Cause of DVT Weeks after Joint Replacement Surgery
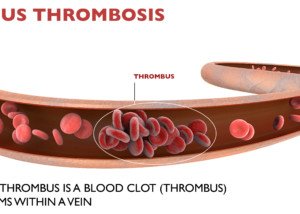
Shutterstock/Naeblys
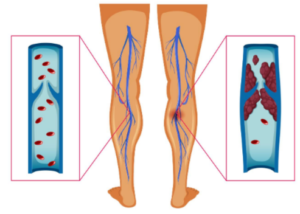
The “grace period” for DVT development after joint replacement surgery is 90 days, but why so far out if by then, the patient is walking?
Three months out from a knee or hip replacement surgery, a patient who has recovered well might be walking a few miles a day.
Despite that, the risk for a deep vein thrombosis is still present.
“Hard to say why one may get a DVT weeks after joint replacement surgery,” says Paul Lucas, MD, surgeon with the Vascular Center and director of the Vascular Laboratory at Mercy Hospital in Baltimore.
“Obviously, being sedentary is the main reason, but poor joint movement, lack of flexion ability….anything that may contribute to stasis [inertia] will be a risk….scar tissue, post-op inflammation/swelling within the knee space,” explains Dr. Lucas.
My father has had four joint replacement surgeries. For the fourth one, he was on Coumadin for only 10 days post-op.
Interestingly, the medical literature, in general, says that a patient is at increased risk for DVT up to 90 days after knee or hip replacement surgery.
DVT Risk Following Joint Replacement Varies from One Patient to the Next
Dr. Lucas says, “Some people have a hypercoagulable state [more prone to clotting] that they are not even aware of, and the insult of surgery triggers the DVT.
“Usually these people don’t get DVT unless another risk exposure presents, like surgery or a traumatic injury, etc.”
DVT Symptoms to Be on the Alert for
- Soreness, tenderness or cramp in the lower leg that is not relieved with rest.
- A cramp or other discomfort can also occur in the upper leg and pelvic area.
- The affected area appears suddenly bigger or swollen.
- The affected area may be reddisn/pinkish. It may also be pale or blanched.
- It may be exceptionally warm to the touch.
- In some cases, the affected vein can be felt by a finger, but this usually doesn’t happen.
- If you suspect you have a deep vein thrombosis, you need to get to the ER as soon as possible, even if the pain is only minor. A DVT can dislodge, travel to the lungs and become life threatening.
 Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Naeblys
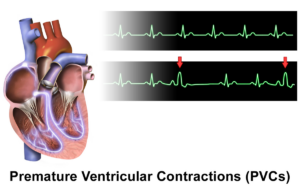
How Long in Length Can a DVT Be?
A doctor explains how long a DVT can measure in length; no wonder a breakoff can cause a massive fatal pulmonary embolism.
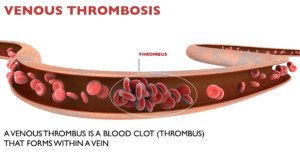
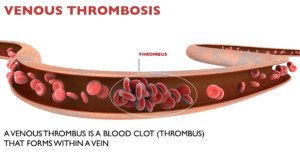
Perhaps you’ve always thought that a DVT, a blood clot in a deep vein, is the size of a BB, just a little bit of sticky blood matter inside a vein, only a centimeter or so long.
Length of a DVT
“In terms of length or extent of a DVT, they can range from those that are very focal (a couple of mm only) to extensive clot throughout the length of the leg, and even into the iliac veins and inferior vena cava,” says Paul Lucas, MD, surgeon with the Vascular Center and director of the Vascular Laboratory at Mercy Hospital in Baltimore.
In other words, a deep vein thrombosis can extend the length from the foot all the way to the heart, all in one vessel, that extends this length, and merges into the inferior vena cava, a major vein that transports blood from the lower body to the heart where it’s reoxygenated and recirculated.
A DVT that’s almost the entire length of the body has the potential for huge bits of it to dislodge.
And in seconds it can plug up the pulmonary artery where it splits off into each lung, causing near-instant death from a massive or “saddle” pulmonary embolism.
Length of Most DVT’s
“Obviously, most clots aren’t that extensive, but it’s important to note that they certainly can be,” says Dr. Lucas. “They can cause a myriad of symptoms from pain only, to swelling, or a combination of them.”
There are other, more benign causes of pain and swelling in the leg, but Dr. Lucas warns that if you have these symptoms and there’s no simple explanation (e.g., no recent hard run up a hill), you should at least think about a blood clot as a possibility and get the leg examined.
