Can a Blood Test Tell if You Had a Heart Attack?
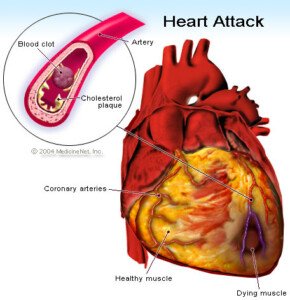
A simple and highly sensitive blood test can detect if you just suffered a heart attack–and this test is so super sensitive that it can detect even a mild heart attack.
The blood test is for an enzymatic protein called troponin. The troponin blood test for heart attack is highly sensitive and is considered the gold standard for determining damage to cardiac muscle.
“Cardiac enzymes are chemicals contained within heart cells,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
“Normally, they are essentially undetectable in the bloodstream,” continues Hanifin.
“When a person suffers a heart attack, cells in the heart die and rupture, releasing these enzymes into the blood where they can be detected.
“Diagnosis of a heart attack (myocardial infarction) is usually based upon the detection of elevated levels of these chemicals in the blood.”
If you go into an emergency room complaining of current or recent chest pain, the doctor or physician assistant will order a blood draw to check your troponin levels.
“So if a patient goes to the emergency department with chest pain and their cardiac enzymes tests are negative, are they in the clear? Not necessarily,” says Hanifin.
“It takes some time for cardiac enzymes to appear in the blood. If a patient is tested in the early stages of a heart attack, it is very possible that their levels will be within normal ranges.”
However, an elevated troponin level alone should not be used to outright diagnose heart attack.
Conditions other than heart attack can result in elevated troponin such as chronic heart failure , atrial fibrillation, kidney failure and a blood clot in a lung.
It’s never elevated by accident. As mentioned, this blood test is super sensitive.
So if the troponin is elevated, something has happened or is going on.
Chest Pain in the ER
The marvel of this blood test is that it can detect a heart attack that occurred more than a day previous, since troponin levels remain elevated in the blood for that long.
It can stay elevated for one to two weeks.
If you present with chest pain or a complaint of recent chest pain, a nurse will promptly take a blood sample.
Results may be in within 30 minutes.
Patients with chest pain and other worrisome symptoms may be told that the first test result is “normal.”
This is NOT a good time to leave the emergency room.
“A single negative test provides little useful information aside from establishing a baseline level,” says Hanifin.
“If the patient is held in the emergency department and several tests are drawn and compared over the course of several hours, a much more confident diagnosis can be made.
“If the levels remain steady, there is less grounds for concern. If the levels are rising – even within the range considered ‘normal’ – further investigation is warranted.”
Troponin takes a while to elevate if you’ve had a heart attack, so the second blood draw will be taken at least four hours later.
Depending on that result, a third one will be taken at least four hours later.
Hanifin explains, “The take-home message for both providers and patients is fairly simple.
“A positive test can be great at ruling a disease in, but one must be extremely cautious in assuming a negative test rules something out.”
 Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Catheter Angiogram vs. CT Angiogram for Heart Disease Detection

So which is better for diagnosing heart disease: CT angiogram or a catheter angiogram, which is invasive and carries big risks?
Are you aware of the less-invasive procedure of CT angiography to obtain images of blocked arteries in your heart?
The CT angiography also goes by the name computed tomography angiography (CTA).
It’s not as expensive as the invasive angiogram, the latter requiring catheterization (tubes) inserted into your body — beginning at the groin and threaded through the blood vessels leading into your heart.
Angiography via catheter carries the same risks as major surgery, including blood clots, cardiac arrest and infection.
A CT angiograph, however, does not pose these risks, and according to a study done at Thomas Jefferson University, the CT angiography is a good alternative for people who had a cardiac stress test (usually done with a treadmill) indicating coronary artery disease — but also have below a 50 percent chance of having significant blockage.
Why would a person undergo a cardiac stress test in the first place?
Some people, upon reaching a milestone age such as 50, will undergo this procedure simply to see if their heart is healthy.
Others will be spurred by a family member’s recent heart attack or, perhaps, a stent placement after the family member complained of symptoms.
And while others will get the test ordered due to complaints of symptoms such as chest pain and shortness of breath upon mild exertion.
In either group of patients — those without symptoms and those with symptoms — a positive stress test (showing blockages in the arteries) — a referral is often given for a cardiac catheterization.
The TJU study showed that even for patients with chest pain, the CT angiogram was a viable alternative that could effectively triage those patients.
What exactly is a CT angiogram?

