Unexplained Jump in Triglyceride Levels in Healthy Adult

Find out a possible explanation for why your triglyceride level has jumped from last time you had it taken.
You awaken at 7 a.m., knowing that at 10 a.m. you’ll be going to the medical clinic to get your blood drawn for a lipid panel.
You drink nothing, no water, not even coffee. That’s because along with the blood draw for the lipid panel, you’re also getting blood drawn for the fasting glucose reading.
The results show a marked jump in your triglyceride level compared to last time.
What on earth? You haven’t changed your eating habits; you still exercise; have not gained weight.
Though menopausal transition can cause a spike in triglyceride levels, what if this happens but you’re nowhere near menopause or you’re a man?
“Prolonged or chronic dehydration can cause cell walls to thicken and increase production of cholesterol, making the numbers falsely elevated,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
“Many physicians counsel of fasting but do not remind patients to stay well-hydrated.”
So there’s a pretty good chance that your triglyceride jump is due to the dehydration that preceded it.
Think about that: No water for three hours since awakening; no water during the eight hours you slept; no water for three hours preceding bedtime. That’s 14 hours without fluids.
• What if you’re well-hydrated at bedtime, but then drink no water between awakening next morning and your lipid panel draw several hours later?
• How much of an elevation in triglycerides might this cause?
“I don’t think we have an actual answer to that,” says Dr. Stevens-Cohen. But she does say this:
“I do not believe that fasting the day of the test would cause a significant increase in triglyceride levels.
“Most labs suggest patients remain well-hydrated, but they do not define how long it would take to cause a significant increase in triglyceride levels.”
Having a repeat test a few weeks later would be a good idea if you still haven’t figured out why there was a jump.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sukiyaki
Ovarian Cancer vs. IBS Symptoms Explained by Doctor

Here’s what a cancer-gyn doctor says about ovarian cancer vs. IBS symptoms.
There are many articles or forum postings online with titles like “ovarian cancer vs. IBS” or “Is it IBS or ovarian cancer.”
I decided to get information straight from a gynecological oncologist: a physician who specializes in cancer of the female reproductive system.
Justin Chura, MD, is a gynecological oncologist in Philadelphia, PA.
Dr. Chura refers to a report by Goff et al. that appeared in JAMA 291(22): 2705-12, 2004.
The report consists of two tables that show a comparison between the symptoms of ovarian cancer and non-OC-related symptoms, as well as IBS.
“The first [table] shows that ovarian cancer patients were more likely to have pelvic pain than IBS patients,” says Dr. Chura.
“They were also more likely to have bloating, increased abdominal size and urinary symptoms compared to IBS patients.
“Additionally, ovarian cancer patients were more likely to have a combination of 3-4 symptoms compared to the IBS patients.”
The Vagueness of Ovarian Cancer Symptoms

Shutterstock/fizkes
“The issue is that the symptoms for ovarian cancer are what we call non-specific,” says Dr. Chura.
“Patients with uterine cancer have a very clear symptom which is bleeding after menopause.
“Thus, these patients get diagnosed at an early stage because they seek medical care.
“For ovarian cancer, there is no symptom that identifies the disease at an early stage.
“Furthermore, there is no screening to identify the disease at an early stage.”
IBS Symptoms
Some IBS patients report a lot of pain, which can be in the leg and back (OC can also cause these symptoms), and they can get a lot of diarrhea and constipation—including alternating.
The overlap between the symptoms of IBS and ovarian cancer have the potential to be markedly similar — and on paper, outright identical.
So what should you do?
First of all, get this in your head: IBS is a diagnosis of exclusion! A doctor shouldn’t be sure that you have IBS unless all other causes of your symptoms have been diagnostically ruled out.
“You could have IBS” is told to patients quite often, and I myself even heard this from the GI nurse who was prepping me for my colonoscopy to find out why I was having strange diarrhea and altered BMs.
My condition turned out to be microscopic colitis—but the diagnosis was verified under a microscope. However, IBS remained a differential diagnosis up till that point.
There is no diagnostic test for IBS.
If you’re being told you have IBS, you’d better be sure that all serious (and benign) differentials have been diagnostically ruled out.
Unfortunately, the only diagnostic test for ovarian cancer is a biopsy of the “mass” on/in the ovary. Even an internal ultrasound cannot diagnose.
If you’re having troubling symptoms or “vague,” “non-specific” symptoms that, on paper, point equally to IBS and ovarian cancer, see a gynecologist first. Ask, “Are my ovaries okay?” Then take it from there.
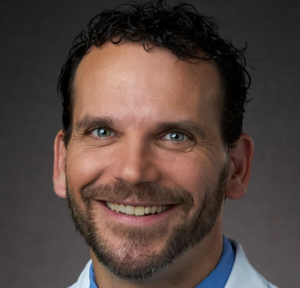 Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Angina Be Ruled out with a CT Scan?