Both pain and swelling, especially in the lower leg, are worrisome, says Dr. Lucas, but not diagnostic for a DVT.
“In fact, no physical examination finding is accurately diagnostic of a DVT, but suspicion should be rendered. About 2-5 percent of people experience a DVT within their lifespan.”
It’s not true that the longer in length a DVT, the more prominent the symptoms will be.
A person can have a DVT that extends from foot to hip and not have symptoms, since in about half the cases, these blood clots present with no symptoms.
 Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Naeblys
You Suspect DVT; Ultrasound Negative; What’s Next Step?

Find out what testing you should insist upon if you suspect a DVT but the ultrasound turns up negative.
One of my articles on DVT is about Staci Stringer, who was told she did not have a DVT even though her calve was swollen and so painful that it was “hard to walk,” she says.
This sounds unbelievable, but it happens: An ultrasound will be negative for a DVT, even though there is one, and the patient just knows that the procedure missed it.
If you ever suspect a deep vein thrombosis but the ultrasound technician says there’s “nothing,” and a doctor says “go home,” count to 3, then remember the following:
“As the director of our vascular lab, I make sure that my techs are very well-versed in venous ultrasound,” says Paul Lucas, MD, surgeon with the Vascular Center and director of the Vascular Laboratory at Mercy Hospital in Baltimore.
“A true vascular lab will examine the entire leg in question, both above and below the knee.
“Some ultrasound departments will only rule out a DVT to the level of the popliteal vein, i.e.. to the knee.”
The popliteal vein is in the back of the knee, and a blood clot in this vessel can cause pain behind the knee.
The reason that some ultrasound departments run the transponder only up to the knee, says Dr. Lucas, “is the low embolization risk for a DVT in the tibial veins.”
Tibial refers to the larger of the two bones in the lower leg.
“If you need an ultrasound done to rule out a DVT, a certified/accredited vascular lab is the place to go.
“Vascular technologists only do vascular studies, whereas an ultrasound tech in some places will do all types of tests. Experience means a lot here.
“If however, a DVT is ‘missed.’ a repeat ultrasound exam may be warranted. If you suspect the DVT may be at the pelvic level or higher, a CT scan may be useful.
“It is possible to have a negative test and within days a repeat could be positive–and it really might not have been there on the first go-around.”
Read more about Staci Stringer.
 Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Shaynepplstockphoto
Causes of DVT in Absence of Risk Factors & Clotting Disorder
Find out what can possibly cause a DVT when there’s no risk factors and no clotting disorders.
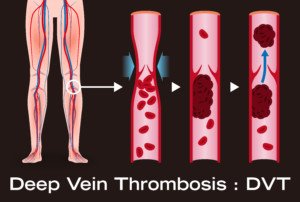
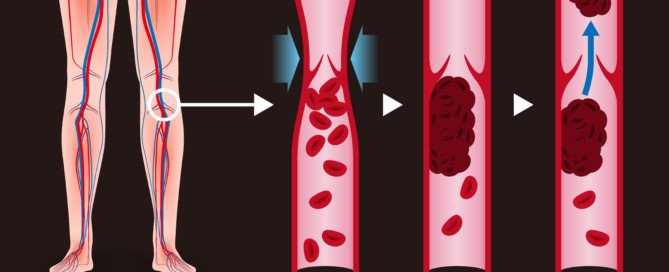
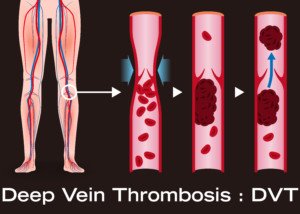
A DVT is a deep vein thrombosis: a blood clot in a vein deep in the body, usually in the leg, but sometimes also in the hip area.
In some cases of these blood clots, the patient seemingly did nothing to bring it on (such as being a smoker and sitting cramped in an airplane for several hours)
Additional DVT Risk Factors
Risk factors for a DVT are quite numerous and include prolonged immobility from any kind of traveling, joint replacement and abdominal surgery, birth control pills, hormone replacement surgery, obesity, lack of regular exercise, elderly age, pregnancy and dehydration.
And of course, blood clotting disorders raise the risk.
However, people have been known to get a DVT who have none of the risk factors and who test negative for clotting disorders, leaving the patient, who may even be a young lean gym rat who can’t sit still, baffled.
“In some cases the cause of a DVT is never found,” says Darren Klass, MD, clinical instructor of interventional radiology at the University of British Columbia and the Vancouver Coastal Health Association.
Dr. Klass explains, “In young healthy patients with no risk factors, mechanical compression of the left iliac vein by the right iliac artery in the pelvis may cause a spontaneous DVT. This entity is called May-Thurner syndrome.”
