Do Thoracic Aortic Aneurysms Have a Genetic Cause?
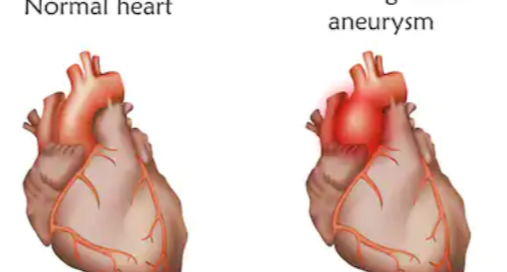
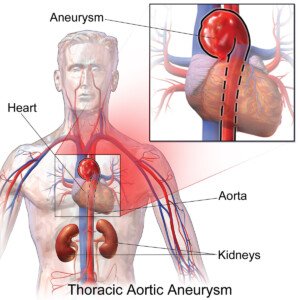
A thoracic aortic aneurysm is a bulge in this great blood vessel that can kill a person within minutes if it rips open.
A genetic basis for a thoracic aortic aneurysm has been the subject of research.
Research (Nature Genetics, Milewics et al) revealed an association between a common genetic variant and a possible predisposition to an acute aortic dissection (AAD).
The genetic variant’s presence may double one’s risk of developing AAD.
The vast majority of people who suffer an acute aortic dissection have a pre-existing aortic aneurysm, which typically grows over time but usually produces no symptoms.
Genetic Variant Discovered Linked to Thoracic Aortic Aneurysm
The genetic variant is on chromosome 15, discovered by researchers (Milewicz et al), and the study report was published in 2014.
The gene involved is called FBN1. It has already been established that mutations in FBN1 cause Marfan’s syndrome, which predisposes patients to aortic aneurysms and hence, AAD.
Marfan’s syndrome. The thinness in Marfan’s is not caused by an eating disorder. Mileny ES Colovati1, Luciana RJ da Silva1, Sylvia S Takeno1, Tatiane I Mancini1, Ana R N Dutra1,Roberta S Guilherme1, Cláudia B de Mello2, Maria I Melaragno1and Ana B A Perez1/Wikimedia Commons
“Although patients with aortic dissection in our study did not have Marfan syndrome, this study suggests that the same pathways are involved in causing aortic dissections in patients with and without Marfan syndrome,” says the 2011 paper.
“Genetic cause for aortic aneurysm have been known but poorly understood,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“There appears to be familial aneurysm disease, but the gene that is causing it has been elusive.
“The one that is known is the aneurysms associated with Marfan’s syndrome.
“That gene has been identified on chromosome 15 and is related to the entire syndrome (tall, slender, hyperflexible joints, aortic aneurysm/dissection propensity).
“The abdominal and cerebral aneurysms remain a work in progress to find the genes.
“Various studies have shown that if a first-degree relative has an abdominal aortic aneurysm, you are 2-4x more likely to have one than someone without that family history.”
Marfan’s syndrome can go undiagnosed because its symptoms are often subtle and vary in severity.
Mild signs, such as joint hypermobility or eye problems, may be overlooked or mistaken for other conditions.
The most serious complications, like cardiovascular issues involving the aorta, can remain unnoticed until later stages.
Extra tall and thin kids or teens with long limbs or hypermobile joints should be evaluated for Marfan’s syndrome, as these traits are common in the disorder.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Veronika Zakharova
Source: sciencedaily.com/releases/2011/09/110911145257.htm
Stent Graft Repair of Aortic Aneurysm Eliminates Open Heart Surgery

