teitelbaum.
“Simply putting pressure on, or massaging, these points can be very helpful in relieving the feeling of shortness of breath.”
Hyperventilation
“When the shortness of breath is associated with feeling of inability to take a deep enough breath, numbness and tingling in the fingers and especially around the lips, and anxiety,” begins Dr. Teitelbaum, “it most often comes from hyperventilation.
“This is basically a severe anxiety attack, where feelings that have been buried earlier bubble to the surface during periods of relative calm.”
This explains why these attacks typically occur when you are relaxed watching TV or reading—stress-free activities.
“Taking rapid deep breaths for 30 to 60 seconds will dramatically flare symptoms confirming the diagnosis,” continues Dr. Teitelbaum.
“Unfortunately, this can also trigger a full-blown panic attack.” Thus, it’s advisable to do this at home.
“Doing calming exercises, as well as letting your stomach expand out at the end of each breath will allow more air into your lungs and can also help end the hyperventilation attack.”
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Aaron Amat
Twitching Muscles and Fibromyalgia: Natural Solutions

A leading fibromyalgia expert comments about muscle twitching and what you can do about this.
Many people with fibromyalgia experience twitching of their muscles. This can be very annoying and even interfere with sleep.
“Muscle twitching, called fasciculations, are very common in fibromyalgia,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“They will decrease after proper treatment with the SHINE Protocol for fibromyalgia (Sleep, Hormones, Infections, Nutrition, Exercise),” continues Dr. Teitelbaum.
People without the pain disorder have been known to experience a lot of benign muscle twitching, and one of the most recommended solutions is magnesium.
“Magnesium is especially helpful,” says Dr. Teitelbaum. This is because this mineral, if insufficient in your body, can lead to fasciculations or make existing fasciculations more pronounced.
The SHINE Protocol consists of:
• Sleep. Get 8-9 hours!
• Hormones. See an endocrinologist to get tested for any hormone deficiencies.
The blood testing is very thorough but worth it, as hormone deficiencies can play a role in your pain disorder.
• Infections. An infection can contribute to, or even cause, FMS. You may have an infection and not even know it.
A perfect example of a sneaky infection is that of sinusitis, which can cause headaches that you think are solely caused by fibromyalgia! Get prompt treatment for all infections.
• Nutritional supplements. Acetyl l-carnitine, glutathione and vitamins A, the B’s, C and D will help reduce muscle twitching when taken in therapeutic doses.
• Exercise. Though FMS can cause exercise intolerance, following the four steps above will increase your tolerance.
Muscle twitching is most pronounced during inertia.
If you have fibromyalgia, exercise as well as you can, but keep in mind that exercise — particularly vigorous — can cause fasciculations (which is perfectly normal).
In fact, only the secondary mover in a strength exercise (e.g., triceps in the bench press) might end up being the muscle with the twitchies.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top of Head Pain from Fibromyalgia: Cause

Pain at the top of your head can be caused by fibromyalgia, and a top fibromyalgia doctor explains why and what to do about it.
“Fibromyalgia can cause a host of different pains, most often from muscle pain and sometimes from nerve pain,” including that at the top of the head, says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
What does the pain at the top of the head feel like to fibromyalgia patients?
“The nerve pain is characterized by sharp electric shooting type pains,” says Dr. Teitelbaum.
“Most of the other pains are associated with what are called ‘trigger points’ which are the ‘bunched up bellies’ of tight muscles or tender points where the tight muscles attach to the bones,” he continues.
The discomfort at the top of the head, which can also be described as the crown of the skull, is actually referred from an origin point that’s located at the base of your skull at the back of the neck.
In other words, the location of discomfort is distal from the origin of the problem.
The origin, at the base of the skull, back of the neck in those with fibromyalgia, consists of tight muscles — the tightness being “where they attach at the base of the skull in the back of the neck,” says Dr. Teitelbaum.
“This refers pain to the crown of the skull and behind the eyes.”
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Pinprick Sensations & Fibromyalgia: Cause, Natural Solutions

Fibromyalgia can sometimes cause a pinprick sensation in your skin. Why is this?
“Fibromyalgia can cause a whole range of nerve sensations including pins and needles (mostly in the hands and feet – called paresthesias),” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally.
His latest book is “The Fatigue and Fibromyalgia Solution” (Avery Penguin 2013).
“In the absence of other nerve problems such as severe localized weakness or numbness, these may be reasonably ignored,” adds Dr. Teitelbaum.
“Other nerve pains are also common in fibromyalgia and can be readily treated with natural treatments.”
A sensation of pinpricks can be difficult to ignore, even though you now know that they don’t mean anything serious as long as there isn’t any numbness or focal weakness.

