Mild Congestive Heart Failure’s Effect on Exercise

Mild congestive heart failure may not even be noticeable to the person who has it, even when they are exercising.
“Usually if the mild congestive heart failure comes on very gradually and it is only mild diastolic CHF, then it may not be noticeable or only noticeable with very rigorous exertion,” or activity that’s more than usual for the individual, says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
So if you’ve always gone out every morning to leisurely walk your dog for half a mile, and all along your diastolic heart function is getting a little worse such that it’s in the range of mild heart failure — you probably won’t be suddenly panting at the end of that half mile.
Diastolic CHF: The heart is stiff, not relaxing properly. It does not fill up with the right amount of blood to be pumped out.
Thus, less blood is pumped out, meaning less oxygen throughout the body.
“If it is more severe diastolic CHF, then it may be a more acute and rapid decline,” says Dr. Sayeed.
“If it is systolic CHF and the ejection fraction [pumping force] goes below 40 percent, then the symptoms may come on more rapidly and with minimal exertion like [walking] a block or two or one flight of stairs.”
Systolic CHF: decreased pumping function. The heart’s “squeeze” is not optimal.
Dr. Sayeed explains, “The fatigue is usually most noticeable with exertion, particularly stairs and inclines, and the patient may suddenly report not being able to go up stairs or a hill or do competitive sports, etc.
“Symptoms won’t be so apparent at rest or with things like golf or easy activities where it may go unnoticed.”
If you’ve been working out all along, it’s smart to keep a record of your key workloads, which may be measured in amount of resistance, distance, speed or time.
As we age, these values will gradually decrease, e.g., your fastest one-minute run on a treadmill may be 12 mph at age 50, but 11.5 mph at age 55. This is normal decline.
If a performance deficit, however, is suspiciously rapid with no explanation (such as recent injury), then this warrants a medical evaluation.
Congestive (chronic) heart failure can be one of numerous causes of an inexplicable deficit in aerobic stamina or strength.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Congestive Heart Failure Cause Only Edema?

Edema refers to fluid retention such as that in the lower legs that causes swelling, but can this be the ONLY symptom of congestive heart failure?
Can a person feel and function just fine otherwise, despite the puffy lower legs and ankles from the congestive heart failure’s edema?
Congestive heart failure can cause numerous symptoms, including the fluid retention of edema.
Sometimes, this backed-up fluid goes higher than knee level, affecting the upper legs and even the groin area.
“Congestive heart failure can just cause edema and no other symptoms if it is due to purely right [heart] sided failure,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“But this is rarer, as right sided failure is usually caused by left heart failure which would cause dyspnea.”
The “failure” refers to the heart’s right or left ventricles failing to perform efficiently. And dyspnea means shortness of breath.
In heart failure, the pumping action of this organ is either inadequate, and/or the heart’s chambers don’t refill with as much blood as they should prior to each beat.
The end result is an insufficient supply of oxygenated blood circulating throughout the body.
So what this all means is that many more times than not, a patient will have, in addition to edema from the congestive heart failure, a problem with shortness of breath or getting out of breath fairly easily.
For example, activities that historically did not leave the patient breathing hard, now leave him or her winded, such as walking up a flight of stairs, walking quickly on an inclined parking lot, doing housework or lightly playing with the grandkids in the backyard.
They will fatigue more quickly from day-to-day activities that had never tired them out before.
When the excess fluid is in the groin area, it can impose upon the bladder, reducing urine output. This fluid would be visible on a CT scan.
Other Symptoms of Heart Failure
In addition to edema and shortness of breath, CHF can cause nausea, appetite suppression, a cough with white or pinkish phlegm, and chest pain.
Consult with your cardiologist if you have any concerning symptoms including new-onset ankle or lower leg swelling in BOTH legs, which could signal congestive heart failure.
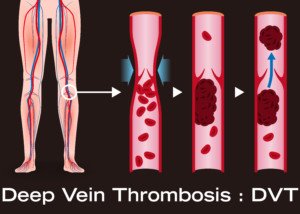
If you have new-onset swelling in only one leg, particularly the lower leg, this could be a deep vein thrombosis.
This needs immediate attention, as this blood clot could detach and very quickly travel to the lungs and be life threatening.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/futurewalk
Source: mayoclinic.com/health/heart-failure/DS00061
Fast Rotator Cuff Tendonitis Pain Treatment without Surgery

