IBS Cramps vs. Menstrual Cramps (PMS)

A female GI doctor who specializes in women’s GI issues addresses IBS vs. menstrual cramps related to PMS.
What are the differences between IBS cramps and those from premenstrual syndrome?
“The main difference between menstrual cramps and IBS cramps would be the timing,” begins Diana Y. Wu, MD, a gastroenterologist and assistant professor of medicine at Brown Medical School.
“Menstrual cramps usually occur a few days before onset of menstruation, whereas IBS cramps can occur at any time, especially in the mornings, after eating, or in times of stress/anxiety.
“IBS cramps can often be relieved by having a bowel movement. Menstrual cramps tend to be lower in the pelvis and not necessarily relieved with defecation. It tends to resolve after the menstrual cycle is completed.”
The cause of the cramps in irritable bowel syndrome and in PMS differs.
In PMS the cause is hormones called prostaglandins, which is why the anti-prostaglandin drug, ibuprofen, is so effective at relief.
The prostaglandins cause uterine contractions, and that’s the “cramping” that a woman feels.
“Irritable bowel syndrome is characterized by chronic abdominal pain, and associated with changes in stool frequency or consistency (e.g., diarrhea or constipation) in the absence of any physical cause that is detectable by our current medical investigations,” explains Dr. Wu.
“The pain is usually relieved or ameliorated with a bowel movement.”
Perplexing
“The pathophysiology of IBS remains unclear and is believed to be multifactorial,” continues Dr. Wu.
“Despite multiple investigations, data have been conflicting and no abnormality has been found to be specific for this disorder.”
I’ve never had IBS so I can’t describe what the cramping feels like. But I’ve had cramping from premenstrual syndrome and microscopic colitis, and they feel identical.
Ironically (though not surprisingly), prostaglandins are implicated in flare-ups of microscopic colitis, though research in this area is scant.
I know that the cramping I had, during the microscopic colitis flare, was related to this benign inflammatory bowel disease because when it happened, I had already completed menopause. Very fascinating!
But prostaglandins don’t seem to be involved in the cramping of IBS.
Causes of IBS are not clear.
“The traditionally favored hypotheses are: alterations in gastrointestinal motility (no predominant pattern of motor activity has emerged as a marker for IBS), visceral hypersensitivity, alteration in fecal flora (such as after gastrointestinal infection/food poisoning), bacterial overgrowth, food sensitivity or a genetic predisposition,” explains Dr. Wu.

Shutterstock/KDdesignphoto
Bacterial overgrowth and food sensitivities are theorized to be causative factors behind microscopic colitis, which is often misdiagnosed as IBS…and vice versa.
Dr. Wu further explains, “Visceral hypersensitivity (increased sensation in response to stimuli) is a frequent finding in irritable bowel syndrome patients.
“Several studies have focused on increased sensitivity of visceral nerves in the gut, triggered by bowel distention or bloating, as a possible explanation for IBS symptoms.
“About half of patients with IBS experience bloating in addition to abdominal pain.
“They may have a measurable increase in abdominal girth associated with bloating (sensation of abdominal fullness), and this may be due to impaired transit of intestinal gas loads.”
Is there a way a woman can tell if the cramps she feels are IBS related or from PMS or mid-cycle cramping?
“There is no way to know for sure. However, typically IBS cramping is relieved with defecation.”
 Dr. Wu is a graduate of Harvard Medical School and is board certified in gastroenterology and internal medicine. She is well-versed in multiple endoscopic procedures and all GI disorders.
Dr. Wu is a graduate of Harvard Medical School and is board certified in gastroenterology and internal medicine. She is well-versed in multiple endoscopic procedures and all GI disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
How to Lessen Anxiety over Moles and Melanoma

Are you so afraid of your moles that you no longer can look at them, for fear of what you might see?
Serial Digital Dermoscopy
This wonder of technology will give you great peace of mind. I’ve had this procedure electively done and will continue having it done.
Moles are photographed, then examined on the computer screen under high magnification by the dermatologist.

