How High Must ALT & AST Be for Liver Disease?

Here’s what a liver doctor says about the ALT and AST blood tests.
The cut-off point for whether or not an ALT or AST value should be of concern, can be confusing, especially since values can vary from one lab to the next.
“There is no definite value for this,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“For example, patients with hepatitis C can have normal or near normal liver enzyme values and still have significant liver disease.
“In short, just because your liver enzymes are normal, does not mean that everything is necessarily normal.”
The AST and ALT number are not the be-all, end-all.
Dr. Blume explains “that you cannot interpret an isolated laboratory value or group of laboratory values as numbers that tell you something.
” You need to interpret these numbers in the context of why they were ordered in the first place, and what question they were supposed to answer.”
Dr. Blume adds: “It is important to remember that we treat people, not laboratory test numbers, so one needs to answer, what that number means in that particular person.”
Symptoms of Liver Disease
• Jaundice: the skin has a yellowish tinge. This may also be present in the eyes and inner lips.
• Abdominal swelling or pain (fluid buildup)
• Swelling in the legs and ankles caused by fluid buildup as well
• Itchy skin with no apparent cause
• Urine that’s the color of tea or cola
• Pale bowel movements
• Blood in the BMs or BMs that have what looks like gooey tar in them (old blood)
• Unexplained fatigue
• Nausea or vomiting
• Loss of appetite
• Tendency to bruise easily
Risk Factors for Liver Disease
• Heavy drinking
• Diabetes
• Obesity
• Drug use with shared needles
• Unprotected sex
• Exposure to toxic chemicals like insecticides and aerosol sprays.
• Tattoos or body piercings
Problems with the liver can also be caused by heart failure.
The ALT and AST values won’t necessarily be as high as expected for this.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/goodluz
Joint Pain from Fibromyalgia vs. Rheumatoid Arthritis
Here is what a doctor says about the difference between fibromyalgia joint pain and that from rheumatoid arthritis.
“With rheumatoid arthritis the pain is localized predominantly in the hands as opposed to the larger joints being more affected in fibromyalgia,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“In addition, rheumatoid arthritis has red [and tender feeling] swollen joints, where there is no swelling or inflammation in fibromyalgia,” adds Dr. Teitelbaum.
The hands (or feet) of someone with rheumatoid arthritis have a distinct appearance that certainly does not look painless. Fibromyalgia does not alter the appearance of any joints.
Rheumatoid arthritis can affect the knees, hips and shoulders when it progresses, but not as commonly as does fibromyalgia.
Dr. Teitelbaum adds, “Morning stiffness is worse with rheumatoid arthritis than fibromyalgia. Fibromyalgia pain intensity is flared by cold weather.”
The stiffness of rheumatoid arthritis is made worse also by extended periods of inactivity such as sitting in front of a TV.
Just what does the pain of fibro feel like?
“It feels predominantly like widespread achiness, but in time progresses to include neuropathic sharp burning pains, and sometimes even the skin sensitivity to touch,” says Dr. Teitelbaum.
This includes odd sensations involving the scalp.
Can it feel anything like “sore” muscles that one experiences after a hard gym workout?
“It actually can feel like that, but amplified many-fold, all over your body, and without going away.”
Another difference in the way rheumatoid arthritis makes the body feel when compared to fibromyalgia is that with the former condition, the patient may have a fever or feel feverish.
Both fibromyalgia and rheumatoid arthritis can make the patient feel fatigued.
A worst case scenario is when a person has both of these conditions.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Aaron Amat
Can Joint Pain Be the Only Symptom of Fibromyalgia?
Fibromyalgia is linked to many symptoms including joint pain, but can this symptom be the only presenting feature of this condition?
“It can present simply with joint pain, and but the way to distinguish it from arthritis is that it is both widespread, does not have red swollen joints, and is associated with insomnia,” explains Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
Symptom Specific Features
“The pain will tend to be more aching around the joints, and is actually coming from the tight muscles where they attach at the joints,” says Dr. Teitelbaum.
“In fact most people with fibromyalgia mistakenly think that they also have arthritis.”
If all you have is joint pain, and it comes and goes, this does not mean you have fibromyalgia or a degenerative form of arthritis.
You may have been diagnosed with fibromyalgia when, in fact, the cause of your joint pain is inflammatory bowel disease.
Have you been diagnosed with Crohn’s disease, ulcerative colitis or the much more benign microscopic colitis?
All three of these inflammatory bowel diseases can cause joint aches or what might be described as pain.
When digestive issues cause aching joints, this is called enteropathic arthralgia.
