Can an X-Ray Show a Heart Attack?
If you go to the ER complaining of chest pain or shortness of breath/difficulty breathing, the doctor will want to order a chest X-ray.
You may wonder if this type of image can show a heart attack or reveal clogged arteries.
Perhaps you were relieved when, in the emergency room, your chest X-ray came back “clear” or “normal,” and maybe this made you think you didn’t have coronary arteries full of sludge.
What does a cardiologist have to say?
I asked Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY, if a chest X-ray can show if a patient had a heart attack.
Dr. Reynolds replies, “No. CXR could show congestive heart failure or an enlarged heart or a myriad of other problems, but it CANNOT show a heart attack.”
Chest pain and shortness of breath are common symptoms and can be caused by a number of other conditions that an X-ray can pick up, such as pneumonia and an aortic aneurysm.
Chest pain and shortness of breath can also be caused by conditions that an X-ray cannot detect, such as gastroesophageal reflux disease, costochondritis and extreme anxiety.
Why an X-ray Can’t Show a Heart Attack
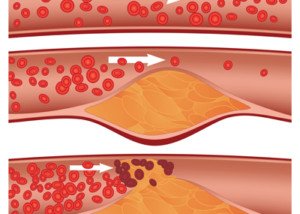
An X-ray cannot see the inside of the coronary arteries. It can certainly see the shape and size of the heart.
But this imaging tool cannot produce a picture of an obstruction inside a heart’s blood vessel.
Nor can it show the difference between cardiac tissue that’s normal and that which has been harmed by lack of oxygen.
When a patient presents to the ER with symptoms that a heart attack can cause, doctors always know that there are other conditions that can produce the same symptoms.
These conditions will show up on an X-ray. The test that is key to diagnosing a heart attack is a blood draw for an enzymatic protein called troponin.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Shortness of Breath, Chest Pain: What if Tests Are Negative?

Find out what you should do if ER testing finds nothing wrong with your heart despite chest pain and shortness of breath.
Chest pain is the No. 1 reason why people visit the emergency room. Shortness of breath is another leading reason for ER visits.
Typically, when a patient complains of chest pain with shortness of breath, they will be given a chest X ray, EKG and a blood test to track levels of an enzyme called troponin.
If troponin levels are increasing, this strongly suggests damage to the cardiac muscle: a heart attack, even a mild one.
The patient will be hooked up to a device that monitors heart rate, oxygen levels and blood pressure.
A doctor will listen with a stethoscope and feel the patient’s chest area. An EKG will be taken.
So imagine you have chest pain and trouble breathing, and all of these tests are normal.
What do you do next?

Shutterstock/ShotPrime Studio
“This totally depends on the patient – age, risk factors, how typical are the symptoms, physical exam, etc.,” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“Symptoms can be due to GI problems, anxiety, muscular strain, infection, etc.
“If cardiac disease is suspected, the patient usually gets referred for a stress test at some point.”
Warning: The above-named ER tests may come back normal, and you can still have dangerously blocked coronary arteries.
The troponin test detects if you’ve had, or are currently having, a heart attack.
It does NOT detect how much blockage is in your coronary arteries. Neither does a chest X-ray.
Though a doctor can tell a lot by listening with a stethoscope, this device cannot detect severely clogged coronary arteries.
An EKG test can be telling of heart disease, but some EKG readings can’t be read well (for possible severe heart disease) due to a “bundle branch block.”
If your ER tests are normal even though you have chest pain and shortness of breath, be very careful about what you decide to do next.
Your health history and absence or presence of risk factors for heart attack should weigh heavily into what should be done next.
Studies show that an MR angiogram, during the ER visit, is a reliable test for detecting severe heart disease in those with chest pain but with low risk factors for coronary artery disease.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Jamesboy Nuchaikong
Do Clear Carotid Arteries Mean Clear Coronary Vessels?