CT (“CAT”) scan. Shutterstock/Tyler Olson
“CT angiogram is preferable, as it is a non-invasive test, particularly for patients who are likely to be NOT requiring stents or need to be treated with medications only,” says Asim Cheema, MD, who’s board certified in internal medicine, cardiovascular diseases and interventional cardiology by the American Board of Internal Medicine. Dr. Cheema is with Your Doctors Online, an online doctor chat site.
The CT angiogram involves lying in the CT scanner, after being injected with a contrast dye to show images of the coronary arteries.
The test is painless but does come with radiation exposure from the CT scanner.
This is something the patient will have to speak to his or her doctor about, as far as any increase in the risk of a future cancer development.
Nevertheless, the CT angiogram does not pose any immediate life-threatening risk such as a stroke, heart attack or infection — though a life-threatening allergic reaction to the dye can happen in very rare cases.
Amount of Radiation
The amount of radiation received from one CAT exam is the equivalent of about the same amount of “background” radiation a person receives over a time period of eight months to three years.
Background radiation comes from naturally occurring radioactive materials. CAT scans are not recommended for pregnant women.
Possible Side Effects
Though a life-threatening allergic reaction to the contrast dye is rare, less serious complications can occur, such as nausea, flushing and itching.
Kidney damage can also result. People with the following conditions may not qualify for a CT angiography:
- Kidney problems
- Diabetes
- Pre-existing allergy to contrast dye
- Weight of over 300 pounds (some X-ray tables do not support this load).
This all sounds scary, but here are possible complications of the angiogram (cardiac catheterization), but note that they are rare:
- Heart attack
- Stroke
- Injury to the catheterized artery
- Injury to the heart
- Excessive bleeding
- Blood clots
- Kidney damage
- Allergic reaction to the dye (yes, a dye is used for this procedure too).
- X-ray exposure should also be considered.
The biggest risk of all, however, is having extensive blockage in your arteries (coronary artery disease), and delaying getting an accurate diagnosis.
If a cardiologist recommends that you need a catheter angiogram, there’s a very good reason for this, as the CT angiogram is NOT the gold standard for identifying the details of heart disease. Only the catheter procedure is.

Your Doctors Online offers a free 7 day trial where you can ask a doctor questions online and get answers in minutes from anywhere 24/7. Learn more here. Dr. Cheema teaches and provides supervision to graduate students at the Institute of Medical Sciences, University of Toronto.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/MAD.vertise
Sources: sciencedaily.com/releases/2010/04/100421162617.htm; radiologyinfo.org/en/info.cfm?pg=bodyct#part_nine
How to Extend Lifespan After a Transient Ischemic Attack

There are simple ways that you can lengthen your lifespan after suffering from a transient ischemic attack (TIA).
A TIA is linked to a shorter life span, but specific steps will increase one’s life span.
Research says that a mini stroke (aka TIA or transient ischemic attack) can shorten a person’s life span – by up to 20 percent over a nine-year period.
A TIA in and of itself does not shorten life span.
Rather, it is an indicator or marker of things about the patient that can shorten life span.
You can’t die from a TIA (but you can die from a stroke). However, a TIA means a high risk of stroke and increased risk of future issues that may reduce life expectancy, says the paper which appears in the journal Stroke: Journal of the American Heart Association.
Dr. Melina Gattellari’s study recommends that doctors very closely help TIA patients manage their lifestyle for many years after the mini stroke.
- Quit smoking.
- Lose excess weight.
- Eat fewer processed foods and more fruits, vegetables and nuts.
- Exercise

And therein lies the problem, because only one of these recommendations is straightforward and not open to misinterpretation: that of quitting smoking: You either smoke or you don’t.
But just what does “exercise daily” mean?
Many people, including those who have suffered a transient ischemic attack, believe they “exercise daily” or get “plenty of exercise.”
You do not have a built-in, ready-made exercise program just because you clean the kitchen every day, shop three times a week, vacuum once a week, walk your dog or use your staircase strictly for transportation eight times a day.
You’ve ALREADY been doing these things. Post-TIA, you need to bump things up a notch.