The procedure is minimally invasive, nonsurgical and provides immediate pain relief from rotator cuff tendonitis.
A minimally invasive procedure to treat tendonitis in the rotator cuff provides immediate symptom relief, according to a study.
For some patients, their rotator cuff can accumulate calcium residue and be resistant to physical therapy.
“Calcific tendinopathy often resolves on its own but can become chronic,” says Jessalynn Adam, MD, who specializes in primary care sports medicine with OrthoVirginia.
“Often, a combination of physical therapy and shoulder injection with/without percutaneous needle tenotomy is sufficient treatment.
“The U.S.-guided procedure is effective but is uncomfortable. Patients are often sore following the procedure for a couple of days as well. However, there are good results.
“A study demonstrated that at one year, patients who underwent needling had more improvement than simple cortisone injection alone.
“Surgery is uncommon for this condition and only indicated for patients with refractory symptoms for six months or more (about 10% of cases).”
Another study found that ultrasound-guided nonsurgical therapy significantly reduces pain from calcific tendonitis of the rotator cuff and restores lasting mobility after treatment.
The treatment resulted in a single and inexpensive approach that was effective, says the study’s author, Luca M. Sconfienza, MD.
In severe cases, patients may require shockwave treatment or open surgery to remove the calcium.
Open surgery requires a hospital stay and rehabilitation and, on rare occasions, may result in major complications, such as tendon rupture.
How the Procedure Is Done
For the 20-minute procedure, the shoulder is anesthetized and, with ultrasound guidance, a radiologist injects a saline solution into the rotator cuff to wash the area and break up the calcium.
A second needle is used to aspirate, or withdraw, the calcium residue. Recovery time is about an hour.
Complete absence of the pain, following only a single procedure, is not guaranteed, but may be well worth it for chronic sufferers.
Symptoms of Rotator Cuff Tendonitis
• Pain in the upper side of the arm when lifting the arm straight out at one’s side
• Same pain when reaching overhead, especially with straight arms.
• Same pain when slipping the arm through the sleeve of a coat or jacket.
 Dr. Adam specializes in the care of athletes and active individuals of all ages, offering prevention, diagnosis and treatment of sports and exercise injuries. Dr. Adam’s care focuses on muscle injuries and biomechanics.
Dr. Adam specializes in the care of athletes and active individuals of all ages, offering prevention, diagnosis and treatment of sports and exercise injuries. Dr. Adam’s care focuses on muscle injuries and biomechanics.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/xmee
Source: sciencedaily.com/releases/2009/06/090630074949.htm
Parkinson’s: What Cardio Exercise Intensity Works Best?
Find out what a study says about the best cardio intensity level for Parkinson’s patients.
Will those with Parkinson’s disease benefit more from low intensity cardio exercise or higher?
Researchers at the University of Maryland School of Medicine and the Baltimore VA Medical Center wanted to find out what would be a preferable exercise for those with this neurological disorder.
Study Results
The low intensity group experienced the greatest degree of consistent improvement in gait and mobility.
For the study, subjects with Parkinson’s disease walked on a treadmill and also did resistance and stretching exercise.
There were three groups:
1) 50-minute treadmill walk for low intensity, 2) 30-minute incline walk for high intensity, 3) resistance exercise for the legs.
All Parkinson’s groups exercised for three months, three times a week.
“These results show that exercise in people with Parkinson’s disease can make a difference in their function,” explains Lisa Shulman, MD, the lead study author, professor of neurology at the University of Maryland School of Medicine.
In the report she adds, “Exercise may, in fact, delay disability and help to preserve independence.”
People with Parkinson’s should strongly consider low intensity cardio workouts.
Walking on a Treadmill for Parkinson’s Disease
Based on this study, it appears that treadmill walking will produce the greatest benefits for ambulation, when compared to using other kinds of cardio equipment.
After all, to get from point A to point B, we usually walk rather than pedal or step upward.
Walking is the most natural form of human movement, so the treadmill is the obvious choice for improving ambulation.
As far as cardiovascular benefits, any cardio equipment will suffice.
Getting Started on a Treadmill
Those with Parkinson’s disease should begin slowly on the treadmill and work on avoiding the habit of continuous holding on, as this will reproduce a gait pattern similar to that of using a walker. The image below demonstrates this.