Just because your carotid arteries are “clean” doesn’t mean you don’t have severe blockages in your coronary vessels.
I was inspired to write this article after my father underwent an exam to see if there were blockages in his carotid arteries.
He underwent the exam twice because he had fallen at home but had no memory of the incident, nor was there a mechanical explanation for it.
The purpose of the carotid ultrasound was to see if there was enough plaque buildup in these arteries, which carry blood to the brain, to put my father at risk for a transient ischemic attack, which can cause a person to fall and sustain a concussion, which my father had.
A transient ischemic attack (TIA) is when a blood clot cuts off blood flow through a vessel in the brain.
These “mini strokes” can cause sudden-onset symptoms such as slurred speech, trouble forming words, facial paralysis or numbness (especially on one side), clumsiness, loss of balance, one-sided paralysis or weakness, severe headache and visual disturbances.
These symptoms may last only a few minutes or even less.
With my father, both vessels (located in the neck) were deemed normal; there was no concerning level of plaque buildup in his carotid arteries.
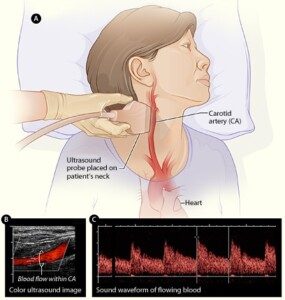
Carotid ultrasound. National Heart Lung and Blood Insitute
Can the carotids be clear in the presence of severe heart disease?
“Yes. Vascular disease tends to be system-wide — but just like most patients have more arthritis in one joint than another, most patients have an uneven distribution of vascular disease,” explains Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
If an ultrasound shows you have “clean” carotids, do NOT assume this means your coronary arteries are also clean or don’t have severe plaque buildup!
My father’s calcium score three years ago (from the initial date of this posting) came in at 1195!
A calcium score of over 450 means that a patient has a strong likelihood of severe coronary heart disease, especially if they have strong risk factors for such, which my father does.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/goodluz
sscpywrt26
Catheter Angiogram for Chest Pain but Low Heart Disease Risk?

Low risk for heart disease but chest pain? Which test is warranted: CT angiogram or catheter angiogram?
Find out what someone with low risk for heart disease should do if they have suspicious symptoms and want more than a stress test: cath angiogram or CAT scan?
Suppose you’re at low risk for heart disease (clogged arteries) in that you exercise, don’t smoke, aren’t overweight, have normal blood pressure, are not diabetic and eat mindfully, but…you’ve been having chest pains, especially upon exertion (or new-onset shortness of breath that’s out of proportion to level of activity).
Should you go straight to the cath lab? Or first undergo the non-invasive CT angiogram?
“You need to understand CT angio vs. cardiac cath angio before you throw up your hands in despair,” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“In summary – CT angio is really not much safer than a traditional cardiac cath.”
The CT angiogram involves significant radiation exposure, but the cath angiogram requires threading a catheter through the coronary arteries.
“And if significant disease is found, only the traditional cardiac cath allows the operator to proceed directly to stenting,” says Dr. Reynolds.
Placing a stent can be done while the catheter is already in place, if it’s determined that’s all the patient needs (i.e., bypass surgery not needed).
“CT angio for coronary arteries was the hot topic a few years ago, but has since fallen out of favor for several reasons,” continues Dr. Reynolds.
First of all, if one’s coronary calcium score is high enough, the calcified deposits will make it difficult to interpret the image from a CT angiogram.
“Patients with CAD almost always have significant calcium deposits. So CTA is really only useful in patients WITHOUT coronary disease, i.e., in healthy patients to rule out CAD.
“Here’s the downside of the CTA – CTA still requires injection of contrast dye and involves radiation,” says Dr. Reynolds.
“Therefore, the risk of an allergic reaction to the dye or risk to the kidneys from the dye in renal patients is the same whether you get a CTA or cath.
“The only advantage over a regular cardiac cath is that the test is performed using a peripheral IV rather than a central stick (usually into the femoral artery).”
Renal pertains to kidneys. The femoral artery is the main thigh artery.
“As I noted above, the other downside to CTA is that if disease is found, you can’t do anything about it. If a stent is needed, the patient then needs to have a cardiac cath to place the stent.”
When my mother was admitted to the hospital (from the ER) with chest pain, the cardiologist ordered a catheter angiogram; he bypassed the CT angiogram. Why?
Because my mother was at very high risk for severe heart disease or cardiac problems based on several factors: 1) Slightly elevated troponin level during ER visit, 2) Elderly age, 3) Abnormal echocardiogram, 4) High triglycerides.
Why waste time on a CTA with this type of patient?
It would only delay what the cardiologist probably was already anticipating: a need for a stent or even bypass surgery, plus expose her to unnecessary radiation and possible insult to kidneys from the contrast dye.
The catheter angiogram revealed “significant blockage” and about two hours later, she was undergoing quintuple bypass surgery!
“So here we go again – PRETEST PROBABLILITY OF DISEASE – if the doctor thinks a patient has normal coronaries but the patient has ongoing symptoms or is worried about coronary disease (CAD), a CTA can be done to rule out CAD,” explains Dr. Reynolds.
“This is being done more and more in the ER setting to expedite the evaluation process.” See link above in yellow highlight.
“However, if a patient is likely to have coronary disease (or the patient had a high CT calcium score), a cardiac cath is a better, more useful, more direct, and really safer approach to diagnosing and treating the disease.
“Current complication rates for cardiac cath, stent, etc., in a generally healthy patient are extremely low!
“Most complications occur in patients with unstable coronary disease and multiple medical comorbidities.”
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Pitchayaarch Photography
Normal Stress Test but a Massive Heart Attack the Next Day ?