Stent graft repair of thoracic aortic aneurysms is becoming more and more commonplace, replacing the riskier open heart surgery.
Open chest surgery for treating a thoracic aortic aneurysm is highly invasive, can take up to eight hours, and months to recover from.
There can also be serious complications such as kidney injury.
So is there any way to treat aortic aneurysm without cutting open the chest?
Yes, there is. It is called the stent graft.
A stent graft can repair this serious condition, and patients usually go home after one or two days, versus the one to two weeks required for the open chest surgery.
- The stent graft is a polyester tube that is covered with metal webbing.
- The surgeon uses a catheter, or thin tube, to deliver the stent graft, via the patient’s groin in an artery.
- The catheter is guided into the chest artery: the thoracic aorta.
- At the predetermined location, the stent graft is deployed, and it expands to the arterial walls.
- The stent graft can range from 1-2 inches wide, to 4-8 inches long.
“Stent grafts have grown in popularity and have become quite sophisticated,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Most thoracic aortic aneurysms can be treated with a TEVAR (thoracic endovascular aortic repair),” continues Dr. Fiocco.
“The vast majority of TAA beyond the aortic arch are treated this way (beyond the left subclavian artery).
“The aortic arch, where the arteries to the arms and brain arise from the aorta, is much more of a challenge for TEVAR, and is a quite complex open surgery for aneurysm as well.
“Treatment of the TAA in the ascending aorta with TEVAR is still in its early development due to the need to avoid the coronary arteries at one end and the aortic arch with its branches at the other.”
Silent Killer
It is estimated that about 60,000 Americans have a thoracic aortic aneurysm: an abnormally dilated aortic vessel.
There are usually no symptoms, and they are normally discovered incidentally via imaging tests for other concerns such as suspected pneumonia.
Treatment at that point depends on the size of the aortic aneurysm.
Depending on the size, the treatment will include that of regular imaging tests to track the growth rate of the artery’s bulging portion.
If it reaches a certain size, usually 5.5 cm, or if the growth exceeds a certain rate per year, or if there are symptoms like chest pain and shortness of breath, surgery will be discussed.
Otherwise, the watchful-eye approach is used, along with lifestyle modifications including no smoking, and blood pressure control.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Build Muscle Safely with Aortic Aneurysm: Hundreds Training

If you have a thoracic aortic aneurysm and are crushed at hearing “avoid lifting weights,” there is hope: Hundreds training, for building muscle.
If you’ve been diagnosed with a thoracic aortic aneurysm, your doctor may have warned you not to lift weights.
This all-encompassing restriction for those with a thoracic aortic aneurysm ensures that there will never be a blood pressure spike from any heavy lifting.
Thoracic aortic aneurysm and building muscle can be in the same sentence with “hundreds training.”
Chances are pretty high that your doctor is not aware of a weightlifting format called “hundreds training.”
Hundreds training is ideal for people who, due to medical conditions (including thoracic aortic aneurysm), cannot or should not lift heavy weights.
Can it be safe, then, for people with a thoracic aortic aneurysm to lift weights?
According to the International Registry of Acute Aortic Dissections website:
For patients who are very much interested in maintaining some sort of weight lifting program, choosing sets of repetitive light weights appears to make more sense than permitting heavy weight lifting.
Hundreds training can actually build lean muscle tissue. If you have an aortic aneurysm and, in the past, strained with heavy weights in the name of building muscle or shaping your body, you can still achieve these results – with hundreds training.
Granted, if you want to place in a bodybuilding contest, you’re going to need a lot more than the hundreds training protocol.
- But this isn’t about getting the look of a bodybuilder.
- It’s about increasing lean muscle mass — which of course, always results in a better looking and fitter body.
Hundreds training will not bulk you up or make you look like a powerhouse.

Shutterstock/wavebreakmedia
But assuming that you want to lift weights to have a sleek, muscular look, hundreds training should work very well for you, and will not contraindicate a thoracic aortic aneurysm.
The “How to” of Hundreds Training
The basic premise of hundreds training is to use a load that is 20 to 30 percent of your 8-12 rep max effort.
The rule of “don’t lift weights” for people with aortic aneurysm assumes that any strength training they do would cause a big spike in blood pressure.
Hundreds training won’t cause a major spike in blood pressure because 20-30 percent of your 8-12 rep max is not heavy enough.
Example: Shoulder Press
Let’s use the shoulder press machine as an example. With a load that’s 20-30 percent of 8-12 rep max, push it up 50 times.