Freepik.com/pressfoto
“After a TIA, and after controlling blood pressure and any other medical risk factors to prevent further TIAs, exercise is definitely important,” says Danielle DonDiego, DO, a family physician and obesity specialist with SteadyMD, an online program where patients can call, text or video chat with their doctor anytime.
“Exercise can keep blood pressure lower and help with circulation.”
Exercise should not be incidental; it should be “dedicated,” says Dr. DonDiego.
“As far as what type, in my opinion it’s whatever the person enjoys doing and will do, and progresses from there. I’m a big fan of resistance training for overall disease prevention and longevity.”
“Regular exercise” is that which does not include the movement of daily living that you were already doing prior to the TIA.
For example, the walking you do while shopping — slow, leisurely, laden with pauses — cannot be equated with a brisk, non-interrupted, arm-pumping walk at a park, track or residential area.
High blood pressure is a risk factor for mini stroke. Aerobic exercise, strength training and yoga will lower resting or baseline blood pressure.

The TIA patient needs to work out hard enough to produce a training effect.
Going through the motions is not enough.
“Regular exercise” means making the effort challenging — outside your comfort zone, yet not straining or painful in any way.

Shutterstock/Liderina
What You Eat
If you’ve had a mini stroke and believe you eat healthy, read the ingredients of your foods.
Avoid anything that says “hydrogenated” in the ingredients, regardless of what the front of the package says!
The FDA allows food companies to get away with labeling the front package with “Zero Trans Fats,” even though the product contains trans fats (disguised by the terms “hydrogenated” or “shortening”).
Learn the names of synthetic food additives, then stop eating products containing them, along with foods containing artificial flavors, dyes and added sugars.
It’s difficult to avoid added sugars (they are ubiquitous), but it’s easier than you think to avoid foods with synthetic chemicals and trans fats.
Healthy eating means focusing mostly on plant-derived foods with minimal processing.
Dismal Study Result
At the conclusion (nine-year mark) of Dr. Gattellari’s study, the survival rate of TIA patients came to 20 percent lower than expected.
The risks faced by one who had a TIA go well beyond the early stroke risk.
So many people who had a transient ischemic attack lose weight, stick to better eating and take up exercise in the few months following the event — only to begin letting their guard down after several months.
And then they’re back to their pre-TIA routine. They are playing Russian roulette.
 Dr. DonDiego focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
Dr. DonDiego focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Source: sciencedaily.com/releases/2011/11/111110191946.htm
Is it Safe to Exercise After a TIA (Transient Ischemic Attack)?
If you’ve had a TIA and have not been treated for it, it’s actually very UNSAFE to exercise, says John M. Kennedy, MD.
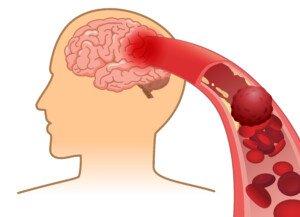
A TIA (transient ischemic attack) is actually a “mini stroke,” or to put it another way, a temporary stroke, and that high blood pressure is a major risk factor for stroke.
Exercise, especially lifting weights, raises blood pressure. Simply adding two plus two spells potential catastrophe if a person who just had a TIA (“just” could mean weeks ago) goes out and exercises.
“I would say exercise (aerobic or strength training) is unsafe for anyone who has experienced symptoms consistent with a TIA before formal evaluation by a health care professional,” says John M. Kennedy, MD, medical director of preventative cardiology and wellness at Marina del Rey Hospital, and author of the book, “THE 15-MINUTE HEART CURE: The Natural Way to Release Stress And Heal Your Heart In Just Minutes A Day.”
Though a TIA, in and of itself, doesn’t cause permanent damage, it is a very serious issue because it signals a possible impending stroke.
Ischemic stroke blood clot. Shutterstock/solar22
A TIA involves a blood clot in the brain that temporarily prevents oxygenated blood from nourishing the part of the brain that the blocked vessel supplies.
Having a transient ischemic attack means that the blood vessels in your brain have a propensity to develop blood clots.
The next blood clot could end up staying there (a stroke) rather than dissolving (a TIA).
It is a health hazard to exercise right after having a TIA.
If you believe you’ve had a TIA, do not exercise, as this will raise blood pressure. Instead, get a full medical evaluation to find out if you had a transient ischemic attack.
Symptoms of a transient ischemic attack are identical to those of a stroke and come on suddenly:
– Tingling, weakness, numbness or heaviness on one side of the body
– Visual impairment: blurriness or darkness; sudden loss of vision in one eye
– Slurred speech or difficulty speaking
– Paralysis on one side of the body
– Alarming headache
– Cognitive impairment; confusion
– Dizziness, loss of balance, difficulty walking
– Suddenly falling with no warning
Symptoms may resolve within minutes to up to 24 hours.
You may feel perfectly fine after symptoms of a transient ischemic attack resolve.
DO NOT LET THIS FOOL YOU ! By definition, a TIA is transient, so of course you’ll feel fine afterwards!
But the next blood clot could be a stroke, which can kill you or leave you permanently crippled.