A cardiologist explains why you can have a normal stress test one day and then a massive heart attack the next.
You’ve probably heard of instances in which a person had a normal stress test but then next day dropped dead of a massive heart attack. How can this be?
“We have more and more theories about how plaque develops within the coronary arteries,” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“We are starting to understand how soft plaque can rupture and lead to greater plaque formation.
“Sometimes these ruptures are minor and result in minor or no symptoms, but other times the rupture can be catastrophic, resulting in a totally occluded artery where before there had only been minor non-obstructive plaque.
“This catastrophic rupture often explains how a patient can have a normal stress test one day and a massive heart attack the next.”
To make this easier to understand, imagine a tube. The inner wall of the tube is only lightly covered with patches of sludge.
Water flows freely through the tube; there is no narrowing or restriction of the water flow.
One day, a piece of the sludge dislodges from the inner wall and travels down the tube, getting stuck at some point—stuck in a way that it blocks the flow of water.
That’s how a heart attack occurs when soft plaque ruptures in a coronary artery that, according to a stress test, has no restricted blood flow.
What a Stress Test Looks For
A stress test measures perfusion: blood flow through the coronary arteries.
A stress test does not measure amount of soft plaque, and it’s the soft plaque that can rupture (hard or calcified plaque can’t).
To kick back any soft plaque you may have in your coronary arteries, avoid processed food as much as possible.
So if you want a chicken, rice and broccoli dinner, make it the way someone in the year 1902 would have made it, rather than buying a frozen dinner.
Though it’s nice to know that one’s stress test was normal, there’s always that small chance that a massive heart attack is around the corner.
This is why it’s so important to keep on top of your heart health even if you don’t seem to have any risk factors or suspicious symptoms.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock
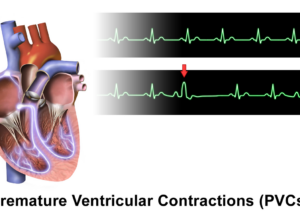
Is Exercise Safe if You Have PVCs 24/7?

A cardiologist addresses exercise safety in people with many PVCs, even nonstop.
Some people have premature ventricular contractions seemingly nonstop, thousands and thousands a day, and fear that exercise may not be safe for them.
“PVC’s had a bad reputation many years ago,” begins Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“When I was first in training, we were very aggressive in treating PVCs, especially in patients who had CAD, because the theory was that patients with PVCs were at high risk for cardiac arrest (V-fib or V-tach).”
CAD stands for coronary artery disease.
Dr. Reynolds continues, “In fact, we tried suppressing them with two infamous medications – Encainide and Fleciainide. Unfortunately, more patients died from the medications than from the PVCs.
“Since then, we’ve done a lot more research on PVCs and ventricular arrhythmias and risk of sudden cardiac death.
“We now use beta blockers, amiodarone, and ICDs (implantable defibrillators) in patients at high-risk for sudden death (low EF, prior cardiac arrest, etc.).”
EF stands for ejection fraction, the amount of blood that the heart beats with each pump. A low EF corresponds to weak pumping ability.
Exercise with PVCs Is Safe for Healthy Individuals
“PVCs in a healthy patient are rarely anything to worry about,” says Dr. Reynolds.
“We usually will do a holter, echo, and stress test to screen for more ominous arrhythmias.

Freepik.com
“Family history is also important to document, i.e., any family history of sudden death?
“Assuming everything checks out fine, then yes, you can exercise to your heart’s content (pun intended). Exercise actually suppresses benign PVCs.”
Exercise is safe for those with premature ventricular contractions who are healthy. This includes strength training.
Don’t let PVCs stop you from exercise if your cardiologist has given you the green light.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How Does Exercise Suppress PVCs?