Shutterstock/CandyBox Images
This may not be possible; you might make it only to 40. Just lift the weight till you can’t anymore.
This muscle failure will not spike blood pressure, even though it will hurt like mad.
People with a thoracic aortic aneurysm should never hold their breath while lifting weights, and should always exhale on the push or pull phase.
However many reps you complete for this first attempt, subtract that from 100, and that’s how many seconds you rest till you resume.
If you completed 45 reps, you rest 55 seconds, then see how many more you can do, which will certainly be less than 45.
Let’s say it’s 25. So now, you’ve completed 70 reps thus far. This means you rest 30 seconds (100 minus 70 equals 30).
Go again. Each time you have to stop, whatever number of reps you have left, is the number of seconds you rest.
By the time you’re done your muscles will be pumped like never before, and the “pain” will be searing.
This is a safe way to lift weights for people with aortic aneurysm, because the resistance doesn’t require the straining that doctors warn against.
Muscle burn is not the same as straining, and comes from lactic acid buildup, which results from many reps. Rest five to seven minutes in between hundreds routines.
Three sessions per week (45 minutes each) will provide a superb, safe weightlifting workout for people with a thoracic aortic aneurysm who wish to build muscle.
Before embarking on this regimen, you should explain it to your cardiologist.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik
Source: iradonline.org/articles/lifestyle_recs.html
Lift Weights Safely with Aortic Aneurysm; Burn Fat with Panaerobics
For people with a thoracic aortic aneurysm, there’s a weightlifting modality that can burn fat & tone muscle: panaerobics.
What’s the Risk of Aortic Aneurysm in a Bicuspid Heart Valve?
An aortic aneurysm is more likely to occur in someone who was born with a bicuspid aortic valve (BAV).
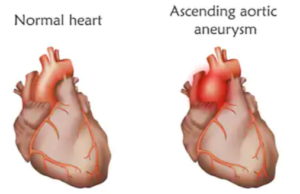
“The aorta is the large artery carrying oxygenated blood away from the heart,” explains Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
Dr. Beatty continues, “It climbs upwards out of the left ventricle (the ascending aorta) into the aortic arch where it curves downwards into the descending aorta.”
The aorta is the body’s biggest blood vessel.
“Arteries supplying blood to the heart muscle, brain, arms, kidneys and bowel branch off at various levels,” adds Dr. Beatty.
****
An investigation looked at the frequency of aortic aneurysm (and dissection) in people with BAV.
The data that was analyzed was of patients diagnosed with bicuspid valve, spanning 1980 to 1999; they were residents of Olmsted County, Minn.
Also analyzed was data involving people with aortic disease whose BAV had gone undiagnosed.
The last year of follow-up was 2008-2009. Included were 416 people with bicuspid valve; average follow-up was 16 years.
Risk of aortic aneurysm development in people with bicuspid valve: 26 percent over a 25-year period.
What does this translate to when compared to the general population? An 86 times greater risk of developing an aortic aneurysm.
What about risk of dissection in those with bicuspid valve? After all, an aortic aneurysm is a precursor to a dissection (size of aneurysm is directly proportional to risk of dissection).
People with bicuspid valve had an 8.4 times higher risk of dissection than people in the region’s general population.
This number may seem high, but the study authors state that the absolute risk of dissection still remains low in people with bicuspid valve.
Say the study authors: “The low aortic dissection incidence and lack of association with a detectable reduction in survival is reassuring.” The full report is in the Sept. 14, 2011 JAMA.
What else did this study unveil? Incidence of dissection was greater in people over age 50, and not surprisingly, higher in patients who had a baseline aortic aneurysm.
Percentage of people with BAV: 1-2 percent
Symptoms of bicuspid aortic valve: Not all patients have symptoms, and in some cases, one may live a normal life span minus BAV problems.
How BAV is usually discovered: Incidentally during a routine physical, or an imaging test for an unrelated condition.
Symptoms are a heart murmur (not always present) and rapid changes in blood pressure during stress or activity.
Complications: aortic aneurysm as well as dissection; leakage of blood back into the heart; narrowing of the valve, which can lead to a thickened, inefficient heart; mitral valve leakage.
If you’ve been diagnosed with a bicuspid valve, it’s very important to have it monitored on a regular basis for the possible development of an aortic aneurysm.
 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: BruceBlaus/CreativeCommons
2011/09/110913161941.htm
http://www.cedars-sinai.edu/Patients/Health-Conditions/Bicuspid-Aortic-Disease.aspx
http://en.wikipedia.org/wiki/Arnold_schwarzenegger#Accidents_and_injuries
Lifting Weights with Aortic Aneurysm: “Straining” Defined