Is it possible for a CT scan to rule out angina?
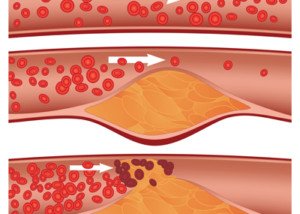
Angina is chest pain caused by blockages in the coronary arteries: coronary heart disease.
It may also be accompanied by shortness of breath and/or nausea.
A CT (“cat”) scan uses radiation to create an image of the heart, so can this device detect angina?
“No. Angina is a symptom that must be provoked by a stressor or stress test,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
“A coronary CT is a non-provocative test. You can see soft plaque and calcified plaque and measure the degree of obstruction.
“However, you cannot tell if a patient’s symptoms are related to that obstruction.
“This is the limitation of coronary CT and why provocative testing with stress tests is the preferred method for diagnosing angina.”
A stress test is often done with a treadmill; the patient walks slowly while the angle of the tread surface is gradually increased to simulate a hill.
Another way is with a stationary bike. A third way, for people who are unable to use their legs such as those with knee problems, is with a drug that makes the heart think that it’s exercising.
As for the CT scan and angina detection — think of it this way: Can an X-ray show joint pain? No. It can show arthritis, but it can’t show the symptom of pain.
Angina is a symptom — chest pain and/or shortness of breath are the two most common — that’s caused by inadequate blood supply through the heart — due to excessive plaque buildup that narrows the inner diameter of the arteries.
Risk Factors for Clogged Arteries — no particular order
- Smoking
- Obesity
- Absence of structured exercise regimen
- Excessive daily sitting
- Untreated sleep apnea
- Junk food diet, or diet of mostly processed goods, even if you’re thin
- Cocaine use
- Advancing age
- Family history of early-onset coronary artery disease

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/airdone
Can You Accidentally Shave Off Melanoma?

Maybe you’ve read a few things about “picking off” a melanoma, but what about shaving it off—by accident?
Are you wondering if melanoma can be picked off?
“It is moles and nevus or seborrheic keratosis which get picked off while shaving or by fingernails,” says Rajiv V. Datta, MD, Medical Director, The Gertrude & Louis Feil Cancer Center; Chair, Department of Surgery, South Nassau Hospital. Dr. Datta performs surgeries on melanoma.
“To remove a melanoma, it has to be deliberate, not accidental. You cannot accidentally shave off melanoma, as it is deep,” he further explains.
“Even if you dig it out with a fingernail, the site does not heal, as it is a melanoma.”
A nevus is another name for a mole (pronounced knee-vus). A seborrheic keratosis is a harmless skin barnacle that can look like a mole, and at times, even resemble melanoma.
A seborrheic keratosis can suddenly start changing in color as well as color distribution, mimicking a malignancy.
Do not pick these off, even though they often look “pickable.” It’s best to have a dermatologist suspect any suspicious lesions.
But as for the idea that melanoma can accidentally be shaved off, Dr. Datta adds:
“Melanocytes are normal cells at the basal layer of the epidermis. These are single cells and can sometime get shaved off.
“Melanoma cells are cancerous which means that they have gone through their cell wall and invaded the surrounding cells; they are also proliferative, meaning that there are a lot of these cells.
“A combination of these makes it difficult to accidentally shave it off.”
 Dr. Datta is an international leader in surgical oncology. Under the direction of Dr. Datta, South Nassau uses leading-edge surgical technologies to remove skin cancer.
Dr. Datta is an international leader in surgical oncology. Under the direction of Dr. Datta, South Nassau uses leading-edge surgical technologies to remove skin cancer.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Oleksandr Nagaiets
Schiff’s MegaRed Krill Oil Capsules Contain Sorbitol: Not Natural