Not only that, but (depending on the specific system) the computer database compares the image to data from melanoma and then comes up with a rating. The rating can be a number or color.
The computer does NOT diagnose melanoma, but it indicates that a mole is suspicious or has characteristics that resemble melanoma more than it resembles a benign lesion.
Based on the rating, the doctor will then decide on further action (or not).
Now imagine the reduction in your anxiety when the doctor tells you, “All of your moles look very stable. You don’t have to come back for another 18 months.”
Serial digital dermoscopy is done yearly, every 18 months or even every two years (depending on the doctor’s recommendations, though you can have it done as often as you’d like).
The same moles are photographed, and the computer program compares new photos to previous images and will detect changes — earlier than a dermatologist possibly can, even with their handheld dermatoscope.
SDD may run about $250, depending on where it’s done.
Home Mole Mapping
Map out your lesions at home (if you don’t have too many), using a large sketch book.
Even if your drawings of various body parts are crude, at least this way you’ll have an idea of where you have moles, so that you will know if new ones have appeared.
This will reduce a lot of anxiety.
Illustrate
If you can illustrate, then draw and render your moles; this will significantly reduce anxiety.
I’ve done this (I can illustrate shape and texture, plus draw scaled-up images; I knew someday this skill would come in handy).
Many artists may not think to do this.
Whip out your favorite illustrating tool and draw your moles, capturing variations in color, patterns, texture, border, etc.
Then, when it’s time to do monthly self-exams, you’ll have a better chance of detecting a change.
Monthly Self-Exam
“An at-home approach to monitoring moles may include the ever popular selfie!” says Emily de Golian, MD, a board certified dermatologist with Forefront Dermatology in Atlanta, GA.

Shutterstock/pixinoo
“Take a photo of any moles in question from a distance for orientation, so you can tell which body part is being photographed, and close-up to capture what the mole looks like in detail,” continues Dr. de Golian.
“You can compare your skin to these selfies periodically, such as during a monthly skin self-exam, and if any changes have occurred, call your dermatologist for an appointment.”
Commit to a self-skin exam every month without fail. This way you won’t wonder, “When did this mole begin changing?” or, “Did this mole look this way only a few weeks ago?” The monthly selfie will cut a lot of anxiety.
Annual Clinical Exam
Have a dermatologist examine your skin from head to toe, and make sure they use a dermatoscope. This will lower anxiety.
“Annual skin exams and any required follow-up are typically covered by insurance,” says Dr. de Golian.
“Patients should call for a sooner follow-up if they notice any new or changing spots.”

shutterstock/wavebreakmedia
Know that only 30 percent of melanomas arise in pre-existing moles (Yale School of Medicine).
Next, to reduce mole anxiety and if you’re tech savvy, you can get an application for your smartphone that works in a similar way to digital serial dermascopy.
There are many apps like this, but they do NOT replace the type of digital serial dermoscopy that was described previously.
Consider it an adjunct to your skin health surveillance program.
Finally, to rid yourself of mole anxiety, have the spot removed and biopsied.
Don’t put this off. Just get it done. Depending on your insurance plan, you won’t have to pay for this other than the copay.
If you want to get rid of mole anxiety as much a possible, the money invested to do this will be well worth it.
 Dr. de Golian focuses on the surgical treatment of skin cancer via Mohs surgery, cutaneous oncology (melanoma and basal cell carcinoma), surgical defect reconstruction and cosmetic dermatology.
Dr. de Golian focuses on the surgical treatment of skin cancer via Mohs surgery, cutaneous oncology (melanoma and basal cell carcinoma), surgical defect reconstruction and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Source: medicine.yale.edu/dermatology/
Elderly Parent Refuses to Go to ER: How to Make Them