Continuous holding on can also lead to repetitive stress injuries in the hips, plus “mold” posture into an incorrect form.
As your balance improves, gradually increase speed.
Again, the key is starting out at a slow-enough speed rather than a speed that makes you feel too off-balance to let go.
When I was a personal trainer, I noted that whenever someone told me they feared falling off a treadmill unless they held on, they had the speed at least 3.5 mph and often had a high incline.
If you must start out at only 1.5 mph, or even just one mph, at zero incline, then do so.
Then from there, gradually increase your speed over time, but never too much that you feel that you’ll lose your balance.
Holding on momentarily for balance checks is encouraged, but again, do not get into the habit of CONTINUOUSLY holding on — and this assumes that you can already walk in day-to-day living without a walker or cane.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/Kristiana Gankevych
Source of Parkinson’s study summary: sciencedaily.com/releases/2011/04/110412162404.htm
Blood Clots (DVT): Q & A with MD about this Silent Assassin
Dr. Darren Klass answers questions about deep vein thrombosis, a potentially fatal type of blood clot that can strike anybody, any fitness level, any age.
Darren Klass, MD, is Clinical Instructor of Interventional Radiology at the University of British Columbia and the Vancouver Coastal Health Association.
In layman’s terms, what is DVT?
DVT is deep vein thrombosis; this term generally refers to the development of a clot in the deep veins in the legs and pelvis.
The deep veins in the legs run between muscle compartments and cannot be seen without medical imaging.
How is it caused?
DVT is caused by blood within moving veins clotting. The clot is cause by three factors:
- Slow flow in the vein
- Abnormal clotting factors in the blood which cause it to clot more than normal
- Damage to the lining of the vein
Are there ways to prevent?
There is no way of completely preventing blood clots without medication, which in itself has risks. Ways to decrease the risks are:
- Keep well-hydrated; dehydration thickens the blood.
- Avoid sitting in the same position for long periods of time (i.e., long plane flights).
- Avoid tight constricting clothing at the hip, which may squash the vein in the groin and slow flow.
How can I be on the lookout for a clot?
If one part of your leg (the calve, thigh or both) suddenly becomes swollen and painful, or suddenly veins which were not visible under your skin become more prominent, you should consult your family doctor.
What are the risks if it’s not caught?
DVT may cause little or no long term complications if treated early. If left untreated, the risks are the following:
- Piece of the clot may break off and travel to the lung causing a pulmonary embolism.
- The clot may extend into the main vein in the abdomen (termed the IVC) and stop the flow of blood from the pelvis and opposite leg, which may cause complications.
- If the clot involves the veins in the pelvis, this may require treatment in a hospital to break up the clot (thrombolysis performed by an interventional radiologist). The aim of the treatment is to clear as much clot from the veins as possible and allow healing of the vein.
If the vein is left untreated and the clot is absorbed by the body, the vein is often left scarred.
The scarring may damage valves in the vein, which can lead to a chronic swollen leg, which is difficult to treat and may cause significant limitation in everyday activity. This condition is called post-phlebitic syndrome.
What are the options for treatment of DVT?
DVT can be treated in the following ways:
Medication to thin the blood and decrease the risk of the clot extending.
However, the clot remains in the vein until the body reabsorbs it and the vein is often left scarred.
The clot can be removed by a minimally invasive procedure performed by an interventional radiologist.
The procedure involves using special medication and advanced equipment to break up the clot and remove it from the vein and restore flow immediately.
The procedure is done through a tiny hole made in the vein behind the knee and a very small cut in the skin about 3 mm in length.
 Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Cause of Heavy Bleeding after Missed Period

The cause of heavy bleeding in menstruation that follows missed periods is quite logical.
Many women wonder and are even worried about the cause of heavy flowing in a period after menstruation has been missed once or a few times.
“The cycle consists of estrogen stimulating the lining of the uterus (endometrium) and ‘building up’ the lining,” begins Dr. Marlan Schwartz, MD, FACOG, robotic surgeon with Lifeline Medical Associates.
“If this is not shed, and there are multiple reasons that could cause this, it will likely be kept being stimulated by more estrogen, thus causing the lining to be even thicker.
“If one then has a period or loss of this lining, as it has been made thicker (six or seven weeks of stimulation versus three weeks), there is more to shed.”
 Dr. Schwartz is the past Chairman of the Department of Obstetrics and Gynecology at Robert Wood Johnson University Hospital-Somerset.
Dr. Schwartz is the past Chairman of the Department of Obstetrics and Gynecology at Robert Wood Johnson University Hospital-Somerset.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Are There Reasons a Colonoscopy Can Miss Colon Cancer?

