Can Sinus Problems Cause Pain in the Neck?

Sinus issues may cause neck pain … but only under a specific circumstance, says an ENT doctor.
*****
Neck discomfort can have numerous causes, including sleep position, a compressed nerve and even heart trouble.
Since the nasal passageways are rather near the neck, you might be wondering if there’s any chance that a problem in your nose could be related to pain in your neck region.
The answer is yes — but only under a specific circumstance.
“Neck pain cannot be from sinus problems unless you additionally have sinus symptoms,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology (ear, nose and throat).
What are the typical sinus related symptoms?
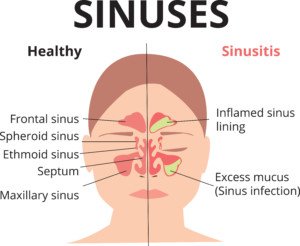
Shutterstock/Ekaterina Siubarova
Sinus symptoms classically consist of a headache (that often feels like a stress or tension type of headache), pressure or aching behind the eyes or across the forehead, nasal congestion, and, says Dr. Silvers, facial pressure (a common symptom of sinus problems) or discomfort in the upper teeth.
“You would not have isolated neck pain with the sinuses as a cause with no other symptoms,” says Dr. Silvers.
So if your only symptom is an ache in your neck, then you need to keep seeking out the cause if it persists despite, for instance, changing pillows or how you sit before the computer, or with a warm compress to help heal strained muscles.
Other Sources of Neck Pain
“Neck pain can be muscle, bone or nerve related,” adds Dr. Silvers. “Our necks are very sensitive and can be sore with stress, sleeping funny and even holding our heads in an awkward position after a while.
“Anything that causes chronic pain elsewhere in the body can also manifest itself in the neck based on how we carry ourselves and how we sleep.”
A new exercise can cause isolated neck pain, such as tilting the head upward during the exercise, which pulls at the frontal neck muscles.
A muscle spasm or a persistent ache from the exercise can result later on in the day or even the day after.
Persistent neck pain with no explainable cause (such as from prolonged bending of your head backwards from belaying your climbing partner) warrants a visit with a doctor and likely an MRI, as the pain can be caused by a pinched nerve or other problem.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sneezing, Sniffling after Exercise: Causes & Solutions

Find out what an ear, nose and throat physician says about sniffling and sneezing after exercise.
Do you find you must sneeze and/or have the sniffles following exercise? Even indoors?
This may occur soon after you completed your training on a stationary bike, elliptical machine, revolving staircase or treadmill.
Or, the sniffling and/or sneezing may begin starting up right after your group fitness class, martial arts class or staircase workout.
And you know it can’t be allergies if this happens indoors.
“Vasomotor rhinitis is the medical term for a runny nose,” begins Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology (ear, nose and throat).
“Triggers in younger people can be eating spicy food, walking in cold weather and exercise. Runny nose causes sniffling and can be more constant with age.”
Allergic rhinitis is another term; does your sneezing or sniffling occur after only outdoor exercise?
Pollens in the air or even environmental pollutants can be causes.
Do the annoying symptoms occur most after you’ve hiked among wildflowers?
“An anticholinergic medication like Ipatropium bromide can dry up a runny nose and be used on an as-needed basis,” says Dr. Silvers. “This is a prescription from your physician.”
What about a runny nose during aerobic activity?
In my case, it kept happening when I was inline skating. The solution is to treat the symptom.
Every so often on the trail there was a trash can off to the side.
I’d have tissue paper in my fanny pack, and when it was time to give my nose a good blow, I simply cruised over to a trash can, blew, then deposited the used tissue paper into the can.
Then I’d take off for another round of inline skating.
It’s possible that pollen contributed to the runny nose., especially since once I stopped this fun form of aerobic exercise, the runny nose ceased.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Vladimir Gjorgiev
How Soon after Total Hip Replacement Can you Cross Legs?
An orthopedic surgeon provides guidelines to crossing legs after total hip replacement surgery.
For many, crossing the legs is second nature.
The tendency to want to do this will be strong even after a cross-legging person undergoes a total hip replacement surgery.
If this is a strong habit for you, and you plan on having a total hip replacement — or have just had one — you’re going to have to give up this habit for a while.
How Long to Refrain from Crossing Legs After a THR
“Some surgeons will limit leg crossing after total hip replacement for six weeks,” says Marc W. Hungerford, MD, Chief of Orthopedics at Mercy Medical Center and Director of Joint Replacement and Reconstruction at Mercy.
Six weeks — yes. That may seem like along time to abandon a habitual seating position. But you really should do this.
Dr. Hungerford explains, “Bringing the hip across the body midline and rotating it could cause the hip to dislocate.
“The restriction is usually in place for six weeks until the tissues around the hip have healed.”
This guideline applies whether a person has an elective THR due to degenerative joint disease (osteoarthritis in the hip) or due to a fractured hip from an accident.
And it doesn’t matter if you’re a man or a woman. The new hip needs a chance to settle in.
What about crossing the legs after a total knee replacement?
“There is usually no restriction to crossing the legs after TKR,” says Dr. Hungerford.
However, after a TKR, you should not do deep squats or sit on your heels (common positions for gardening). And this rule is in place for all time following the surgery.
The need for elective total hip (and knee) surgery is caused by the reduction of cartilage between the bones.
In some cases there is no cartilage; the X-ray shows bone-on-bone contact. Crossing one’s legs does not cause the hip cartilage to wear down.
 Dr. Hungerford was the first orthopedic surgeon in Maryland to perform MAKOplasty, a minimally invasive partial knee procedure powered by the RIO® Robotic Arm Technology.
Dr. Hungerford was the first orthopedic surgeon in Maryland to perform MAKOplasty, a minimally invasive partial knee procedure powered by the RIO® Robotic Arm Technology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik
Why Swelling of Surgical Leg (TKR) Goes Down Overnight