Here is how to make a stubborn elderly parent go to the emergency room.
Have you ever heard of a case in which an elderly person died because their medical treatment was delayed, because family members couldn’t get that individual to visit the emergency room?
I’ve always wondered how it’s not possible for the adult child of an elderly person, who’s compromised by an illness or injury, to make them get into a car and be driven to an emergency room.
I made my elderly mother, who refused to go to the ER, get in the car and be driven to the ER.
She was delirious and wouldn’t keep still, requiring nonstop supervision.
The delirium ultimately had been diagnosed as a side effect from a type of medication that, in a very small percentage of recipients, causes a reactive “psychosis.”
The drug had been prescribed by a neurosurgeon to mitigate fluid buildup in her brain as a result of a recurrence of a chronic subdural hematoma.
So to this day, we’ll never know how much of that “psychosis” was brought on by the increasing blood and fluid in her brain (sounds frightening but she fully recovered).
My elderly mother flat-out refused to go to the emergency room, even though I and my father were insisting on this.
My father had orthopedic issues and was not in a position to use a hands-on approach to make my mother get into the car.
Look, if you have an elderly parent who needs to go to the ER, and he or she refuses, there is NOTHING stopping you from doing what you intuitively know is the right thing to do!
I forced my mother into the car. This sounds like I used violence, but all I did was stand behind her, place my hands on her upper arms, and “force” her to walk out of the kitchen, through the laundry room and into the garage. There was no way she could break loose.
Holding her upper arm with one hand, I opened the car door with the other hand, and I made her get into the front seat.
I turned her body to face the open door and gently pushed downward, making her lower.
I guided her into the seat, lifting her legs into the car, then quickly closing the door. I then put her seatbelt on.
My father and I knew she’d try to get out. I quickly got in behind her as my father put on the automatic lock for all the doors.
This way my mother couldn’t open her door. She was still verbally delirious and insisting she be let out.
The drive to the hospital took 40 minutes, during which I kept my hands firmly on my mother’s shoulders while I sat behind her.
Several times she reached for the door handle, and I didn’t quite trust that automatic lock.
I kept her pinned against the seat with my hands. She kept saying she wanted to jump out.
The CAT scan at the emergency room revealed the chronic subdural hematoma, and since the scan looked pretty much the same when compared to the one that had been taken a few days ago, the ER doctor deemed my mother’s behavior to be an adverse reaction to the drug.
She was admitted and underwent a second burr-hole operation to evacuate the cSDH, then fully recovered within a few weeks.
You do NOT have to injure or bruise an elderly parent in order to “force” them to walk to a car, get in, and be driven to the ER.
If your elderly parent can’t walk (my mother had no problem walking), then pick them up.
If your parent is heavy, then of course, picking them up won’t always be an option.
If it’s impossible to get them into a chair with wheels or a wheelchair and roll them to the car, then hoist them in, or if two people find they can’t dually carry the person, then call 9-1-1.
If an elderly person falls and can’t move much, leave them be and let professionals do the moving!
When my elderly father blacked out, fell, hit his head and had an altered mental status at 3:00 in the morning, I found him on all fours (elbows on floor).
This was a week after he had total knee revision surgery.
Though he was conscious, all 190 pounds of him, combined with the inability to realize he needed to try to get into a seated position on the floor, made his body dead weight.
I took the mobile phone into another room and dialed 9-1-1.
He didn’t want me to call 9-1-1, and my mother was even swayed by his insistence that he was alright (by then she had talked him into making his way, along the floor, to a seated position on the floor with his back against the bed).
But I wouldn’t have it. Within minutes, four EMTs arrived and properly transferred my father, neck brace and all, into a special chair and secured him in it, then carried the chair down a flight of stairs and out the front door. He fully recovered.
So as you can see, there’s really NO reason why you can’t somehow, some way, get an elderly parent to the emergency room, no matter how much they refuse to go.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Racing Heart after Climbing Stairs: Cause & Solution
If your heart races after you climb a flight of stairs, here’s one reason why and how to solve this problem.
When I worked as a personal trainer at a large gym, I’d have my clients simply walk up a flight of stairs to see if they’d get a racing heart.
I just want to first encourage those who experience a racing heart after going up a flight of stairs to have a complete exam by a cardiologist.
A healthy person (no heart troubles) who is de-conditioned due to lack of exercise will experience a racing heart after climbing stairs fast enough.
Even a slow pace can get the heart rate shooting up in an otherwise healthy person.
When I was in a volleyball club years ago, consisting of primarily 20-somethings, these young people hated having to climb five flights of stairs to get to the fifth story of the building where the courts were set up — and these were experienced volleyball players.
Going up flights of stairs is no picnic, even to athletes.
Climbing stairs, to any out-of-shape individual, is a bear, and it’s expected that their heart would be racing at the top.
If climbing stairs produces other symptoms besides a racing heart, this would be cause for concern, such as chest pain, nausea and feeling faint.
A heart that’s not conditioned will race under exertional circumstances, even in the absence of an abnormality, heart disease or other medical condition.
The Fix Is to Exercise
You may already think you’re getting plenty of exercise, including “going up and down the staircase at home a hundred times a day.”
But use of a staircase in the activities of daily living is not sufficient to overcome the racing heart issue.