If you’re eager to buy Schiff’s “MegaRed” krill oil capsules, you may want to know that they contain sorbitol—a synthetic version.
When I first saw the TV commercials for Schiff’s MegaRed krill oil capsules, I was very excited that there seemed to be, finally, a high quality omega-3 capsule, since I could not find any at Whole Foods.
I could not find them at regular grocery stores, either, so I had to order them online.
I couldn’t find information about ingredients online, but I figured, what could possibly be in these krill oil capsules that’s bad?
I know that some supplements contain soy, but I banked that Schiff’s MegaRed would not contain soy. And the product doesn’t.
However, doggone it, this product contains sorbitol.
- My question to Schiff: Is this really necessary? SORBITOL?
- Is this an essential ingredient that without it, these krill pills would be useless?
Sorbitol, a sugar alcohol commonly used as a low-calorie sweetener, has been linked to several health issues.
One major concern is its gastrointestinal effects. Sorbitol can cause digestive distress, including bloating, gas and diarrhea, especially when consumed in large amounts.
This occurs because sorbitol is poorly absorbed in the small intestine and fermented by bacteria in the large intestine (Gibson et al., 2007).
Furthermore, sorbitol has a known laxative effect, which can lead to diarrhea if intake exceeds recommended levels.
This property is utilized in some over-the-counter laxatives (Tucker, 1993).
Additionally, despite having a lower glycemic index than regular sugar, sorbitol can still affect blood glucose levels, making it a concern for individuals with diabetes.
It is metabolized more slowly than glucose but can still contribute to overall blood sugar levels (Mann & Cummings, 2004).
Why is this chemical in the MegaRed product?
Now, I don’t know if the amount of this chemical in Schiff’s MegaRed constitutes the same amount that has been linked to a variety of adverse side effects, but what I DO know is this:
1) If something is truly safe, long-term use should not be associated with adverse side effects.
2) Even though I’m not a chemist, I can’t for the life of me imagine why Schiff feels it’s necessary to include this synthetic substance in its MegaRed product.
3) There’s enough seemingly legitimate information on synthetic sorbitol to make me NOT want to buy another bottle of Schiff’s MegaRed.
I’ll just make a point of eating more fish and continuing to take my omega-3 fish oil capsules.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
The Next Step if Your Breast Lump Isn’t on a Mammogram?

Have you found a breast lump but the mammogram is clear? Should you just let this go and put all your faith in the mammogram?
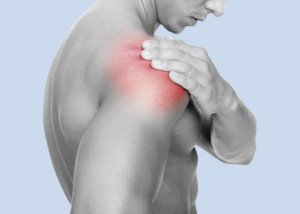
Neck, Throat Soreness: May Be Caused by Exercise
I was noticing a strange though mild soreness in the front of my neck soon after I awakened, and initially didn’t know what could have caused it.
Then I soon realized that the day before, I had been doing standing overhead presses.
This exercise involves standing in one spot with feet about shoulder width apart, and pressing a barbell overhead.
This is not the most common exercise, but it’s a very functional one that also strengthens the lower back. Proper form is crucial.
You may think that the standing overhead press works only the shoulders, arms and core, but pay closer attention next time you’re pressing up a heavy barbell.
The muscles in the neck are subjected to isometric contractions: The muscles are under tension, but do not lengthen or shorten.