A person may never know they have May-Thurner syndrome until a deep vein thrombosis develops.
“A similar entity exists in the chest, where the subclavian vein (continuation of the vein from your arm) may become compressed by muscle or bone in the chest and cause a DVT,” says Dr. Klass. “This is called Paget-Schroetter syndrome.”
In this condition, repetitive and strenuous upper body activity (swimming, gymnastics, wrestling) is often linked to the deep vein thrombosis.
“Young patients with DVT with no risk factors will be investigated by their physician and these entities excluded,” continues Dr. Klass.
“Other more benign causes may simply be due to dehydration; patients who do not keep their fluid intake up may become dehydrated, which makes the blood more susceptible to clotting.
“In these cases often the dehydration is corrected long before the clot is discovered, and the cause is never found.
“These cases are very few and often a cause can be found after extensive investigation.”
 Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/metamorworks
sscpywrt26
Can a Blood Clot in the Leg Break off with Movement?
Learning you have a blood clot (DVT) in the leg is frightening.
And even more unsettling is the thought that movement can cause it to break off and travel to the lung and become a life-threatening pulmonary embolism.
If the broken-off portion of the clot is big enough, it can block both entryways for oxygen to the lungs, resulting in a quick death.
A person who’s been diagnosed with a DVT, or who believes they have one, may be afraid to be up and about walking.
Should movement be limited in someone diagnosed with a DVT?
If you’ve been diagnosed with a deep vein thrombosis, you might be thinking that you should remain as still as possible so that it doesn’t break off and travel to your lungs.
“No, most DVTs are fixed to the wall of the vein and it is highly unlikely to dislodge unless the vein is exposed to vigorous compression or unnatural force,” says Darren Klass, MD, clinical instructor of interventional radiology at the University of British Columbia and the Vancouver Coastal Health Association.
When these blood clots do dislodge, it’s usually something that happens spontaneously, with no apparent trigger.
This is why if you suspect a blood clot in a leg, you should immediately go to the nearest emergency room. Have someone drive you!
Treatment will begin immediately after diagnosis.
A DVT may cause redness, warmth, pain, cramping and/or swelling in a leg or behind the knee.
Immobility
Dr. Klass adds, “Conversely, not moving with a DVT may increase the risk of the clot getting larger due to the lack of blood flow from the legs.
“For this reason, pneumatic compression devices are often used during and/or after major surgery when a patient is not ambulant in order to stimulate venous flow in the legs.”
 Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals. Vancouver Coastal Health
Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals. Vancouver Coastal Health
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Casa nayafana
Top 4 Causes of Swollen Legs after Surgery
There are four main conditions that can cause legs to swell after surgery.
“There are a number of reasons for swollen legs post-operatively,” says Darren Klass, MD, clinical instructor of interventional radiology at the University of British Columbia and the Vancouver Coastal Health Association.
“The majority of the causes for this is fluid leaking into the soft tissues due to low protein in the blood, poor heart function, deep vein thrombosis, lack of mobility.”
Surgery that causes swollen legs need not involve the lower part of the body.
Coronary bypass surgery can leave both legs quite bloated.
DVT not the Leading Cause in Bilateral Swelling
“Unless the swelling is only on one side, the chance of this being a deep vein thrombosis is less than other causes,” says Dr. Klass.
“A deep vein thrombosis may not cause swelling of the leg initially and patients may be completely asymptomatic. It is only when the return of blood to the heart from the legs becomes compromised, do we see swelling from DVT.”
The swelling in the one leg may not be noticeable at first. But if the patient believes that the lower leg is looking just a little bit bigger than the other, they should point this out to their nurse and doctor.
If a DVT is suspected, a bedside ultrasound will be taken of the leg. It will immediately show if there is a blood clot.
If the result is negative, this is no reason to let your guard down. Do keep monitoring your legs, since a DVT may still develop.
Other Symptoms of DVT
Some hospitals will make sure that no matter what kind of surgery, the patient will postoperatively have on pneumatic compression devices for their liower legs.
These deliver intermittent compressing motions that help keep the blood from pooling.
To further help prevent a blood clot, some hospitals will mandate that all patients receive a daily injection of the blood thinner heparin.
Other signs of a deep vein thrombosis are reddish or purple or pale discoloration of the leg, tenderness, cramping or pain.
The pain may even persist even if you’re at rest or sitting. Pain can also occur in the pelvic area.
If both legs are swollen soon after surgery but feel fine and are not discolored, the patient should always be DVT-conscious.
 Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com/ pressfoto
Can a Pulmonary Embolism Be Diagnosed without Imaging?