Casual use is not enough. Shutterstock/Javani LLC
Program for Preventing a Racing Heart from Climbing Stairs in a Healthy Individual
Incorporate twice weekly sessions of high intensity interval training.
HIIT will teach your heart to get used to brief high loads of exertion and to recover quickly from them.
HIIT is superior to inducing this kind of cardiac fitness when compared to steady state aerobic sessions.
For best results, conduct HIIT using a staircase.
One of the versions of this that’s very effective is to dash up a flight of stairs while holding dumbbells or weight plates.
The “dash” can be a walk, if that’s all you can do with the weights.

The objective is to move as fast as you can (even if it’s a slow pace) while holding the weights.
At the top of the stairs following one of these dashes, your heart should be racing. That’s the objective.
If it’s not racing, go faster or use heavier weights. (Of course, if you get chest pain, nausea or otherwise feel sick, stop the activity.)
So if holding 10 pound dumbbells no longer is difficult even with a fast trot, then see what happens when you use 12- or 15-pounders. Use more weight over time.

At the top, set down the weights and walk around for one to two minutes, then do another set (four or five total).
Do not sit or stand still during the rests. Keep moving during the recovery.
For healthy beginners, you should have a rating of perceived exertion of 6-7 at the top of the staircase.
For fitter people, aim for an RPE of 8-9. This is based on a scale of 1 to 10, where 1 = how you’d feel soaking in a hot tub, and 10 = how you’d feel after trying to outrun a train.
The ideal staircase is at least 30 steps (two or more flights), but don’t climb so many steps that after 30 seconds, you’re still climbing.
This is supposed to be short, brief bursts of exertion, not a pacing type of movement.
To prevent your heart from racing from casual use of a staircase (like on the job or around the house), you must get your heart racing via HIIT, and twice a week is all you need.
On one or two additional days, yes, I encourage steady state cardio.
But if you rely only on steady state (long duration aerobics), it won’t produce the spectacular results of HIIT.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/Orawan Pattarawimonchai
Is Daily Aspirin Beneficial if You Have a Zero Calcium Score?

Here’s information if you’ve ever wondered if it would be worth it to take a daily aspirin even though you’re calcium score is zero.
Are you wondering if there would be any benefit to taking a daily aspirin because your coronary calcium score is zero?
Would popping a small aspirin every day make your risk of heart attack even lower?
I wondered about that, as I my calcium score is zero; I figured that adding a daily aspirin would really, really make me resistant to a heart attack.
Now, a study has come out answering this question. Michael D. Miedema, MD, the study’s lead author, says in the paper, “Many heart attacks and strokes occur in individuals who do not appear to be at high risk.”
Dr. Miedema points out that treating only those people with a high risk of heart attack with a daily aspirin means that a “substantial portion of patients” without high risk will go on to have a heart attack that maybe could have been prevented with daily aspirin therapy.
Aspirin, because it’s a blood thinner, can cause internal bleeding. This is the problem with taking this drug when you aren’t at high risk for a heart attack; you risk internal bleeding to prevent a heart attack that would have never occurred in the first place.
The American Heart Association recommends aspirin for those who have known cardiovascular disease or who are at high risk for a heart attack. This drug is not advised for those at low or even intermediate risk.
Dr. Miedema’s study looked at over 4,200 participants who were followed for about seven years.
They were grouped according to their calcium scores. Heart attack rates in each group were calculated.
Results
Subjects with calcium scores over 100 were two to four times more likely to benefit from daily aspirin than to be harmed, even if they didn’t qualify for daily use according to the current AHA guidelines.
Subjects with a calcium score of zero were two to four times more likely to suffer harm from aspirin than any benefits.
These results stood ground even when traditional risk factors were accounted for.
The results mean that significant plaque buildup means this individual is “much more likely to prevent a heart attack with aspirin use,” says Dr. Miedema in the report, “than to suffer a significant bleed.”
But conversely, if you have a zero calcium score, the daily aspirin would result in more harm than anything good — even if you have any risk factors for heart disease (e.g., high cholesterol).
Dr. Miedema says that a zero calcium score “is associated with a very low risk of having a heart attack.” He adds that such individuals may not benefit from preventive drugs.
Well, that does it for me. I have not yet taken the daily aspirin, and I have decided not to.
Why risk internal bleeding, which I’d more likely suffer than a heart attack, what with my zero calcium score?
Nevertheless, if you’re not sure what to do, consult with a board certified cardiologist.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Photographee.eu
Source: sciencedaily.com/releases/2014/05/140509172919.htm
Dent in Middle of Thigh Muscles Is Benign, Harmless
There’s no cause for alarm about that dent in the middle of the front of your thigh; there’s a benign explanation.
As a result of consulting with Dr. Google, many people are in a state of panic upon discovering a “dent” in the middle of their upper thigh.
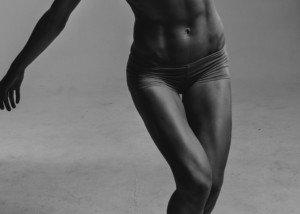
Check out the woman below; does she have the same kind of dent in the middle of her upper thighs as in yours?
This athlete’s thigh has an elongated dent.