Dr. Teitelbaum suggests a natural remedy for pinprick feelings that consists of a mineral, vitamins, an antioxidant and an amino acid, as follows:
• Magnesium: 200 mg a day
• Vitamins B6 (25 mg daily) and B12 (500 mcg daily)
• Lipoic acid (300 mg twice daily)
• Acetyl l-carnitine (1500 mg every day)
Can medications be useful in reducing pinprick sensations from fibromyalgia?
Yes, says Dr. Teitelbaum.
Ultram, Neurontin and Cymbalta are several examples of medications that can reduce or numb nerve pain. NSAIDs like aspirin are usually not effective.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Why Does Gastric Bypass Surgery Cause Belly Pain?
Pain in the belly following gastric bypass surgery can have a number of causes, and it’s not even that uncommon.
Also keep in mind that a major cause of this is the fact that you were just cut open in the stomach.
Belly Pain after Gastric Bypass Surgery: Here Are Some Causes
“Again, this can be benign from something as simple as indigestion or a tight abdominal wall muscle,” says pain specialist Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“But if it is a new pain, especially if it is severe and the surgery was recent, call your physician,” continues Dr. Teitelbaum.
“Any severe abdominal pain, especially if associated with vomiting without diarrhea, or with severe tenderness when pushing on the abdomen, should be checked.
“If the surgery was recent, concerns include a rupture or infection, or obstruction from an adhesion.”
These last few possible causes are life threatening. Waste no time getting to the emergency room.
What seems like even a minor delay can be the difference between life and death.
Another possible cause of pain in the belly region after gastric bypass surgery is that of kidney stones, since the procedure alters the way the body absorbs oxalate and calcium.
This problem, though, would not occur right away; it’s a possible long-term complication.
Interesting statistics regarding bariatric surgery:
A surgeon earns between $4,000 and $6,000 per operation.
A Fresno, California team of three physicians performed 1,128 gastric bypass operations in a single year.
The fatality rate is half a percent.
So in summary, though pain in the belly is not all that uncommon after a gastric bypass operation, it can also be a sign of something that needs immediate medical attention.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Lina Wolf, magenverkleinerung.tips
Source: gastric-bypass-surgery-lawsuits.com/pgs/gastric_bypass_statistics.html
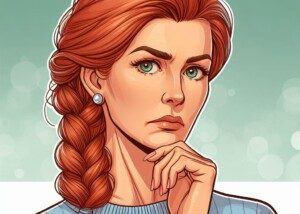
Can’t Sleep and Have Pain All Over? Solutions
If you’re suffering from pain all over your body but also from insomnia, find out what you may have.
If your entire body is suffering from pains or aches, and you have trouble with sleeping, these issues often go together.
Of course, body-wide pain can easily cause insomnia.
Here is information about when these two symptoms are independent from each other, that is, caused by a third agent.
And what is that third agent?
“Chronic widespread pain is becoming increasingly common,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “From Fatigued to Fantastic!”
“Unfortunately, most physicians are still clueless about how to evaluate this symptom. The first and key question to ask is, ‘Can you get a good night sleep?’
“If the answer is no and you have horrible insomnia associated with the widespread pain, it is likely coming from fibromyalgia or a fibromyalgia related process. If so, fatigue and ‘brain fog’ are also commonly present.
“This is true even if there is another problem such as lupus triggering the fibromyalgia.
Unfortunately, some physicians who have not stayed up-to-date with the science have a simple motto: IF I.”
What Dr. Teitelbaum is referring to is that of a doctor thinking, “If I don’t know what’s wrong with you, you’re crazy!”
Dr. Teitelbaum continues, “Then, instead of doing a proper evaluation, they may simply tell the patient that they are depressed.”
Though depression can cause body-wide pain, this article is about people who do not have any depression or diminished mood issues.
“If a good doctor does not know what is wrong with a patient, they will simply say so.”
Pain All Over Body, Insomnia, Fibromyalgia
Dr. Teitelbaum further explains, “My randomized double-blind placebo-controlled published research has shown that by treating with the SHINE Protocol (Sleep, Hormones, Infections, Nutrition, and Exercise), 91% of fibromyalgia patients improve with an average 90% increase in quality of life and more than 50% decrease in pain.
“The study and information on this can be found at www.endfatigue.com, and the free Symptom Analysis program on the homepage can be dramatically effective at helping you determine the cause of your fibromyalgia and how to effectively treat it.”
If you’ve been having trouble sleeping, along with pain all over your body, consider that this might be fibromyalgia.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/fizkes
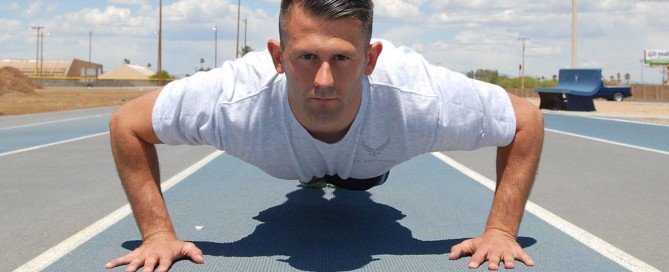
Are Pushups Painful Due to a Strange Lump in Wrist?
Does pain in your wrist make pushups difficult and you’ve now noticed a little rubbery lump in your wrist?
The lump may be tender if you press on it.
It’s not rock hard; it gives a little when you press on it, but it’s not super soft, either.
What is this strange painful lump in your wrist that messes up your pushups?
“The most common cause of a lump in the wrist is a small fluid filled cyst called a ganglion cyst,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“The good news is that it is quite benign and reasonable to ignore unless it is annoying you enough to need treatment.”
In other words, it’s not cancer and cannot turn into cancer. It also will not cause local destruction.
This odd but harmless mass stays the same size if one decides not to have it removed.