A doctor may strongly suspect a pulmonary embolism based on a patient’s circumstances, such as suddenly struggling to breathe the day after hip replacement surgery, or sudden chest pain.
Even if the patient has other classic symptoms of a pulmonary embolus such as coughing up blood-tinged sputum, a doctor in good faith cannot just order administration of a clot busting drug unless the diagnosis is confirmed with imaging.
“The use of medication to bust up clots carries with it a risk of bleeding elsewhere in the body, as the medication stops blood from clotting,” says Darren Klass, MD, clinical instructor of interventional radiology at the University of British Columbia and the Vancouver Coastal Health Association.
“The physician responsible for administering the medication knows this and will ask specific questions to the patient to ensure it is safe.
“The patient must be closely monitored after this medication has been administered and therefore requires hospital admission.”
What leads to a pulmonary embolism?
Shutterstock/Designua
A pulmonary embolism is a blood clot in a lung (sometimes both; there can be multiple) that originally developed in a lower-extremity vein (lower leg to hip).
Such a blood clot is called a deep vein thrombosis (DVT) and are considered an emergency situation because it can dislodge at any time — and head straight for the lungs.
So to prevent a pulmonary embolus, one must take measures to lower their risk of a DVT.
Major Risk Factors for a DVT
- Obesity
- Smoking
- Birth control pills
- HRT therapy
- Excessive sitting throughout the day
- Sitting immobile in cramped quarters for hours without a break
- Long airplane rides
- Recent joint replacement or abdominal surgery
- Excessive bed rest
- Pregnancy
- Older age
A DVT is easily diagnosed with an ultrasound. A pulmonary embolism is diagnosed with a CT scan.
PE symptoms in combination with a positive result of a specific blood test will raise strong suspicion of this blood clot, but are not enough for an official diagnosis.
“Aside from this, PE can only be confidently diagnosed using medical imaging such as a CT scan,” says Dr. Klass.
“The clinical signs of pulmonary embolus are non-specific and cannot be confidently made without imaging.”
 Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
Dr. Klass specializes in interventional oncology, aortic intervention, PVD, venous disease and venous access. He has been inducted into The Leading Physicians of the World, published by the International Association of HealthCare Professionals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
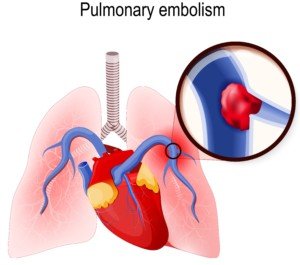
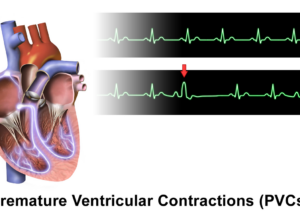
Thousands of PVCs, Normal Echo: Get EP Testing

A cardiologist says that if you have thousands of PVCs but a normal echo, you should get an EP test for a possible arrhythmia.
If you have PVCs (premature ventricular contractions), you may have developed an understanding along the way that these “skipped heartbeats” are benign as long as your echocardiogram is normal.
“Just because the echo is normal, that doesn’t mean that the person does not have bad coronary artery disease or a PVC focus that is causing all the PVCs,” says Dr. Sameer Sayeed, MD, a cardiologist at ColumbiaDoctors of Somers, NY.
Coronary artery disease can cause these “skipped heartbeats,” and an echocardiogram cannot detect or evaluate plaque buildup in arteries.
Other tests can evaluate for the existence of heart disease or assess heart disease risk: coronary calcium scoring, and the CT angiogram.
“If there are many thousands of PVCs, the patient’s coronary arteries should also be evaluated,” says Dr. Sayeed.
“If they are normal, then EP testing should be performed to determine if there is a PVC focus and if it should be ablated.”
An EP test is an electrophysiological exam of the heart to see if there is a rhythm disorder.
It takes about three hours and is administered by a cardiac electrophysiologist.
A doctor threads thin catheters with electrodes through veins into the heart, records signals and may try to trigger arrhythmias.
This helps diagnose and guide treatments like ablation or pacemaker placement, usually under sedation.
“When there are excessive PVCs, the heart is at risk for an arrhythmia or weakening of the muscle [cardiomyopathy] due to the excessive stimulation by the excess PVCs,” says Dr. Sayeed.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Why a PVC Can Cause Coughing

A cardiologist offers a simple explanation for why PVCs can cause some people to cough.
PVC stands for premature ventricular contraction, and some people can’t help but cough after having one of these episodes.
The coughing is usually just a single or double, and all it takes is just one PVC to trigger this.