An orthopedic surgeon explains why swelling of the surgical leg (total knee replacement) goes down overnight and then seemingly balloons up after awakening.
Following a total knee replacement, the patient may notice that the initial swelling subsides as the hours after the surgery pass.
But then, come next morning, the leg looks bigger than ever, all puffed up.
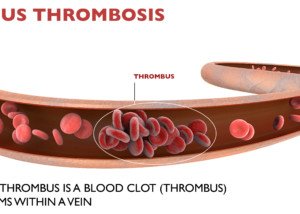
The patient may then be alarmed over the possibility of a blood clot (deep vein thrombosis).
A DVT is an alarming problem because at any moment, a piece of the blood clot (or the whole thing) could dislodge and in seconds get into the lungs and cause a life threatening pulmonary embolus.
Swelling after a Total Knee Replacement
“Swelling is a function of circulation and fluid pressure,” begins Marc W. Hungerford, MD, Chief of Orthopedics at Mercy Medical Center and Director of Joint Replacement and Reconstruction at Mercy.
“After a total knee replacement the circulation to the knee is increased because of the body’s healing response.
“When you are standing or sitting during the day, the leg is in a dependent position and the pressure in the blood vessels is increased.
“When sleeping at night, the leg is at the same level relative to the rest of the body and the pressure decreases. This allows the pressure and swelling to go down.”
But then once you’re awake — and up and about — you may see that the leg appears to be swelling more.
Following TKR, the patient is urged to get up and about as soon as possible, not only to help prevent a blood clot, but to hastily get the joint acquainted with its new device. The sooner the better.
Nurses will check both legs of the patient throughout the day to make sure that the swelling is par for the course rather than suspicious for a DVT.
Over 600,000 total knee replacements are performed in the United States every year!
Each year, over 600,000 total knee replacement surgeries are performed in the U.S.
The knee joint is the most unstable joint in the human body.
Adults of any age can be affected by osteoarthritis, though it’s most common in older people.
 Dr. Hungerford was the first orthopedic surgeon in Maryland to perform MAKOplasty, a minimally invasive partial knee procedure powered by the RIO® Robotic Arm Technology.
Dr. Hungerford was the first orthopedic surgeon in Maryland to perform MAKOplasty, a minimally invasive partial knee procedure powered by the RIO® Robotic Arm Technology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Dave Haygarth/CreativeCommons
Vomiting During or After Exercise: Causes & Solutions