If you believe you had a TIA, don’t exercise before you find out if you indeed had a transient ischemic attack.
Dr. Kennedy explains: “TIAs are signs of a threatening ‘full blown’ stroke. Two possible causes include hypertension (high blood pressure) and certain arrhythmias such as atrial fibrillation (AF), both of which can be triggered by or exacerbated by exercise.
“After a stroke, data suggests in order to achieve the best quality of life, and greatest functional capacity, walking is the best type of exercise.”
If you suspect you had TIA, don’t delay; head straight to the ER for tests, and do not exercise or perform any challenging physical activity like carrying out heavy garbage before heading out to the ER.
 Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
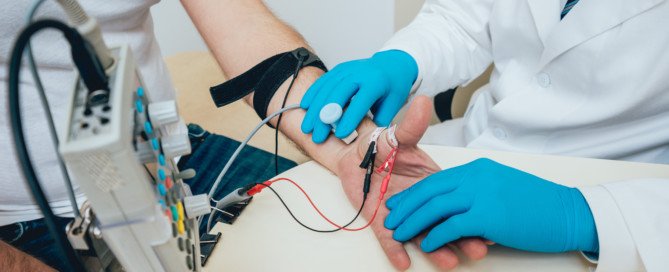
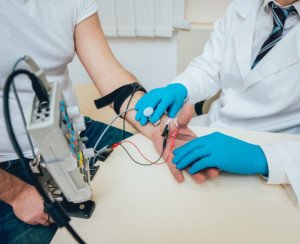
Does an EMG Test Hurt?

An EMG test can actually hurt.
It depends on how sensitive a person is to pain, and in the case of an EMG test, the pain can come from two sources: an electric shock delivered by the doctor, and needle pricks, which can take the form of an embedded needle that the doctor maneuvers around while it’s beneath the skin.
I sat in on my mother’s EMG test for her suspected pronator teres syndrome.
The doctor had warned her the day before, “It will be unpleasant.” The needles are a little thicker than acupuncture needles, said the doctor.
An electric shock is always an unpleasant experience, and there will be times that the doctor will increase the voltage.
I was watching my mother’s face while he applied the shock with a cell-phone-sized device that he’d press a button on for a split second.
She was lying on her back, eyes closed, while he worked on her arms. Her eyes would mildly flinch, and sometimes flinched more noticeably. Sometimes her face twitched from the discomfort.
However, in my mother’s case, most of the hurt from the EMG came from the needles.
The doctor would place a needle on her skin, then tap the top of it. At one point he embedded a needle about a quarter inch into her skin on the underside of the palm, and moved it around.
The most painful needle prick was when it was applied to my mother’s left palm, even though the doctor had tested her right palm first. She let out a good yalp when this happened.
How much an EMG test will hurt will depend upon where the needles are being applied, and how tolerant an individual is of this kind of pain.
I’d imagine that if they were concentrated on the upper legs, they wouldn’t hurt as bad.
I think what would hurt most during an EMG test is the patient’s anticipation of what the diagnosis might be.
I’d venture to say that the needle pricking of an EMG test doesn’t hurt nearly as much as the “pricking” that occurs during the extractions that come with facials.
Extractions on the nose hurt to high heaven (I’ve had them done). However, these don’t hurt nearly as much as sclerotherapy on the nose, which I have also had.
If you’ve had facial extractions, and especially sclerotherapy (at least on the nose), then the needle pricking of an EMG test certainly won’t hurt too much in comparison.
The bigger issue for some people, as far as pain during an EMG test, will be the electric shocks.
The electric currents last a split second, but EMG literature warns that these are not pretty.
Most people will find that at least some components of an EMG test will hurt, but you must realize that in order to find out what’s wrong with you (or not wrong with you), the EMG test is going to have to hurt.
Despite the pain or discomfort, this neurological testing procedure is perfectly safe, and my mother’s doctor said that a person can have an EMG test “all day long and it won’t harm them.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Roman Zaiets
Chronic Subdural Hematoma: How Long to Heal