However, when a patient presents to their primary care doctor with complaints of joint pain, the doctor’s first thought isn’t going to be colitis.
A person with joint pain may have both an inflammatory bowel disease and fibromyalgia.
It may not be possible to determine which of the disorders is causing the discomfort in the joints.
Making the overall picture more vexing is that the cause of fibromyalgia joint pain — though speculated upon by many — is not truly known. A few theories:
Central Sensitization: This theory suggests that fibromyalgia involves an abnormal processing of pain signals in the central nervous system.
The brain and spinal cord may become more sensitive to pain stimuli, leading to heightened pain perception.
Neurotransmitter Imbalances: Imbalances in neurotransmitters such as serotonin, norepinephrine, and dopamine may play a role.
These chemicals are involved in regulating mood and pain perception.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/fizkes
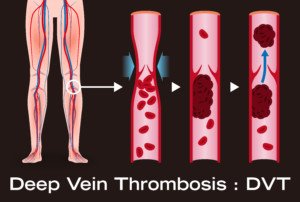
Duodenal Cancer Tips for Treatment, Chemotherapy
A woman who was personally touched by duodenal cancer offers valuable tips for those going through treatment.
Unless you have a known “condition or illness” that runs in your family, most do not go for an endoscopy or any scope for that matter.
That is changing with each milestone; a test (endoscope) should be done just like annual mammograms, and starting at age 35, for sure at age 40.
I’m not a doctor, but I’m writing from experience and knowledge I’ve gained over the years from collecting information about a rare cancer: duodenal cancer.
When this type of cancer is even mentioned, many people say, “Where is the duodenum?” or, “I’ve never heard of that cancer.”
Duodenal cancer is so rare that there is minimal research out there and unfortunately it gets shuffled into the same category as stomach or colon cancer, when, realistically, duodenal cancer is in a category of its own.
I’ve read case study after case study on duodenal cancer and while I’d like to state that what I’ve read is getting better, there’s still a long way to go. The key is as always to catch any type of cancer in time.
Whether lack of testing is due to insurance, money, work or just that slightly dismissive feeling of “I don’t get sick and I feel fine” — a little health maintenance lasts a lifetime.
The duodenum is the first part of the small intestine located between the stomach and the jejunum (the middle part of the small intestine).
After foods combine with stomach acids, they descend into the duodenum where they mix with bile from the gall bladder and digestive juices from the pancreas, just to give you an idea of the importance of this canal per se.
Needless to say, duodenal cancer symptoms are both painful and very warring, ranging from abdominal pain, weight loss, nausea, vomiting and chronic GI bleeding.
Depending on what stage of cancer a person may have is the “cocktail” of chemo, radiation therapy or, if the cancer is contained enough, a Whipple procedure (a major surgical operation involving the pancreas, duodenum and other organs).
I put together my own theory just from reading e-mails from people and seeing Google alerts that come up with the words duodenum or duodenal. The best way to get rid of cancer is to REMOVE it!
Cancer, Chemo, Radiation…they all do a number on your body and senses, and every day is a goal to figure out how to handle it, what to do and how to get through it.
You’ll notice it does a number on the people around you as well, so you’re never alone; everyone is empathetic.
I wanted to end this with a few tips. Although they might seem like common sense, when you’re actually in the moment, you might not be thinking straight.
Prior to starting chemo, go for a nice teeth cleaning (check with your oncologist first as if blood count is low, you won’t be able to). Always have orange peels and put them under your nose for nausea.
There are many appetite stimulants which should be taken to keep your weight on, which will in turn keep your strength up.
The thought of a port (a small medical appliance installed beneath the skin) might seem so permanent and although you’re determined to beat it fast, consider the port as something that, in the long run, could save a lot of unnecessary poking and pinches.
Should the duodenum become inflamed and they want to put a stent in, think hard and long about that, as chemo could shrink it and cause the stent to shift, which would cause even more problems you just don’t need.
I’m always available to chat with anyone going through duodenal cancer.
Visit here to contact Adrienne.
Source: DuodenalCancer.com
Swelling in Both Ankles: Can’t Find Cause?

What can be causing the “edema” or swelling in both of your ankles when everything’s been ruled out?
One day I noticed that my ankle area (both feet) was very mildly puffy (swelling).
Did I have edema? Edema is fluid retention and has many causes, some serious and some benign.
I first thought it was because I’d been wearing tight socks, but I quickly ruled that out.
I then thought it was a menstrual cycle coming, but it never came (not surprising because I hadn’t had one for nine months).
I then blamed menopause, which I obviously was going through. However, I still wondered.