A doctor offers a very interesting cause of vomiting during or after exercise.
“That can happen when a person is very toxic, so when the circulation improves, then the lymphatics start moving and dumping toxins,” explains Carolyn Dean, MD, ND – Medical Advisory Board Member of the non-profit Nutritional Magnesium Association at nutritionalmagnesium.org.
“Vomiting is one way for the body to eliminate toxins.”
When I was a personal trainer, several of my clients upchucked a little towards the end of their workout session.
They were not what I’d call “physicalky fit” individuals. I worked them pretty hard, but kept a close watch on them to make sure they weren’t feeling sick.
The clients were beat towards the end of the exercise session, and only then did the vomit come.
My conclusion was that they hadn’t nourished and hydrated themselves well prior in the day.
In fact, one of these clients had nothing to eat all day prior to her evening workout with me.
Others reported having hardly eaten all day. This, combined with being out of shape or not being used to a strenuous workout, caused nausea, leading to vomiting.
A poorly conditioned person on the SAD (standard American diet) has a more toxic body than a physically fit person who’s been eating healthfully.
Additional Causes of Vomiting During or Shortly After Exercise

Shutterstock/MikeSaran
Motion sickness can lead to upchucking, such as the motion experienced when twirling around in a dance-based group fitness class, or even from some of the pivoting motions of a step aerobics class.
GERD (gastroesophageal reflux disease) can cause a queasy feeling from the acid jostling around as it refluxes back up the stomach and food pipe.
Exercise decreases blood flow to the cells of the digestive tract. A de-conditioned person is less able to tolerate this, and nausea can result.
Quite simply, improving one’s physical condition will resolve this issue.
There are those who can strenuously exercise on an empty stomach (morning workout) with little hydration, and not feel the least bit queasy.
Ending a grueling exercise session abruptly. A warm-down is important.
Then again, vomiting after abruptly ending a hard-hitting exercise session goes back to lack of conditioning.
A woman who doesn’t know she’s pregnant and exercises hard can also find herself vomiting at some point.
To avoid vomiting during or after exercise:
1) Take time to warm up; don’t dive into the workout full-force.
2) Par back on intensity to give your body a chance to get fitter.
3) Have some fruit or juice before the workout.
4) Have water before, and every 15 minutes, during the exercise.
5) Stick to a plant-based diet with strict limits on processed foods.

Dr. Dean, in practice for 35+ years and author of “The Magnesium Miracle,” is also a naturopath, nutritionist, herbalist, acupuncturist, lecturer and consultant.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Burning Lungs, Coughing after Hard Running: Benign Causes

There are several benign causes of burning lungs & coughing after hard running, and what’s “hard” is subjective.
“Burning in the lungs and coughing after hard running are likely due to magnesium deficiency,” says Carolyn Dean, MD, ND – Medical Advisory Board Member of the non-profit Nutritional Magnesium Association at nutritionalmagnesium.org.
“Magnesium makes muscles work properly, allowing calcium to cause muscle contraction and then pushing calcium out of the muscle cells to allow the relaxation phase.
“When there is a lack of magnesium, muscle cells in the bronchial tubes can go into spasm, tighten up and cause wheezing and burning and coughing.”
Try a magnesium citrate supplement in powder form. Follow directions; usually it’s one teaspoon twice per day.
Other Benign Causes of a Burning Sensation in the Lungs (with or without) a Cough after Running
Exercise-induced acid reflux. Wait 60-90 minutes after eating (even if it’s just an apple) before running and see what happens.
Exercise-induced asthma. This too is a possibility.
Being out of shape. Being de-conditioned can result in blood vessel constriction and excess mucus after you stop running, causing a burning feeling in the lungs and possibly a cough.
Solutions
See a physician if you suspect exercise-induced asthma. As for reflux, this may diminish over time as your body gets more physically fit.
In general, poorly conditioned lungs will “burn” after you do a level of running that you’re not used to.
This situation is quite common. And see how a magnesium supplement works.
Two of my personal-training clients, men in their 20s, experienced this lung burn after they worked out hard (high intensity interval training) on the elliptical machine, something they hadn’t done before.
Though this isn’t the same as running, it was still hard work that their lungs and GI tract were not used to.