Ganglion cyst. Shutterstock/girl-think-position
Treatment for a lump in your wrist is something you should consider if it’s interfering with pushups.
I have a ganglion cyst and I must do pushups while grasping dumbbells or pushup handles on the floor.
This is no big deal and actually allows for greater range of motion.
However, a ganglion cyst can also cause pain when doing bench dips due to the positioning of the hands.
At one point in my life, it was causing pain while doing lying chest presses with heavy dumbbells as well as when pushing against handles for the seated chest press.
But that inconvenience was short-lived and eventually went away spontaneously.
Dr. Teitelbaum says that “treatment includes putting a needle in to drain the cyst or surgically removing it. Recurrence is not uncommon with either of these options.
“The best option? Ignore it (as long as it does not cause pain). It may go away spontaneously.
“If you need to do something, I would begin with having the doctor simply put a needle in to see if it can be drained (depending on how thick the fluid inside the cyst is). I would save surgery as a last resort.”
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
When to See Doctor for Sharp Pain when Breathing
If you’re experiencing sharp pain when breathing, this may mean something quite serious that needs fast medical attention.
This can also mean something that’s nothing to worry much about.
Breathing that’s accompanied by a sharp kind of pain can be benign…or…it can be dangerous, says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“Because of this, if it is a new symptom you should check with your physician – especially if it is associated with shortness of breath, cold sweats or fever.”
When is sharp pain when breathing a serious issue?
“The worrisome causes include irritation of the lining of the lung (called the pleura) or the heart (called the pericardium),” says Dr. Teitelbaum. Pneumonia can cause this.
“In most cases, however, it simply turns out to be benign pain coming from tight chest wall muscles – most commonly along either side of the central chest bone (called the sternum) or on the chest wall two inches below the right or left nipple where the muscles attach.”
This problem is often referred to as costochondritis “because of the likely mistaken assumption that the pain comes from tender cartilage around the ribs and sternum,” says Dr. Teitelbaum.
The discomfort “usually originates in muscles that are tight, in areas called trigger points or the muscle insertions where they attach to the bones.
“A simple telltale? If pushing over the painful area (give a good hard push with your thumb) reproduces or relieves the pain, it is most likely to be muscle related” — perhaps caused by overdoing an exercise regimen in the gym or on the job lifting heavy items.
“If it does not, it is likely coming from something beneath the ribs – like the heart or lungs,” adds Dr. Teitelbaum.
Sharp pain while breathing that’s coming from the heart or lungs always warrants medical attention. Always. This is nothing to brush off — never.
“If you have ever eaten ribs at a restaurant you can see that they are pretty thick.
“Pushing on them is not likely to affect the organs underneath the ribs – but will affect the pain in the muscles overlaying the ribs.
“But see your physician anyway for this symptom, to be on the safe side.”
A rib fracture can also produce this scary symptom, though with a rib fracture, there will be visible bruising in the area of the fracture. There will also be tenderness in the area.
If you’ve been experiencing a sharp kind of pain when you take breaths, it would be a very smart idea to have a doctor check you out — even if you’re “young and healthy.”
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE certified personal trainer.
.