“You may cough due to the phenomenon of post-PVC beat where the heart has a stronger contraction after a PVC, and this can irritate the diaphragm or phrenic nerve and cause cough,” explains Dr. Sameer Sayeed, MD, a cardiologist at ColumbiaDoctors of Somers, NY.
Source: BruceBlaus/CreativeCommons
The phrenic nerves (a pair) come down from the cervical area of the spinal cord and control breathing by innervating the diaphragm.
Both phrenic nerves pass very closely to the heart.
It’s also possible, though less likely than the explanation above, that the cough is triggered by sudden anxiety over feeling a “skipped heartbeat.”

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
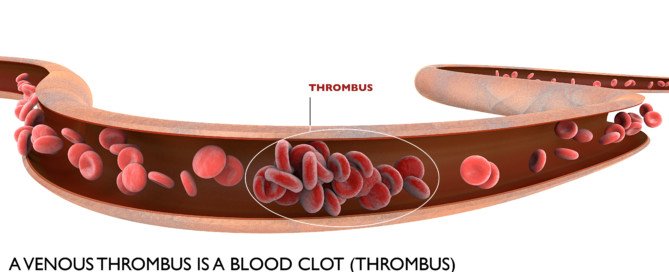
Can an Ultrasound Miss a DVT (Deep Vein Thrombosis) ?

It’s very true that an ultrasound can actually miss a DVT, but other tests are more definitive.
Staci Stringer’s DVT was missed by an ultrasound.
In September 2010, she experienced a deep vein thrombosis and pulmonary embolism.
When the DVT developed, Stringer was on birth control, but she also had lupus anticoagulant syndrome and rheumatoid/psoriatic arthritis.
Ultrasound Misses DVT
“It started as a pain in my leg, and after a week I went to the ER and had an ultrasound; they said it was nothing,” says Stringer on her site.
“The following Monday I was admitted to the ER with a PE,” which had caused chest pain.
“After a week or so the PE cut off blood flow to a portion of my lung which caused a pulmonary infarction.”
Another way of saying this is a “heart attack in the lung,” in that oxygen was cut off by the blood clots to the lung tissue, permanently damaging it.
Symptom Detail
“I started to feel the symptoms of a DVT in my right calf,” says Stringer’s account.
“It was swollen, extremely painful, hard to walk. I ignored the symptoms because I figured it was just arthritis pain.”
She continues: “I spoke with my general practitioner after a week and she told me to go to the ER for an ultrasound.”
Ultrasound is a standard diagnostic tool for DVTs.
“The technician thought he saw something but sent me home. I started to get a fever; my calf became so stiff I couldn’t walk.
“I walked up two flights of stairs to my apartment and was so out of breath I was grasping for air for 10 minutes.
“Next day I walked up the stairs to my office and I was so out of breath I fainted. I was admitted to the ER. After the CT scan they found a pulmonary embolism.”
How does an ultrasound miss a DVT?

Scientific Animations, Creative Commons/BY-SA/Attribution-ShareAlike 4.0 International
“I regularly order a venous Doppler to rule out DVT,” says Reena Patel, MD, a board certified family medicine physician who treats patients at Garnet Health Urgent Care in NY.
“An ultrasound uses sound waves and compression [of the blood vessel wall] to see blood flow in the veins of an extremity and can find an obstruction.
“There is room for error. Specifically, human error can result in a false negative, so it’s important to see the patient as a whole.”
A probe is used and if it slides off the vessel wall, a false-negative finding can result.
“It’s important in my experience, if suspicion is high and Doppler is negative, to have a backup plan,” says Dr. Patel.
“I may order a D-dimer. This is a sensitive test and can be very helpful to back up your diagnosis and warrant further imaging.
“I consider their history, the current symptoms and calculate their risk using reliable scoring such as the Wells’ score [a numerical value derived from the patient’s answers to numerous questions].”
Additionally, if you believe an ultrasound has missed a DVT, you should ask about a color flow venous duplex scan.
This should be of the vessels close to your pelvis as well as extending down to the foot.
If the D-dimer blood test is positive, the protocol is to have the patient undergo a chest CT scan.
The younger the patient, the more likely that a positive D-dimer means a blood clot, since old age can cause a false-positive with the D-dimer.
What caused Stringer’s DVT?
“The doctors weren’t sure if it was my birth control, my arthritis flare that caused the DVT,” says Stringer, “but I later found out I have lupus anticoagulant syndrome. I’m on warfarin for life.”




















 In addition to treating many chronic conditions,
In addition to treating many chronic conditions,