The cardiologist I’ve seen a few times for routine heart disease screening took one look at both my ankles and immediately agreed that I had mild edema and said it was “akin to a few grey hairs” and nothing to be concerned about.
My primary care physician took one look at both my ankles and said they looked great; no edema.
However, further into the appointment she then said that there could be “trace edema.”
A dermatologist looked at both ankles and immediately said they looked normal and that there was no edema or swelling.
A gynecological nurse examined both ankles and she too said there was no edema and they looked perfectly normal.
So, do I have edema in both ankles or not?
A cardiologist sees a lot of this condition because heart failure is a classic cause.
I’d also think that a gynecological nurse sees a lot since PMS can cause swelling, and so can pregnancy.
A primary care physician would see it too, since they see patients with all sorts of conditions just for routine checkups.
A dermatologist will sooner or later run into it and get a good look at it simply by checking for skin cancer on the lower legs.
When I discovered the “edema” I had to go with the consensus that I actually did not have this condition after all.
If you believe you have mild swelling in your ankle area, there’s a possibility you actually don’t have any fluid retention.
What can masquerade as fluid retention is your unfamiliarity with how the skin about your ankles has changed over time.
I wasn’t in the habit of examining this area because there are no moles there, and when I shave, I don’t really look closely at the area.
But the day I discovered what I thought was swelling was when I just happened to take a look from a viewpoint that I normally never did. I have no idea how long my ankles have had this appearance, either.
The dermatologist said that skin loses elasticity as we get older, and when I grabbed at the puffy areas, she said it was skin.
There’s less muscle in that area, so that’s why the skin was “grabbier” than the skin along the calve.
If you were to see my ankles you wouldn’t think they were swollen or had edema; they’re actually skinny. But what had caught my attention was their apparent composition.
There seemed to be fluid under the skin because the skin was fleshy and soft-looking. And “grabby.”
You may want to take a good look at your ankle area and make a note of what they look like. I had never done this.
A tip-off that you probably don’t have edema is that you can see veins under your skin (such as below), and the area has indents from sinew.


My blood tests for kidney and liver function were normal. My thyroid is normal.
My celiac test was negative. I don’t sit or stand excessively. My diet is very low in sodium.
My heart is in perfect condition. There are no other symptoms like pain in the legs that can signal venous insufficiency.
Again, the consensus is that I don’t have edema or swelling in the ankles. Maybe you don’t, after all, either.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/srisakorn wonglakorn
Mole with White Spot in Center

Find out what it could mean if a mole has a white spot in it.
I have a mole that has a white (or actually, flesh or cream colored; it’s hard to tell) spot kind of in the center of it.
I’ve been aware of this for several years since I began doing exams of my skin.
My primary dermatologist wondered if it had always been there and examined it more closely with a dermatoscope.
When I said it had always been there since I began doing skin exams, she didn’t seem concerned, but she pointed out that she thought it appeared to be an area of missing pigment.
She then said it could be a hair follicle.
When pigment appears to go missing is what can be of concern. What appears to be missing pigment could actually be a change in the color of a portion of a mole.
Shortly after seeing my primary dermatologist, I visited a second dermatology office where I get my serial digital dermoscopy done; I was due for another annual visit.
The dermatology resident said it was a hair follicle after I asked him what the “white spot” in my mole was.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Image Point Fr
What if You Get a DVT While on Coumadin (Warfarin)?
Is it possible for someone to get a deep vein thrombosis while on the blood thinner coumadin (Warfarin), and if so, why?
This is a prescription drug that’s so effective at thinning blood, that it carries the risk of internal bleeding, including in the brain.
Once a definitive diagnosis is made, the patient is placed on anticoagulation, which typically is that of coumadin (Warfarin), says Dr. Kurtis Kim, MD, a vascular surgeon with Vein & Vascular Institute of Central Maryland.
A common reason for being placed on a blood thinner is to help prevent DVT as a result of surgery, particularly joint replacement.
Joint replacement surgery is notorious for heightening the risk of a blood clot.
Abdominal surgery is another type of operation that will put the patient at high risk for a deep vein thrombosis.
Dr. Kim explains that a “very small percentage of people who develop DVT” are on a blood thinner.
And when this does happen, “one must ask the following questions:
#1) Is this patient compliant with this medication?” and
#2) “Is the medication at a therapeutic level (for example coumadin needs to be dosed to achieve an INR of 2-3).”
The third check is to review other risk factors for a deep vein thrombosis.
INR stands for international normalized ratio. It’s a numerical value that correlates to how long it takes the blood to clot. The higher the number, the longer it takes.