A cardiologist explains how exercise suppresses or inhibits PVCs: premature ventricular contractions.
Though some people with PVCs wonder if it’s safe to exercise, it’s a well-documented fact that exercise suppresses PVCs.
In fact, many individuals who have frequent premature ventricular contractions report that exercise is a reliable, predictable way to stop them cold.
How does exercise stop or suppress premature ventricular contractions?
“Premature beats originate during the ‘resting’ phase of the cardiac cycle, i.e., the time when the myocardial electrical activity has reset itself and is waiting for the next electrical wave coming down from the atria -> through the AV node -> through the His bundles -> and then through the ventricular myocardium,” explains Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“With exercise, the heart rate increases which essentially shortens the ‘resting’ time and reduces the amount of time that PVCs can originate.
“Basically, the increased electrical activity of the faster beating heart overrides the aberrant beats in the ventricles.”
So even though you may have heard that the reason exercise seems to make PVCs go away is because PVCs can’t be felt as much when your heart rate is elevated and you’re huffing and puffing during physical activity, it’s a fact that working out actually inhibits PVCs.
And this process has nothing to do with the individual’s perception.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Deep Vein Thrombosis (DVT) Prevention: 7 Lifestyle Changes
Making lifestyle changes to help prevent a DVT is as easy as 1 through 7.
Deep vein thromboses are much more common than you think and are very dangerous, requiring immediate medical intervention.
“The problem isn’t the formation of the clot in the leg (although it is painful and causes significant morbidity such as swelling of the leg),” begins Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“The real risk is if the clot breaks off from its location in the leg and travels to distant parts of the body,” continues Dr. Besser.
“Once there, it can lodge in a blood vessel and cause that blood vessel to block. If there is no blood flow — that area of the body ‘starves from the lack of blood.
“The most common site for the clot to travel is the lungs (pulmonary embolus). That causes the lungs to work less efficiently — so less oxygen (a necessary substance for life) is absorbed.
“It is also possible for a small clot to pass through the lungs and lodge in a heart blood vessel which can cause a heart attack, or into the brain which can cause a stroke.”
You can now clearly see why making lifestyle changes to prevent a DVT is so crucial to one’s overall health regimen.
Even athletes can get a DVT. This disorder is not reserved just for the old and sick!
A DVT is a very preventable condition, even though a pulmonary embolism kills a person in the U.S. approximately every five minutes.
Big Steps Towards Preventing DVT
These ways to help prevent a DVT come from research that was presented at the Arteriosclerosis, Thrombosis and Vascular Biology 2013 Scientific Sessions.
- Exercise
- Don’t smoke
- Eat healthfully
- Avoid being overweight
- Control blood sugar level
- Control blood pressure
- Control cholesterol
These seven lifestyle factors go a long way in preventing DVT.
A study followed over 30,000 adults 45-plus for 4.6 years. Blood clot incidence was compared among three groups:
1) inadequate heart health
2) average heart health
3) optimal heart health.
Blood Clot Risk in the Study Subjects
- 44 percent lower in those with optimal heart health when compared to inadequate heart health.
- 38 percent lower in those with average heart health when compared to inadequate.
Out of the seven, what were the top two as far as greatest effect on lowering DVT risk? Exercise and weight control.

Shutterstock/wavebreakmedia
So now you have even more motivation than ever to lose body fat and stay on an exercise program. Exercise should include strength training.
And please, don’t assume you have an automatic built-in exercise regimen just because you do housework or have a staircase in the home.
A deep vein thrombosis is a lot more powerful than household chores!
Do your part in helping prevent the development of a DVT by following the seven lifestyle changes here.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2013/05/130502185419.htm
ABDOMINAL AORTIC ANEURYSM: Surgery, Drugs, Watchful Waiting
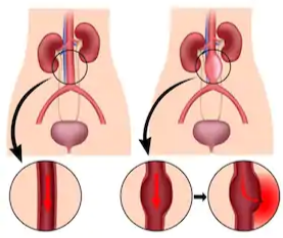
An abdominal aortic aneurysm is a very serious condition, but not all cases require treatment.
The aorta is the largest blood vessel in the body.
It comes out of the heart and travels all the way down the abdomen, where it branches off to feed blood to the lower extremities as well as organs, especially the liver and kidneys.
Usually, a bulging section of this great vessel is discovered by accident, when the patient is imaged for an unrelated cause.
For example, he might undergo an X-ray covering the abdominal region for an unrelated issue, and the ballooned portion of the aorta is picked up on the study.
Treatment for an Abdominal Aortic Aneurysm
If the vessel is only mildly dilated, the treatment will be ongoing surveillance via imaging studies to track the growth of the aneurysm.
“If you have been diagnosed with an aortic aneurysm and have been told to simply observe symptoms, know what symptoms you should be looking for,” says Walter Gaman, MD, FABFM, board certified in family medicine and the author of several award-winning books including “Age to Perfection: How to Thrive to 100, Happy, Healthy, and Wise.”
“This will allow you to recognize a serious change in your condition.”
The symptoms may be abdominal pain, back pain, a bulge in the lower abdomen and/or feeling a throbbing pulse in the lower abdomen (without actually touching the area with your fingertips).
“Also, share these symptoms with your family members so they will know how to react in case of an emergency,” says Dr. Gaman.
If the aneurysm ruptures, the pain will be sudden and agonizing, capable of bringing the person to the floor.
“Alerting medical personnel early will help your chances of survival. The most common symptom is intense pain in your abdomen, side, or back.”
The excruciating pain of a ruptured abdominal aortic aneurysm may be the person’s first symptom.
The mortality rate is very high due to the rapid internal hemorrhaging. Below is a graphic image of an actual AAA.