You know a colonoscopy can miss colon cancer, right? So find out exactly why, and what questions to ask your doctor.
Though a colonoscopy has saved the lives of many people by detecting precancerous polyps, it can also miss actual colon cancer.
“Endoscopy is not perfect and that’s tough fact to deal with as a gastroenterologist,” says Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
For average-risk people, colonoscopies should begin at age 45 — according to the U.S. Preventive Services Task Force — and be done every 10 years after.
“The 10 year interval as we all know is a negotiated time frame, not a date set in stone from God,” says Dr. Jones. “It’s the best estimate.”
The truth is, a colonoscopy can provide “incomplete protection,” adds Dr. Jones, which “usually lies with three factors.”
Three reasons a colonoscopy can miss colon cancer
#1. “Operator characteristics: Not all docs who do endoscopy do the procedure equally well,” says Dr. Jones.
“Many are benchmarking and working on continuous improvement, i.e., tracking fecal intubation rates, withdrawal times, adenoma [cancer] detection rates, of using split dose preps which better clean and prepare the right [sided] colon.
“These are questions any person having a colonoscopy should ask their physician.”
The second reason a colonoscopy can miss colon cancer is “anatomic considerations,” says Dr. Jones.
“It is impossible to see every square cm of the colon with any modality. There is a miss rate of up to 10% for 1cm adenomas, even by experts.”
Reason #3 for why a colonoscopy can miss colon cancer: “Biological issues: Right colon adenomas are much more likely to have an evolving pathology called serrated adenomas; these polyps evolve into cancer through a different pathway called hyper- methylation. They are not your mother’s colon polyps/cancers.
“They have several differences including a more flat nature, making them harder to identify, be obscured with mucus or stool, progress to cancer in a shorter time frame and be located obviously in the right colon, which is harder to reach.”
Dr. Jones advises high-risk people to request more frequent screening and to consider asking their doctor for a stool test between colonoscopies.
 Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
What if You Get a Pulmonary Embolism on a Plane?
Suppose a passenger on an airplane develops an apparent pulmonary embolism; what should, or CAN, you do?
A deep vein thrombosis can develop while a person is on an airplane.
What might be done for help if this DVT migrates and becomes a pulmonary embolism, and a doctor just happens to be on the plane—a doctor who has treated pulmonary emboli?
“You will not show signs of a pulmonary embolus on an airplane,” says Michael P. Zimring, MD, Director, Travel Medicine, LLC at Mercy Medical Center, Baltimore, Maryland..
“The PE usually breaks off from a clot starting in the lower extremities — and that takes a while to develop.
“You usually show signs of a pulmonary embolus after a significant time of first forming a clot in the leg. Sometimes it is fast, but not usually.”
In a hospital setting, the treatment for a pulmonary embolus is IV administration of a “clot busting” or thrombolytic drug.
Doctor on Airplane Suspects Passenger Has a Pulmonary Embolism
But what if a doctor on a plane suspected that a passenger had a PE (based on symptoms, risk factors), and that doctor just happened to have a clot busting drug and syringe in his medical kit?
These are fair questions for a layperson to wonder about.
Though thrombolytics carry the risk of dangerous internal bleeding as a side effect, it’s reasonable for a layperson to wonder about this if a passenger has an apparent pulmonary embolism and is 35,000 feet off the ground.
Diagnosing a Pulmonary Embolism
A pulmonary embolism cannot be confirmed based on just symptoms (sudden difficulty breathing, chest pain, coughing up blood) and risk factors for DVT (prolonged inertia in an airplane, obesity, smoker, among many others).
Back to that doctor on the plane. What if he also has a stethoscope and listens to the distressed airline passenger’s heart?
A pulmonary embolism can change the way the heartbeat sounds through a stethoscope.
Dr. Zimring explains, “A typical physician will not hear a strain of the right heart through a stethoscope, and no one will be able to detect a PE by physical means.
“No one would dare treat a pulmonary embolus by injecting a thrombolytic on a plane because there is no way he could be sure the patient has a PE.
“There are many factors to be taken in consideration before injecting a thrombolytic in the best hospital environment.
“In addition, the physician might not be covered under the Good Samaritan Laws if he did such a specialized procedure in an emergency situation.”
Prevention of Blood Clots Triggered by Air Travel
If you’re worried about developing a pulmonary embolism as a result of flying, take precautions:
Stay well-hydrated throughout the plane trip; exercise the calve muscles every 15 minutes during the flight; don’t be seated for more than an hour; and avoid alcohol.