How long does it take for chronic subdural hematoma to resolve completely?
Chronic subdural hematoma refers to gradual, slow bleeding in the brain that can be caused from getting hit in the head, but how long does it take for this condition to completely resolve?
This varies. My mother experienced chronic subdural hematoma.
Usually, chronic subdural hematoma is born when a person gets hit in the head, or bumps their head, but the risk is much higher in the elderly, especially if they’re on blood thinners.
My mother was on two blood thinners at the time she fell in the bathroom and hit her head on the bathtub.
The first symptom of this accident, other than the visible wound that I saw soon after I helped her to her bed after the fall, was a debilitating headache and lower body weakness … six weeks after she fell.
That day she was diagnosed with chronic subdural hematoma.
Nine and a half weeks later, the neurosurgeon declared my mother completely clear of the chronic subdural hematoma.
The CAT scan of her head was clean, normal, and she was discharged from his care.
This doesn’t mean that it typically takes nine weeks for a chronic subdural hematoma to resolve.
In the case of my mother, there is strong reason to believe that a second fall caused a setback.
One need not strike their head to cause a chronic subdural hematoma, or create a setback in a healing cSDH.
If a fall or sudden motion (such as riding in a car in which the driver slams on the breaks) causes a jarring motion of the head in an elderly person, this can shake things up with the brain’s blood vessels.
And if there’s already a tear in a vein that caused a chronic subdural hematoma, than this jarring can cause more tearing, and hence, more bleeding.
My mother had a recurrence of the cSDH; the symptoms of this began about 10 days after the burr hole draining of the first chronic subdural hematoma.
The neurosurgeon was not able to rule out that her second fall (in which she did not hit her head, but jarred it) didn’t cause the recurrence, even though recurrence happens about 15 percent of the time after drainage.
If a chronic subdual hematoma produces symptoms, it will almost always require surgical draining.
The neurosurgeon will then “follow” the condition with CAT scans.

CT scanner. Liz West, Boxborough, MA, CC Wikimedia Commons
The CAT scan will show how much blood and cerebral spinal fluid is still in the brain, and how old the blood is.
Over time, follow-up CAT scans should show a diminishing amount of blood.
The surgical draining will not get rid of 100 percent of the blood, but is designed to get rid of enough to:
1) relieve symptoms, and 2) promote the healing process, which is the body resorbing the fluid and the veins healing.
While a patient is healing from chronic subdural hematoma, blood thinners will be off limits, and the patient must take vigilant precautions to avoid hitting their head or experiencing any jarring motions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Photographee.eu
Carpal Tunnel Syndrome Causes Cold Hands and Pain

Carpal tunnel syndrome can cause hands to feel cold, and it can also cause discomfort in the hands and even forearms.
In fact, the symptom of cold hands can precede any symptoms of actual pain or aching.
“Very few patients have significant pain,” says Dr. John T. Knight, MD, an L.A.-based hand and wrist orthopedic surgeon and director of the Hand and Wrist Institute at the D.I.S.C. Sports and Spine Center. He continues, “The most common symptoms are tingling, numbness, and aching discomfort.”
However, it’s not uncommon for carpal tunnel syndrome to awaken somebody in the middle of the night by causing pain.
This is because during sleep, a person may take on certain body positions that are conducive to putting the wrist in a flexed position, that is, bent so that the angle between the palm and underside of the forearm is decreased.
Sometimes the angle of wrist flexion can be close to 100 degrees, while the person is fast asleep, unaware that this wrist flexion is putting pressure on the median nerve.
Pressure on the median nerve is what causes carpal tunnel symptoms.