Hertzer NR, CC
Risk Factors
- Male gender
- Over age 70
- Smoking
- High blood pressure
- Family history of AAA
Ongoing Surveillance
“Aortic aneurysms should be monitored yearly,” says Dr. Gaman. “If they get to or above five to six cm in diameter, surgical intervention may be necessary.”
Sometimes, though, when an abdominal aortic aneurysm is discovered, it’s already at a life-threatening size, and the diseased portion must be repaired asap.
The repair may be done invasively by opening up the abdomen, or, it may be done endovascularly, which means a shorter recovery time and lower risks of complications.

Dr. Gaman is with Executive Medicine of Texas and is with the Staying Young Radio Show 2.0 podcast.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Alila Medical Media
Peripheral Neuropathy Misdiagnosis: Doctors Miss Disease
Just because doctors haven’t mentioned peripheral neuropathy as the cause of your pain, doesn’t mean you can’t have it.
“Peripheral neuropathy” means disease of the nerves of the peripheral nervous system, and I know at least one person who’s been recently diagnosed with this — after it was missed for the past four years by a steady stream of doctors: my father.
For about four years he’d been complaining of pain in his legs, and several doctors attributed this to problems with his low back, including spinal stenosis. Two endoscopic back surgeries didn’t help.
Another doctor said it was from osteoarthritis of the hip and recommended a hip replacement, which my father had; it did no good.
He’s had three knee replacement surgeries by two orthopedic surgeons who both said that the leg pain was caused by osteoarthritis in his knees.
The second surgeon, who did the third knee surgery (a revision) said that the pain could very well be from a failed knee replacement.
What seems to make it easy for doctors to miss peripheral neuropathy is when the patient actually has these other conditions, which are easily proven with X-rays and MRIs.
My father has had more than one primary care physician over this time period, who named back and knee problems, as well as old age, as probable causes of the leg pain.
Other proposed explanations for the leg pain was a knee infection, and allergic reaction to the knee replacement device.
Early on, an adverse side effect to my father’s use of a statin drug was suspected, but ruled out after he went off the statin but the leg pain continued.
Strangely, none of these many doctors came up with, “You know, this very well could be peripheral neuropathy. Let’s aggressively pursue this possibility.”
Peripheral Neuropathy Doesn’t Necessarily Work Alone
If you have degenerated knees or lumbar discs, this doesn’t mean you can’t also have peripheral neuropathy adding to your lower body pain, burning and tingling.
Peripheral neuropathy is associated with diabetes; diabetes is the most common cause.
A doctor may rule out peripheral neuropathy if you don’t have diabetes (my father doesn’t), and especially if you have other “differentials” that can explain the leg pain, such as degeneration of the lumbar spine as shown on imaging tests.
How did my father finally get diagnosed with peripheral neuropathy?
His assortment of doctors would have continued to miss this had he himself not decided one day to review his medical records over the past four years.
He’d had an EMG about three years ago and the doctor said he had “nerve damage.” However, that doctor, plus his primary care doctor at the time, didn’t further pursue this “nerve damage,” and thus, my father had thought nothing of it.
My father found the words “peripheral neuropathy” in the paper work as a diagnosis, and was floored that nothing ever came of this; no further workups or recommended drugs.
He immediately contacted his newest PCP, who in turn ordered blood tests to rule everything else out.
Within 24 hours of the blood tests, my father was prescribed Nortriptyline, a tricyclic antidepressant that’s also used to suppress the pain of peripheral neuropathy.
At the time of this writing, he has not yet gotten the prescription because it was ordered late Friday afternoon.
Why, after four years, did so many doctors not think of peripheral neuropathy?
And why didn’t the EMG neurologist pursue it? It’s because sometimes, the patient knows more than their physician.