The lower central dent is caused by the tendon that’s between the two pennate structures of the rectus femoris muscle.
The rectus femoris is a pennate type of muscle. This means that the muscle fibers attach diagonally to the central tendon that divides the two sections of this muscle.
So more specifically, the rectus femoris is a bipennate structure (“bi” meaning two). You can clearly see this in the anatomical illustration below.

The more muscle fiber in any given cross-section, the more force that can be generated.
Quadriceps muscles are pennates in order to be very potent force producers (think sprinting, squatting, jumping, leg pressing, kicking down doors).
The reason that the muscle fibers attach diagonally to that central tendon is to get as much of the muscle fiber as possible in any given cross-section.
The central tendon will be more visible in a person who has lower bodyfat, in combination with toned muscles.
If you see a dent that wasn’t in your middle front thigh before, you’ve either lost some bodyfat and/or increased the tone of your muscles.
Dents in the thighs actually go by several names in the bodybuilding/physique-sculpting community: cut, crack and definition. The goal of such athletes is to get as deep a cut as possible.
There’s a reason why you’ve never seen flabby, mushy thighs with dents in them.
Soft, untoned muscles aren’t firm enough to create this impression, especially if there’s a higher level of bodyfat.
Thus, a “skinny fat” person can be minus a visible dent in their thigh.
People who’d be considered “fat” won’t have a visible dent in their thigh, middle or anywhere.
Do not freak out or feel fear upon looking at your thigh dent.
Instead, reassure yourself with anatomy illustrations and images of physique athletes.
Google “sculpted thighs,” and similar keywords, such as “bodybuilders’ legs,” and “lean muscular quads,” etc. You’ll see plenty of dents.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Indent in Outer Thigh Muscle Explained
Here is why you should calm down and stop worrying about that indentation in your outer thigh muscle.
I’m going to tell you why seeing an indent in your outer thigh is actually a GOOD sign.
I’m a former certified personal trainer and of course, a fitness expert — very knowledgeable of human anatomy and the musculoskeletal system.
By far, and I mean VERY FAR, the most likely explanation for an indent in your outer thigh muscle is NORMAL HUMAN ANATOMY.
We are not perfectly smooth and flat under our skin.
Take a good look at the quad indents in the legs shown at the top of this article. How many do you see? I count four on the leg closest to the viewer.
Look at the outer right thigh in the woman below.

Frankly, I think that the “dent” is attractive. There is a less obvious dent above it, just below her panty line. Both are normal human anatomy.
Do you see YOUR indent in the above photo?
I know the indent you’re speaking of, because it’s usually the first one to show when a person’s bodyfat gets low enough and they already have some tone to the thigh muscles.
Below is an anatomical illustration that clearly shows grooves between major muscles. These grooves are the sources of dents, when bodyfat is low enough.