The first time someone takes coumadin, the INR will not be in the therapeutic (or DVT prevention) range.
It has to build up. And it fluctuates, which is why when someone is prescribed coumadin to take for a while, they must have regular blood draws to make sure that the INR is within therapeutic range.
After my father fell and hit his head, resulting in neurological symptoms, the doctor reduced the coumadin dose to bring the INR down to 1.5.
He had had knee replacement surgery a week prior, and the fall resulted from passing out — for reasons that still remain somewhat of a mystery, though the best theory is that his blood pressure had plummeted as a result of drug interactions.
The INR was dropped to 1.5 because he was at risk for having a brain bleed from the fall.
However, after he was released from the hospital, the doctor increased the coumadin dose and the targeted INR.
Coumadin is very effective at DVT prevention, but it’s not 100 percent guaranteed to prevent a deep vein thrombosis.
 Specializing in minimally invasive procedures, Dr. Kim combines medical expertise with a caring approach to diagnose and treat patients with circulatory issues including leg pain, swelling and blood clots in the legs and lungs.
Specializing in minimally invasive procedures, Dr. Kim combines medical expertise with a caring approach to diagnose and treat patients with circulatory issues including leg pain, swelling and blood clots in the legs and lungs.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Number of DVTs Missed by Ultrasound
Ultrasound (Doppler scan) is not 100 percent effective at detecting a deep vein thrombosis, a life-threatening blood clot that can dislodge and travel to the lungs and be fatal.
Percentage of DVT’s Missed by Ultrasound
“Sensitivity and specificity of ultrasound detecting DVT in the leg above the knee is 97% and 94%, respectively, meaning, while they are very accurate, it can miss it,” explains Dr. Kurtis Kim, MD, a vascular surgeon with Vein & Vascular Institute of Central Maryland.
Dr. Kim continues, “This stresses the importance of seeing a specialist, as at times, even with negative ultrasound, physicians initiate anticoagulation due to strong clinical suspicion.”
If a physician suspects a deep vein thrombosis – even in the absence of a positive ultrasound result – the doctor will prescribe anticoagulant medication (blood thinners).
What would make a doctor suspect a DVT if the ultrasound is negative?
The physician knows that the ultrasound will, on average, miss a very small percentage of deep vein thromboses detection. But what brought the patient into the exam room in the first place?
Suppose both the patient’s legs are swollen. There is no pain or redness. A week prior the patient had back surgery and reports that for the past week he’s been doing way more sitting than usual.
The ultrasound of his legs is negative; no apparent DVT.
A doctor won’t have a high suspicion of a blood clot due to this patient’s presentation and medical history.
The suspicion for DVT when both legs are swollen equally isn’t very high, especially since excessive sitting (such as that can occur after back surgery) can cause edema or fluid retention in the legs.
But if a patient presents with only one leg newly swollen, and it has a reddish color, and the calf area hurts regardless of activity or rest – the doctor will suspect a deep vein thrombosis even if the ultrasound is negative.
“Unlike CT or X-ray, accuracy of ultrasound is highly operator-dependent, so finding a good vascular specialist and associated vascular lab is important,” says Dr. Kim.
 Specializing in minimally invasive procedures, Dr. Kim combines medical expertise with a caring approach to diagnose and treat patients with circulatory issues including leg pain, swelling and blood clots in the legs and lungs.
Specializing in minimally invasive procedures, Dr. Kim combines medical expertise with a caring approach to diagnose and treat patients with circulatory issues including leg pain, swelling and blood clots in the legs and lungs.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Artemida-psy
How Do Stockings Prevent Blood Clots after Surgery?

Are you scheduled for surgery and are wondering why you’ll need to wear stockings?
These help prevent blood clots, which can travel to the lungs and be fatal.
The stockings are actually called TED hose. TED is an acronym that stands for thromboembolism deterrant.
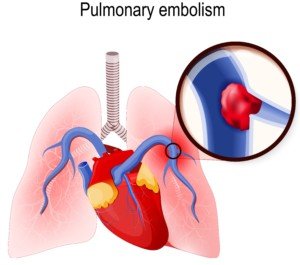
A thromboembolism is the term referred to deep vein thromboses (blood clots) that can travel to the lungs and become a pulmonary embolism.
“Many data support the use of TED hose but has not shown to prevent postoperative DVT on its own,” says Dr. Kurtis Kim, MD, a vascular surgeon with Vein & Vascular Institute of Central Maryland.
“Depending on the situation (how big the surgery was, how immobile the patient was prior to, does this surgery limit patient ambulation, prior history of DVT, age, ongoing medical issues, etc.), some are placed on prophylactic anticoagulation or placement of inferior vena cava [filter] due to significant predictable risk.”