If you raise your head just even a little bit while fighting to get the barbell completely over your head, this can set you up for some neck soreness (in the front) the next day.
Since the muscles in the neck go over the throat, you may perceive what seems to be soreness in the throat area as well (not like a “sore throat” from a cold, but a soreness in the front of your neck where the throat is). The soreness may also be under the jaw.
Whenever I have this soreness, it’s the day after heavy standing overhead presses. It’s also very transient in that it dissipates as the day proceeds.
Pay attention to your neck the next time you’re pushing up heavy weight.
You will note that the muscles in this area are straining. They certainly aren’t doing nothing, that’s for sure.
This will be particularly evident if you use good form: feet flat on floor, no jerking up the weight.
A calm rather than jerky pressing motion will enable you to better tune in to how your various muscles are making this exercise possible. The neck is not excluded.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
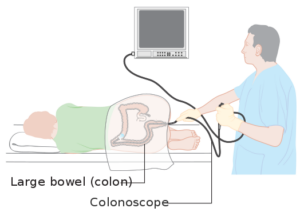
Did the Colonoscopy Miss a Cancer or It’s a New Fast Tumor?

When colon cancer develops between routine colonoscopies, does this mean it was missed or is it usually a new fast growing tumor?
We are advised to have a screening colonoscopy beginning at age 45 and then every 10 years to catch colon cancer.
People with above average risk, including those for whom polyps were found, have shorter intervals between screening colonoscopies.
Nevertheless, it happens: A colon cancer is discovered between colonoscopies.
This includes at some point after the previous colonoscopy was deemed normal.
Imagine being told, “Your colonoscopy was normal,” and then several years later you begin developing concerning symptoms and are diagnosed with colon cancer.
Did the colonoscopy miss this cancer or did it spring up out of nowhere a few years later?
“Interval colon cancers are defined as those cancers diagnosed after a previous colonoscopy and before the next screening/surveillance colonoscopy,” says Santosh Sanagapalli, MD, a consultant gastroenterologist, endoscopist, colonoscopist and specialist in esophageal and bowel disorders.
“There are four possible reasons for interval cancers developing.”
• Polyps that were missed on the initial colonoscopy, that progressed to a cancer.
• Polyps identified on the initial examination, but incompletely resected.
• New polyps developing following the initial colonoscopy, that rapidly progressed (the standard rate of progression from small polyp is generally thought to be at least a decade or more).
• Failure to visualize a cancer that was present on the initial colonoscopy.
“It is very difficult to determine which of the four causes is responsible for development of an individual case of interval cancer.
“However, using mathematical models, others have concluded that the majority of interval cancers result from missed rather than new lesions.
“The colonoscopy is highly dependent on its operator, and there is now plenty of evidence for this.”
How does a colonoscopy miss a tumor?
Cancer Research UK
“There is substantial variation in detection of adenomas (the most common precursor of colorectal cancer),” continues Dr. Sanagapalli.
Researchers from Huntsman Cancer Institute (HCI) at the University of Utah looked into this phenomenon and discovered:
1 The interval colon cancers tended to appear in patients 65-plus
2 In patients with a family history of the disease
3 In those who’ve previously had polyps
Not only that, but the “missed” cancers in the study’s patients tended to appear on the right portion of the colon, which, interestingly, is at the far end of the reach of the colonoscope.
“Further, large U.S. studies have shown that the adenoma detection rate of a colonoscopist (measured as a percentage of all colonoscopies they perform where they detect an adenoma) is inversely proportional to the rate of interval cancer in their patients,” says Dr. Sanagapalli.
“Put in other words, the more adenomas a colonoscopist detects in their colonoscopies, the less likely they are to ‘miss’ significant lesions that can turn into an interval colon cancer.”
This is why, when you’re seeking a gastroenterologist to perform your colonoscopy, you should ask what his or her adenoma detection rate is.
It is perfectly fine for the patient to seek this information, and you should never be reluctant to.
It should be at least 15% for female patients and 25% for male.
Don’t Squawk About the Prep
“If the bowel is not adequately cleansed, fragments of stool and debris can easily obscure a small polyp/adenoma that may then be missed and turned into cancer,” says Dr. Sanagapalli.
“For this reason, much research has gone into improving the quality of bowel preparation in recent years.
“One major advance in recent years is our understanding of the value of ‘split’ bowel preparation.
“This is where the last dose of the bowel preparation is taken on the day of the surgery (usually two to four hours prior to the procedure), rather than the night before.
“This has been shown to improve the quality of bowel preparation significantly, especially in the right colon.
“By doing so, the rate of detection of polyps is improved, and therefore the risk of interval cancers is reduced.
“For this reason, ‘split’ bowel preparation has now become the standard of care.”
Can we ever prevent a missed colon cancer?
“Even with the best colonoscopists and perfect bowel preparation, not all interval cancers will be prevented.
“There is evidence to suggest that around a quarter of interval cancers occur through no deficiency of the initial colonoscopic examination, and are simply due to a new polyp that rapidly progressed.
“Ongoing research is focused on identifying characteristics of patients and polyps that may have rapidly progressed, so we can schedule more frequent colonoscopies for such patients.”
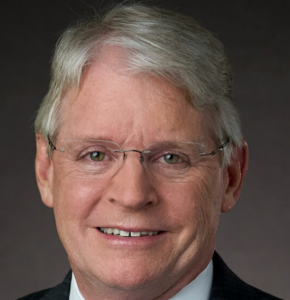
 Dr. Sanagapalli is a gastroenterologist and director of the Esophageal Disorders Center at St Vincent’s Hospital, Darlinghurst. He performs diagnostic and therapeutic endoscopic procedures, and enjoys providing comprehensive and holistic care to patients with a wide variety of disorders affecting the gastrointestinal tract.
Dr. Sanagapalli is a gastroenterologist and director of the Esophageal Disorders Center at St Vincent’s Hospital, Darlinghurst. He performs diagnostic and therapeutic endoscopic procedures, and enjoys providing comprehensive and holistic care to patients with a wide variety of disorders affecting the gastrointestinal tract.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2014/03/140320173512.htm
sscpywrt26
Extremely Dense Breasts: Mammograms & Advanced Imaging