Exercises during air travel
 Dr. Zimring has 40+ years of experience diagnosing and treating a host of medical conditions.
Dr. Zimring has 40+ years of experience diagnosing and treating a host of medical conditions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Quick Easy Way to Tell if Red in Stools Is Beet Juice

Here’s how to tell within seconds if the “blood” you see in your bowel movements is actually undigested beet juice.
I juice beets all the time, and I experience “stool beeturia” as a result.
Perhaps the biggest telltale sign that the red in your poops is from the beet pigment betain, is that it has a glowing, neon-like quality.
Even veteran beet eaters can still wonder if the red in their stools is blood, especially if they’ve recently had a digestive problem.
This is the same glowing, neon-like quality you see when a glass fills with the juice of a fresh beet being juiced.
Pictures of glasses of beet juice on the Internet don’t do this pigment justice.

Shutterstock/bitt24
Most website images of beet juice in glasses seem to be beet juice blends.
Read the descriptions; almost always, there are other items juiced into the beverage, such as carrots, blueberries, apples, celery or some leafy green.
This suppresses that glowering, neon-like color. If you juice ONLY beets, you’ll be struck by the amazing crimson glare.
It’s beautiful and bright. This quality is retained in your stools when betain does not get absorbed.
Blood in the stools does not look like this.
Though blood in the stools may be fresh (and “bright red”), it lacks that glow, that neon-like feature, that distinct ruby-magenta or crimson-magenta color, whereas blood is simply a solid red.
There’s a difference between crimson-magenta and solid red.
The exact color of betain in BMs seems to be 80 percent crimson, 20 percent magenta, with neon. This hardly describes blood, fresh or old.
As a woman, I’ve seen blood in the toilet with (NOT in) my stools as a result of menstruation.
If blood is being discharged from my vagina at the same time I’m having a bowel movement, the blood will sometimes get “mixed” with the poops.
I know what this looks like all too well. And it cannot pass for betain. Quite simply, betain often just GLOWS.

Freepik.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/KarepaStock
How Many Burps per Minute from Anxiety? How to Stop?
Wait till you find out how many times per minute anxiety can make a person burp.
It’s no secret that anxiety can cause burping, but just how much?
“In extreme cases, belching can occur up to 20 times a minute,” says Dr. David Robbins, a gastroenterologist at the Manhattan Endoscopy Center, NY.
“But in these cases it’s usually release of air from the esophagus back up into the pharynx without ever getting down into the stomach.”
The sound of a belch occurs when air escapes from the esophagus into the pharynx, says Dr. Robbins.
But he adds, “The most common type of belching originates when swallowed air from the esophagus enters the stomach, only to be released when the valve at the bottom of the esophagus relaxes.”
He refers to the type of burping, in which the released air was never in the stomach (only in the esophagus) as “supragastric.”
Most patients who have this type of burping “suffer from some element of anxiety,” continues Dr. Robbins.
“Studies have shown that the symptoms increase along with increasing stress. It’s also been described with obsessive-compulsive disorder and various eating disorders.”
So how does one stop burping 20 times a minute?

Shutterstock/Aaron Amat
“Interestingly, many patients can ‘squelch the belch’ while speaking,” says Dr. Robbins.
“This is basically a sort of distraction maneuver. This type of belching never occurs during sleep, again pointing to an active anxiety component.”
If you find yourself burping many times in just one minute, talking incessantly to squelch it isn’t practical, for obvious reasons.
What else can you do, then, besides making efforts to manage stress?
“There are no established treatment regimens for excessive belching,” says Dr. Robbins.
However, he adds, “Extreme cases require the help of a cognitive behavioral psychologist or a psychiatrist. Speech therapy and biofeedback have shown some modest results, while drugs such as simethicone (or Gas-x) have not.”
When circumstances are normal, says Dr. Robbins, burping “actually occurs up to 30 times a day” and is a “normal physiologic phenomenon,” even though we all have known at least one individual who can emit loud belches seemingly at will.
 Dr. Robbins is board certified in both gastroenterology and internal medicine. He has been invited to speak internationally and has published and lectured widely.
Dr. Robbins is board certified in both gastroenterology and internal medicine. He has been invited to speak internationally and has published and lectured widely.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.