Anticoagulation refers to blood thinners. The IVC filter is placed in the IVC vein to trap any broken-off DVT fragments that are traveling towards the lungs — like a net catching fish.
“Same orthopedic surgery can pose high risk for patients who has limited mobility already with prior history of DVT vs. 40 year old athlete who is walking out of the hospital,” says Dr. Kim.
“While more standardized treatment guidelines seem ideal, individually tailored treatment is far more important.”
If you’re scheduled for joint replacement surgery or any major surgery for that matter, be sure to discuss DVT prevention with your surgeon.
This includes asking questions about the use of TED hose or “stockings.”
Deep vein thromboses are common, and the postoperative period is one of the riskiest times for these blood clots to form.
After surgery, especially for procedures involving the legs or pelvis, patients are at increased risk for DVT due to reduced mobility, changes in blood flow and potential damage to blood vessels.
During recovery, prolonged periods of immobility or bed rest can contribute to blood pooling in the veins, which raises the risk of clot formation.
Symptoms of a Deep Vein Thrombosis
Though about half of all people with a DVT will not have symptoms, this condition is responsible for the following classic signs:
- A portion of the leg is reddish/pink.
- The area of discoloration is swollen.
- The area may also be unusually warm to the touch — warmer than the surrounding normal areas of skin or the same area on the opposite leg.
- Cramping or pain in the lower leg or behind the knee. This cramping does not correlate to movement.
Though TED hose may be part of the postoperative prevention plan for a DVT, blood thinners and pneumatic compression (leg wrap device) are far more effective.
 Specializing in minimally invasive procedures, Dr. Kim combines medical expertise with a caring approach to diagnose and treat patients with circulatory issues including leg pain, swelling and blood clots in the legs and lungs.
Specializing in minimally invasive procedures, Dr. Kim combines medical expertise with a caring approach to diagnose and treat patients with circulatory issues including leg pain, swelling and blood clots in the legs and lungs.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: James Heilman, MD, CreativeCommons
Acute Subdural Hematoma WITH Pulmonary Embolism!
How is a patient treated if presenting simultaneously with an acute subdural hematoma AND a massive pulmonary embolism?
Can anything be more vexing?
For example, a patient arrives at the emergency room from a motor vehicle accident, with a suspected acute subdural hematoma, but is also showing signs of a massive pulmonary embolism.
Yes, it’s possible. The massive pulmonary embolism wouldn’t necessarily arise from the vehicular accident.
For all we know, the patient had recent knee replacement surgery; or is a smoker on birth control pills; or is obese who very recently ended a long airplane flight—all risk factors for a DVT — which can break apart and lead to a pulmonary embolism.
An acute (not chronic) subdural hematoma is a life-threatening situation that requires immediate surgical intervention.
A massive pulmonary embolism also is life-threatening and must be treated immediately. Both conditions are confirmed with a CAT scan.
However…the treatments are polar opposites!
Give a blood thinner to a person whose brain is bleeding from an acute subdural hematoma, and this will intensify the hemorrhaging.
But if the acute subdural hematoma is treated before the pulmonary embolism is, the PE could kill the patient while the craniectomy is being performed.
What a Vascular Surgeon Says
“You’re describing a patient in severe duress with significant neurologic changes and near-hemodynamic collapse,” begins Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
“These always have to be looked at on a case by case basis, so it is impossible to say what I would do, but the issues would be this: relieving the SDH and restoration of blood flow to the pulmonary artery which is causing the hemodynamic instability.
“If pressors alone were not alleviating this, then the possibility of mechanical thrombolysis (removing the clot from either an endovascular or open surgical technique without the use of systemic anticoagulation) exists and may be the best option.”
- Pressors: medications that increase blood pressure and/or cardiac function, says Dr. Casey.
- Systemic anticoagulation: blood thinner given intravenously; it will circulate throughout entire body, including the brain.
But which doctor (neurosurgeon or vascular surgeon/interventional radiologist) should “go first”?
“It is unlikely that a neurosurgeon would be doing a craniotomy (relieving the bleed in the skull) while anyone else would be doing an angiogram or sternotomy (cracking the chest) at the exact same time.”
A massive pulmonary embolism can require cracking of the chest for access to the lungs.
“Perhaps it has been described in the literature, but it is not common and I’ve never seen or been a part of that combined approach,” says Dr. Casey
Simultaneous pulmonary embolism and acute subdural hematoma would be nothing less than agonizing for doctors to be faced with.
Shutterstock/Designua
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.