Carpal tunnel syndrome. Scientific Animations
It is along this nerve, which begins at the neck, that electrochemical signals travel that allow your thumb and fingers (except pinky) to move, as well as to feel.
In carpal tunnel syndrome, the median nerve is pressed upon at the wrist by a band of ligamentous tissue.
This nerve compression interrupts the signals coming from the brain for movement, or coming from the receptor neurons in the fingers for touch and feel, hence, why classic symptoms of carpal tunnel syndrome are tingling, numbness and weakness involving the fingers and hand.
Cold hands can be a symptom of carpal tunnel syndrome as well.
Dr. Knight explains, “Coldness in the hands is similar to tingling and is due to the pressure on the nerve and temporary decrease in circulation loss to the nerve.”
Surgery to correct carpal tunnel syndrome is recommended when conservative treatments (e.g., wrist splinting, cortisone injections, hand exercises) have failed.
Traditionally, surgery involves an incision about an inch long, stitches, and bulky restrictive bandages that must be worn for 2-3 weeks after surgery, and rehabilitation can take up to three months.
Dr. Knight specializes in stitchless endoscopic carpal tunnel release, which involves only a 1 cm incision, no stitches, much less surgical pain, and a much faster recovery time.
 Dr. Knight is widely regarded as one of the most prominent hand and wrist specialists in the U.S., specializing in minimally invasive techniques for hand, wrist and upper extremity injuries and disorders.
Dr. Knight is widely regarded as one of the most prominent hand and wrist specialists in the U.S., specializing in minimally invasive techniques for hand, wrist and upper extremity injuries and disorders.
 Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
sscpywrt26
Can Stress Cause a TIA (Transient Ischemic Attack)?

Stress absolutely can trigger a TIA, or transient ischemic attack, says John M. Kennedy, MD, medical director of preventative cardiology and wellness at Marina del Rey Hospital.
So if you’re at risk for a TIA, and especially if you’ve had a TIA, you’d better practice stress management.
“Stress comes in two varieties, acute or chronic,” says Dr. Kennedy, author of the book, THE 15-MINUTE HEART CURE: The Natural Way to Release Stress And Heal Your Heart In Just Minutes A Day.”
Acute stress is sudden in onset, like that experienced in a natural disaster, a heated argument or car crash.
Chronic stress is consistent, day in and day out, unrelenting stress like that experienced in a difficult relationship or a hostile work environment.
“Both forms of stress, whether acute or chronic, lead to a release of hormones, adrenaline and cortisol, which cause physiologic changes,” says Dr. Kennedy.
And once you get a TIA, or transient ischemic attack, you are at prime risk for a future stroke. In fact, the TIA can be a warning of an imminent stroke.
The physiologic changes that occur from stress, that can give rise to a TIA, are:
- Increased inflammation
- Increased heart rate
- Increased blood pressure
- Thick, sticky blood, “All of which create the perfect storm for a cardiac event, TIA or stroke by damaging the delicate inner lining of blood vessels,” says Dr. Kennedy.
Though there are people who have recovered completely from a stroke, or have had only a “minor” stroke, don’t let this comfort you.
About 750,000 people in the U.S. every year suffer a stroke, so certainly, out of this enormous statistic, there will always be some lucky people.
However, nearly 60 percent of stroke victims suffer permanent walking disability, and stroke is America’s leading cause of disability, and third leading cause of death by disease.
So if you’ve had a TIA, learning to manage your stress levels can save your life.
If you believe you’ve had a TIA, then get a complete evaluation as soon as possible.
In fact, a competent medical insurance plan will cover an ER visit for a transient ischemic attack if you come in that same day.
A TIA is a medical emergency, even though the symptoms may last only a few minutes and be mild.
“Additionally, acute and chronic stress can trigger an arrhythmia (abnormal heart rhythm) known as atrial fibrillation (AF), which causes the upper chambers of the heart to quiver, causing blood to become stagnant and prone to forming a clot,” says Dr. Kennedy.
“If the blood clot becomes dislodged and released into the bloodstream, it can travel to the brain and obstruct blood flow, causing TIA or stroke.”
In conclusion, stress really CAN kill, and stress can definitely cause a TIA.
 Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
sscpywrt26
Can EMG Test Miss an ALS Diagnosis?
Can electromyography be done too early to detect amyotrophic lateral sclerosis?
People fearful they have ALS may wonder if their EMG test missed it because it was done too early; the EMG test results came out normal, but then, you still think you have ALS and begin doubting the EMG’s accuracy in detecting this fatal neurological disease.
Every 90 minutes in America, someone is diagnosed with amyotrophic lateral sclerosis, and death typically occurs 2-5 years after diagnosis, usually due to respiratory failure.
To find out if an EMG test can be done too early to diagnose ALS and thus miss it, I posed this question to Daniel Kantor, MD, director of the Neurology Residency Program, Florida Atlantic University.
Dr. Kantor responded: “There are two questions here. Can an EMG be normal in a patient who eventually gets diagnosed with ALS, and can an early abnormal EMG in an ALS patient be misinterpreted as another disease process. The answer to both, is, unfortunately, yes.”
The first of these two questions mentioned above simply means that you can go in for an EMG test that turns out normal — because you don’t have ALS.
But by sheer coincidence, at some point down the road, you happen to develop this untreatable neurological disorder, and sooner or later you’ll be going in for a second electromyography, due to the new symptoms.
This is akin to a woman going in for a mammogram that doesn’t detect breast cancer – because she doesn’t have it. But five years later, a mammogram shows a suspicious mass.
The second question is that a person with ALS has an EMG, and the results are misinterpreted for another condition. But the scenario doesn’t end here.
Dr. Kantor adds: “A person with ALS may have a normal EMG years before they become symptomatic, so theoretically an EMG early in the course of their ALS may appear normal (or mostly normal).”
So I then asked Dr. Kantor: What if they have the electromyography at the time they actually start having early symptoms?
Assume that’s why they’d have the test in the first place; they’re having peculiar symptoms; at this point, then, could the EMG still “miss” the ALS and still show normal readings?
Dr. Kantor says, “Actually, no test is 100 percent, even x-rays. So, theoretically (but not likely), an EMG could fail to detect the typical ALS changes because the electrical signals are below the sensitivity of the machine.
Other problems may cause an EMG picture similar to ALS, and ALS may be misdiagnosed as another problem.
Also, please remember that an EMG, like any test, is not 100 percent and is very operator dependent.”
Dr. Kantor is also President Emeritus, Florida Society of Neurology.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Roman Zaiets
What Is the Best Painkiller for Carpal Tunnel Syndrome ?