It’s not pretty finding out you have “extremely dense” breasts — because this is a big risk factor for breast cancer; what makes this worse is that a tumor can pass as benign fibrous tissue on a mammogram reading.
A cancer surgeon and a diagnostic radiologist weigh in on extremely dense breasts, mammograms and an advancement in imaging.
Do you have “extremely dense breasts” and have read that this is a risk factor for breast cancer and/or that this situation makes it more difficult for a tumor to be detected by eye on a mammogram?
For this article I consulted with Dr. Steven Standiford, MD, Chief of Staff Emeritus at the Cancer Treatment Centers of America Breast Cancer Institute across all five CTCA sites, and Dr. Debora Fineman, MD, a diagnostic radiologist formerly with the Philadelphia CTCA.
“Regarding extremely dense breasts and the risk of breast cancer, the issue is more that extremely dense breasts make it difficult to DETECT cancer mammographically,” says Dr. Fineman.
Imaging for Extremely Dense Breasts
“A fairly recent advancement in mammography, Tomosynthesis, is quite beneficial in evaluating dense breasts, as it enables visualization of the breast in ‘layers,’” says Dr. Fineman.
“Most insurance companies will not cover this as a screening procedure. We do get tomosynthesis coverage for performing diagnostic workups such as evaluating an abnormal screening mammogram or evaluating a clinical problem.
“Screening tomosynthesis is readily available, with some institutions collecting a nominal out-of-pocket.”
Your gynecologist may order this test for you if it’s available in your health network even if it isn’t covered, so ask about it.
What about the MRI for extremely dense breasts?
Dr. Fineman says that coverage for the cost varies across insurance companies, and that most insurance companies will not pick up the cost for MRI screenings.
“I believe the research has not yet been finalized as to risk stratification and frequency of performing screening MRI evaluations,” adds Dr. Fineman.
Dense (fibrous) breast tissue appears as white on a mammogram. So do tumors. But in addition to this visual issue, it’s true that having more fibrous tissue and less fatty tissue increases a woman’s risk of the cancer.
Just how much of an increase is up for debate. This all begs the question: Why isn’t an MRI screening covered by insurance for patients with dense breasts?
Dr. Standiford has this to say: “I worry about policies mandating coverage of a specific, as yet unproven test – for as yet, MRI has not impacted breast cancer mortality, and the resources could be better utilized in expanding mammography coverage – the impact would be far greater.
“Also, newer technology is on the way, for example higher resolution ultrasound, tomosynthesis mammography and breast CT, which may have more utility in screening dense breasts.”
 As a part of Dr. Standiford’s life-long commitment to improving cancer treatment, he has partaken in wide-ranging research and has been awarded grants to study breast and colon cancer.
As a part of Dr. Standiford’s life-long commitment to improving cancer treatment, he has partaken in wide-ranging research and has been awarded grants to study breast and colon cancer.
 Dr. Fineman has been in practice for 30+ years.
Dr. Fineman has been in practice for 30+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Billion Photos
Can Breast Cancer Be Spread by Mammogram Compression?