Shutterstock/Sebastian Kaulitzk
Depending on your bodyfat level, you can make the indent in your outer thigh disappear (or rather, get hidden) by gaining fat.
Eat up, gorge and put on fat, and this additional fat will conceal the indent or make it less noticeable. Guaranteed for normal anatomy.
The less bodyfat with toned muscles, the more visible will be the separation between the muscles. Less bodyfat is a desirable feature!
Physique athletes (not just bulky bodybuilders) LOVE to see indentations in their quads.
It’s a sign of reduced bodyfat.
The lingo in the muscle-building community is cut, definition or crack. But you need NOT be a physique enthusiast to “get” an indent in your outer thigh.
People with flabby, mushy muscles but also low bodyfat will probably not see this groove; or, it’ll be hardly noticeable.
The people most likely to notice it, who are not deliberately trying to get it, are those who exercise or play sports (and therefore have toned leg muscles), and have a low bodyfat level in that area.
When I say “low,” I don’t mean as low as a physique athlete posing on stage, but “low” as in: There’s really no excess fat there, no plumpness kind of fat.
If your weight fluctuates or you’re a yo-yo dieter, take notice of what these weight fluctuations do to the indent. The heavier you are (with fat), the less visible the indent.

Shutterstock/Syda Productions
People may panic if they notice that the indent comes and goes, but this coming-and going parallels weight fluctuations.
Other types of athletes also have this indent in their outer thigh, and the fact that athletes have this should reassure you that it’s benign, harmless.
Do some googling of images for soccer players, tennis players, any athlete where there are generous views of their outer thighs, and you’ll see lots of indentations — just like yours!
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/Weitwinkel
Angina Vomiting vs. from Bad Food or Anxiety

Is there a way to tell the difference between the vomiting from angina and that from anxiety or bad food?
“Angina vomiting would be similar to any form of angina; that is, it would be brought on by physical activity or severe emotional stress and go away when the stress is removed,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“It would typically be associated with chest pain (but not always), sweating, difficulty breathing or other signs of a heart attack.”
Bad Food
“Vomiting caused by bad food will usually start just after eating the food, be accompanied by abdominal cramping and/or diarrhea.
“True food poisoning may include fever and chills and the vomiting will be very copious until the stomach is emptied.”
One time when I gorged on pizza loaded with ground beef, I upchucked rather copiously.
When my mother vomited two days before a catheter angiogram showed life-threatening blockages in her coronary arteries, it was just a few gobs of goop in the waste can, but nonetheless, it was vomitus. And there’d been no abdominal cramping or diarrhea.
Nevertheless, Dr. Denier says, “These scenarios can be very similar in real life and even a doctor cannot always tell the difference right away.
“A bad gall bladder episode can look just like a heart attack! Any concerning symptoms should always be reported to your doctor.”
Vomiting from anxiety is uncommon. Don’t confuse anxiety with viewing a stomach-turning scene—anxiety is not the same as being “grossed out.”
I’m talking about anxiety from job stress, an unhealthy relationship, worrying about debt—just the classic chronic anxiety.
Vomiting from Unstable Angina
“Vomiting related to unstable angina is caused by stimulation of the autonomic nervous system,” begins Dr. Denier.
“In unstable angina, there is a severe blockage of blood flow to the heart. The heart is starved of oxygen and it is under stress because of that.
“When the body or parts of the body are under stress, the autonomic nervous system is triggered. This can result in vomiting, sweating and clammy skin.”
My mother had quintuple bypass surgery three days after mysteriously upchucking the goop; not the typical volume of vomitus that you’d see from bad food.
It was morning, prior to breakfast, and she hadn’t had that much food the previous day.
Dr. Denier says, “Unstable angina is a sign of an impending heart attack.” Three doctors told me that my mother would likely have a massive heart attack within a week without the bypass.
“In some cases, sweating and vomiting may be more significant symptoms than chest pain,” adds Dr. Denier.
“In fact, some patients have no chest pain at all. That is why unexplained vomiting should be taken seriously.” Even if the person has anxiety.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Left Side Chest Pain When Exhaling: Possible Causes