The pain of carpal tunnel syndrome isn’t the same kind of hurt that comes from injured cartilage, tendons or arthritic joints, so you need a painkiller that targets the specific problem of CTS.
Carpal tunnel syndrome and painkillers can go hand in hand (no pun intended).
If you have carpal tunnel syndrome, you may have already tried a number of painkillers to alleviate the discomfort, only to find that nothing really works.
As to what painkiller you should take for carpal tunnel syndrome, I asked Dr. John T. Knight, MD, an L.A.-based hand and wrist orthopedic surgeon and director of the Hand and Wrist Institute at the D.I.S.C. Sports and Spine Center. Dr. Knight specializes in the stitchless endoscopic carpal tunnel release, which takes only 10 minutes.
If your carpal tunnel syndrome necessitates painkillers that aren’t even working, then it’s wise to consider the next step.
Says Dr. Knight: “If severe carpal tunnel syndrome is present, surgery is usually indicated as soon as possible.

Carpal tunnel syndrome. Scientific Animations
“If there is significant pain not relieved with over-the-counter NSAID’s such as Advil or Aleve and possibly a cortisone injection, then a mild narcotic such as Darvocet may be helpful.
“No narcotics should be used more than a week or two, as they are habit forming, and if the pain is severe enough to require this type of medication, then surgery should be expedited.”
In addition to the kind of discomfort that can make you seek out narcotic painkillers, carpal tunnel syndrome typically presents with numbness and tingling in all the fingers except the pinky; and sometimes finger/hand stiffness and weakness.
Conservative treatment for this nerve compression disorder involves wearing a wrist splint while sleeping to prevent wrist flexion, which compresses the median nerve, the nerve at the center of carpal tunnel syndrome.
If you are reaching for narcotic or prescription painkillers, or perhaps any painkillers to subdue carpal tunnel pain, it’s time to seek out a surgical solution.
The more invasive, “open” procedure requires stitches, and results in longer recovery time than Dr. Knight’s stitchless endoscopy.
Until you have surgery, what kind of painkillers should you take for carpal tunnel discomfort, if narcotics can be habit forming over such a short period of time?
Dr. Knight explains that there is “no set time table; each person is different; the more they use, the greater the chance of addiction, and if the problem is correctable with surgery, then best to do soon if narcotics are necessary, but usually not an issue, as pain is not usually very bad.”