Find out what a breast cancer surgeon has to say about the idea that a mammogram can compress a pre-existing tumor and make it spread.
The compression from a mammogram can hurt quite a bit.
This can make some women wonder if this painful compression could somehow squeeze out an undiagnosed malignant tumor to the point of scattering it beyond its local position.
So the big question becomes: If there’s cancer in the breast, can what feels like excessive compression can make it spread or disseminate it to other parts of the body?
The Answer
“Manipulation of a tumor – whether by exam, compression of a mammogram, ‘disrupting’ the tumor with a needle biopsy, or manipulating the tumor at surgery – has NOT been shown to increase the risk of tumor recurrence or dissemination of metastases,” explains Dr. Steven Standiford, MD, Chief of Staff Emeritus at the Cancer Treatment Centers of America Breast Cancer Institute across all five CTCA sites.
Spread of Cancer Cells
Dr. Standiford explains, “Cancer metastasis is a complex dance between tumor cells separating themselves from the initial tumor, having the biochemical reactions that loosen the bonds between cells so that one can break free, having access to blood vessels or lymphatics to have a highway to travel, avoiding identification by the immune system, and having a site which provides an appropriate milieu for the cell to develop into a metastatic lesion.
“Compression, or exposing the tumor to the air, or any other single factor will not change the nature of the disease, which is determined by the tumor and not how hard it is squeezed.”
In short, malignant breast tumors are “tough” and don’t just break apart.
If you are still concerned about the “spread” of cancer cells during a mammogram, you may want to consider having a whole-breast screening performed via ultrasound — as this does not involve compression of the breast tissue.
You should discuss the pros and cons with your women’s health physician regarding screening technology.
Keep in mind that not all insurance plans will cover the cost of a screening ultrasound, and in fact, the procedure may not even be offered by your health plan.
However, independent imaging centers will provide screening ultrasounds for breast cancer, though you may need an authorization from your doctor to have it done.
 As a part of Dr. Standiford’s life-long commitment to improving cancer treatment, he has partaken in wide-ranging research and has been awarded grants to study breast and colon cancer.
As a part of Dr. Standiford’s life-long commitment to improving cancer treatment, he has partaken in wide-ranging research and has been awarded grants to study breast and colon cancer.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.