A cardiologist explains possible causes of left side chest pain when exhaling.
“Left sided chest pain that occurs with exhaling only is very rare,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“Usually pain that is related to inflammation of the lining of the heart or lungs (pericarditis or pleurisy) will occur with inspiration (inhaling), but it can happen with both (inhaling and exhaling) because it is worsened by any movement of the lining.”
Of course, pleurisy, which is inflammation of the lining of the lung, wouldn’t cause left side chest pain only when exhaling — but rather, both exhaling and inhaling.
“Asthma is a condition where exhaling can become difficult and there may be a sensation of pain on exhaling,” says Dr. Denier.
“Other things to consider are pulmonary embolism (blood clot), rib fracture, pneumonia [which can be only on the left side], spontaneous collapse of the lung or shingles (herpes zoster).”
A pulmonary embolism is likely to also present with difficulty breathing.
Risk Factors for a Blood Clot in the Lung (Pulmonary Embolism)
Prolonged Bed Rest
———
Recent Orthopedic or Abdominal Surgery
———
Pregnancy
———
Birth Control Pill Use
———
Obesity
———
Smoking
———
Recent Long Trip in an Airplane
If your rib is fractured, you’ll likely recall getting hit there or taking a hard fall.
If you’re healthy and fit, it’s not likely that your lung has suddenly collapsed, and shingles usually comes with additional symptoms.
Nevertheless, these above conditions can cause left side chest pain with each exhalation.
Can left sided chest pain only upon exhaling be related to heart disease?

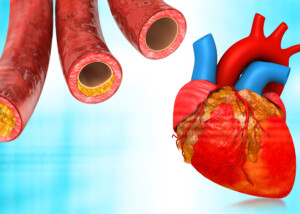
Plaque buildup in artery. Shutterstock/Explode
“This type of pain (only on exhaling) is not likely to be from coronary artery disease because angina is not related to respiration but is more likely to be influenced by exertion,” explains Dr. Denier.
“Even though the heart is located slightly to the left side, pain related to the heart is most often substernal or right under the sternum, the bone in the middle of your chest.
“Heart pain can be on the left however, and heart pain that is associated with breathing is usually inflammatory in nature and called pericarditis.”
I’ve had left side chest “pain” upon only exhalation more than once, and it correlated to my gym workouts (I suspect involvement of the pectoralis fascia).
The “pain” was more like an ache, but was quite noticeable.
The last time this happened, I could make it disappear if I leaned forward in my chair — even a hard exhalation couldn’t bring it out.
But if I sat back in the chair and exhaled, it was there. By late evening, it was completely gone.
Chest pain from coronary heart disease is not influenced by a change of position or, as Dr. Denier says, respiration.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Korawat photo shoot
Can Angina Last for Only Seconds?

Here’s what a cardiologist says about that sudden chest pain that lasts only seconds: angina or is this somehow related to your heart?
Any kind of pain or ache in the heart area (“beneath” the breasts or “behind” the breastbone) can be frightening.
Angina is chest pain that results from a shortage of blood flow in the heart, which means an insufficient oxygen supply — and hence, pain.
“A flicker of chest pain, especially if it happens at rest, is not likely to be angina,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System.
“Anginal chest pain is related to a lack of blood flow to the heart muscle.
“It usually occurs when the demand for oxygen-rich blood to the heart is greater than the supply.
“This type of chest pain typically occurs when a person is performing some type of physical activity or is under extreme emotional stress.
“The pain will come on when the demand on the heart is present and will go away when the activity is stopped.”
Dr. Denier points out that if someone who has angina over-exerts themselves, thus evoking the pain in the chest, they may immediately cease the offending activity, causing the pain to promptly go away — so in that case, the angina was brief.
“Most brief chest pains are not angina but other causes such as gastrointestinal or musculoskeletal pains. All chest pains should be reported to your doctor.”
Can angina last for five seconds?
“Five seconds of chest pain, especially if it happens randomly or at rest, is not likely to be angina,” says Dr. Denier. She says the same goes for 10 seconds: not likely to be.
Possible causes of chest pain that comes on suddenly and lasts only seconds:
- Motility of fecal matter through the large colon
- Skeletal muscle spasm
- Nerve pain caused by muscles stressed from a recent weight workout
- Acid reflux
- Esophageal spasm
What about unstable angina? Can that last only seconds?
“No, unstable angina is not likely to last for only seconds. Pain that is very brief like that is not likely to be caused by the heart,” explains Dr. Denier.

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.