Dr. Dean, in practice for 35+ years and author of “The Magnesium Miracle,” is also a naturopath, nutritionist, herbalist, acupuncturist, lecturer and consultant.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Tiny White Bump Inside Lower Eyelid, Painless
I asked my dermatologist what the very tiny white bump on the inside of my lower eyelid might be.
A “tiny white bump” on the inner lower eyelid can be a rather broad description.
But in my case, the very small white bump was about one and a half or so millimeters. It was painless, didn’t itch; I didn’t feel it in any way.
I noticed it when I one day slightly pulled down my lower eyelid to see if anything was where my lower eyelid meets the white of the eye, because there was an irritant in my eye.
I figured there was an eyelash there. That’s when I noticed a very small white bump, almost like a nodule.
For many months I’d periodically check it to see if it was changing in any way, and it always looked the same. This was reassuring.
Dermatologist
Finally when I saw my dermatologist for a routine skin check, I asked her what it was. She didn’t hesitate to say it was a cyst.
If you have any kind of white bump in your eyelid that’s causing symptoms, a scratchy feeling, swelling or is evolving especially, do not hesitate to see a dermatologist.
A dermatologist is more qualified to diagnose this than is an ophthalmologist — because it involves the skin, not the actual eyeball.
Now think about that for a moment. The eyelid is not part of the eye; it’s part of the skin. This includes the inner portion of it.
Yes, it’s right up against the eye, but that doesn’t change the fact that it is SKIN tissue. See a dermatologist.
“Diagnostically speaking, tiny white bumps in the lower eyelid are most likely to be either a hordeolum (stye) or chalazion,” says Tejas Patel, MD, a board certified dermatologist with AdvantageCare Physicians in New York.
“A chalazion is a noninfectious obstruction of the oil glands of the eyelids,” continues Dr. Patel.
“The benign cysts usually develop after abnormally thick oil gland secretions due to gland obstruction.
“A chalazion is usually not painful and usually develops further back on the eyelid than a stye.”
My cyst eventually disappeared on its own.
“A hordeolum (stye) is usually a pyogenic infection, most prevalently caused by staphylococcus,” says Dr. Patel.
“These benign cysts usually result from obstruction and infection of an eyelash follicle and adjacent gland. Styes are usually very painful.”
If you have a stye, applying a warm, moist compress for about 10-15 minutes several times a day can help loosen it, promoting drainage.
Gently massage the area with clean hands to encourage drainage. If there’s no improvement, consult with your dermatologist; don’t squeeze the stye.
A tiny white bump inside the lower eyelid is not likely to be something worrisome, but it’s always reassuring to get a benign diagnosis from your doctor.
 Dr. Patel treats all skin types and welcomes the most challenging skin problems. Dr. Patel specializes in both medical and cosmetic dermatology, and treats patients of all ages.
Dr. Patel treats all skin types and welcomes the most challenging skin problems. Dr. Patel specializes in both medical and cosmetic dermatology, and treats patients of all ages.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Why So Many Pulmonary Embolisms in Hospitals Are Fatal
Many pulmonary embolisms in hospital settings cause sudden death without symptoms, but many people die even when there are warning signs.
You may be thinking that it takes about four minutes for irreversible brain damage to occur when a patient has been deprived of oxygen (airflow blocked by a massive pulmonary embolism).
You may then be thinking that between symptom onset and death, medical personnel have four minutes to re-establish airflow.
However, people in hospitals have died from a pulmonary embolus even when there was more “brain time” involved.
In that case, the patient was still conscious and breathing (albeit very labored) after initial PE symptom onset.
“Massive PEs or saddle embolisms have a high risk for being fatal in any setting,” says Paul Lucas, MD, a surgeon with the Vascular Center and director of the Vascular Laboratory at Mercy Hospital in Baltimore.
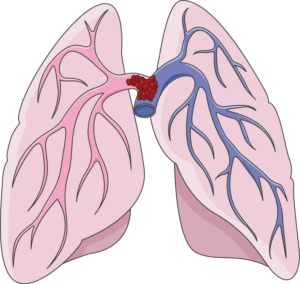
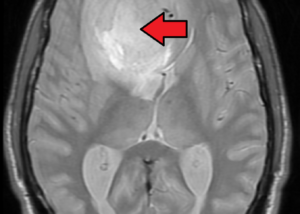
A “saddle” pulmonary embolism, plugging up the point at which the pulmonary artery branches off into each lung. Death can occur suddenly. Laboratoires Servier, CC BY-SA 3.0 /creativecommons.org/Wikimedia Commons
“Events occurring in a hospital, or at any site for that matter, require a trigger of a sequence of events to occur …. time of event to intervention,” continues Dr. Lucas.
“Although we would all like this to be instantaneous, it does take time. Every effort is made in these emergencies to expedite this.”
Treatment of Pulmonary Embolus Has Risks
“Keep in mind, you have to have a strong suspicion/diagnosis for this entity to just administer “clot busters,” as other things can have similar presenting symptoms,” says Dr. Lucas.
“You certainly don’t want to give ‘clot busters’ to someone whose symptoms are from that of bleeding.”
Here is what Steven Elias, MD, a vein specialist with Englewood Health in NJ, says:
“Before starting any therapy [i.e., blood thinners) that has significant risk such as intracranial bleeding (bleeding in the brain), most MDs would like a definitive diagnosis.
“If a patient survives a ‘massive PE’ and doesn’t immediately die, there is usually time for a CT scan which takes about 1-2 minutes.”
 Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can You Get Deep Vein Thrombosis DURING Air Travel?
Two doctors weigh in on getting a DVT while on the airplane.
Perhaps you’ve heard of cases in which a person seemingly developed a DVT at some point after landing from air travel.
There are cases in which the patient becomes aware of leg pain and swelling while in a hotel or shortly after arriving back home.
“Yes, you can develop DVT during air travel, or any travel for that matter that requires long periods of immobility,” says Paul Lucas, MD, a surgeon with the Vascular Center and director of the Vascular Laboratory at Mercy Hospital in Baltimore.
DVT Risk Factors Aboard a Plane
“The risk increases with the length of flight,” says Steven Elias, MD, a vein specialist with Englewood Health in NJ.
A very long trip in an airplane will encourage sleeping — which means very inert legs in a cramped space, unable to move about as they normally would when a person sleeps in a bed.
Dr. Elias adds, “The nature of air travel: immobility and dehydration secondary to cabin air low humidity add to the risk. DVT risk goes up significantly in flights longer than four to six hours.”
Shortest amount of time between takeoff of the airplane and DVT formation?
Dr. Lucas explains, “As far as the shortest amount of time to develop a DVT on the flight, that’s hard to pin down, and the reality is, it could be at any moment, but increased with the longer periods of immobility.
“Keep in mind though, the incidence of in-flight DVT is pretty low overall.”
Tips for avoiding a deep vein thrombosis while flying:
Stay hydrated, avoid liquor, get up every hour — no longer — and walk up and down the aisle
And, while seated you can regularly flex your feet up and down, which will stimulate blood flow in the calves. See the illustration below.
 Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
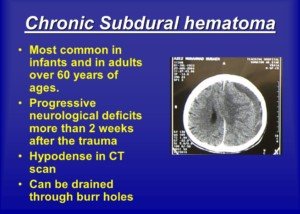
How Common Is Headache in Chronic Subdural Hematoma?

Headache incidence varies depending on the age of the patient with chronic subdural hematoma.
A report in the Postgraduate Medical Journal states that the incidence of headache, as a symptom of chronic subdural hematoma, varies among different studies. The variance range is 14 percent to 80 percent.
The report points out that headache is less common a symptom in the elderly with chronic subdural hematoma than in younger patients. There’s a few reasons for this.
As the brain ages, it shrinks.
This is called age related brain atrophy. A shrunken brain means more intracranial space or room for the leaking blood to take up before pressure builds up on the brain (causing headache).
In a young person, there isn’t as much room for the leaking blood to fill, making headaches more likely as a first symptom.
This doesn’t mean elderly patients can’t get headaches from a chronic subdural hematoma.
In fact, my elderly mother’s first symptom complaint was of a horrible headache—later that day she was diagnosed with chronic subdural hematoma (from a fall six weeks prior in which she hit her head).
The Postgraduate Medical Journal then notes that the second reason is that in the elderly, there’s an “earlier onset of confusion,” and this “attracts medical attention before the development of headache” in elderly patients.