For those with thoracic aortic aneurysm, the restriction of “No straining” when lifting weights needs to be explained.
If you’ve been diagnosed with a thoracic aortic aneurysm and have always lifted weights, you’re likely wondering how to recognize that fuzzy boundary between a challenging workout and a “straining” workout.
Sometimes, straining is obvious, as in the case of a man barely getting a barbell off the floor in a deadlift, his back buckling, legs quivering, face turning red, and it seemingly takes him forever to straighten his back.
But straining doesn’t always look like this, either.
Lifting weights doesn’t have to be straining, so here are guidelines for distinguishing between straining and not straining.
There are five basic levels of lifting weights: 1) Going Through the Motions, 2) Some Work, 3) Challenging, 4) Difficult, and 5) Straining.
What’s the difference between Difficult and Straining?
- It’s not determined by amount of weight lifted.
- It’s determined by amount of effort.
One person’s straining load can be another person’s warm-up lift. As a former personal trainer, I’ve had clients straining with weight loads that others moved with little effort.
Signs of Straining
- Vocalizing or feeling like vocalizing
- Squirming or other substantial form breaks
- Grimacing
- Moving the load slowly because it’s so heavy, especially with pauses.
- Valsava maneuver
“Valsalva is what we do when lifting something very heavy and when we are bearing down to have a bowel movement,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals..
Now, if you are not grunting, moaning or groaning, this does not mean you can’t be in the Straining zone.
The key is if you feel compelled to grunt or groan. You may be avoiding this simply out of courtesy to nearby people, but if you actually feel like doing it, then you’re straining — at least somewhat – a forbidden zone for thoracic aortic aneurysm.
What does Challenging mean?
A Challenging set of eight bench presses means that the tempo is a little slowed down at the seventh or eighth rep due to increasing fatigue, but you feel you can do another eight. You stop at only eight.

Turn the Challenging bench press into a Difficult set by lifting the same weight, but for 12 reps.
You stop at 12, but know you can do three or four more. Your arms “feel it,” but you aren’t “whupped” yet.
To make this a Straining set, add more weight so that you must struggle to complete four or five reps.
Form breaks are tempting at this stage, namely, arching the back. Or perhaps one arm is lagging behind the other and you’re gritting your teeth and scrunching up your eyes.
Often, an eight-rep max will make a person feel they must strain — depending on the move. Certainly, you’ll feel much more straining for an 8-RM deadlift, squat or bench press vs. a dumbbell curl.
BruceBlaus/CreativeCommons
Recap
Going Through the Motions: This is like warming up.
Some Work: Think of this as more than a warm-up, or what you might do when recovering from a mild injury.
Challenging: Minimal heart rate elevation; no or minimal increase in respiration; yet you feel worked.
Textbook form, and solid, rhythmic breathing are maintained throughout, but you also induced a little muscle burn.
The lifts can be done quickly with full range of motion. You could have done the 12 reps with 25 percent more weight. You made it look easy to the observer.
Difficult: You can do fast lifts at the beginning, but quickly find you can no longer go fast.
You must pay more attention to breathing to avoid any breaks in breathing, but form is intact. No desire to grunt, groan, moan or grimace.
But the weight did get heavy. By the time you think you’re closing in on the Straining zone, the set is over. Heart rate is up, but nothing significant. An observer knows you definitely were not warming up.
Straining: To the observer, and to yourself, you are struggling. The lifts are laborious and slow, and unsteady if it’s with dumbbells.
You must concentrate on breathing to avoid pauses in breathing. There may be eventual form breaks, such as arching your back while bench pressing.
If you’re not grunting or moaning, it’s out of courtesy to others. Your face shows “pain.” At the conclusion, you know you kicked some bad butt.
Lifting Weights with a Thoracic Aortic Aneurysm

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com/ pressfoto
Think You Have Lymphoma? Blood Pathology Questions to Ask

What questions should you ask regarding blood pathology if you might have lymphoma?
Lymphoma is cancer of the lymph nodes, and if this disease is suspected by your physician, then your blood will need to be analyzed.
If you or your doctor suspect lymphoma or leukemia, your blood will need to be scrutinized by a pathologist. A blood pathologist is called a hematopathologist.
If your doctor informs you that your samples need to be sent to a hematopathologist, here are some questions you should ask about this process, according to Dr. Zsuzsanna Vegh-Goyarts, assistant director of the Flow Cytometry department at Acupath Laboratories, a leading anatomic pathology and cancer genetics laboratory.
Questions to ask blood pathologist if you might have lymphoma or leukemia:
Who will evaluate the specimen? Can I speak to the blood pathologist?
The blood pathologist does not have direct contact with the patient. “Your doctor will send your samples, along with your clinical history, to a laboratory to process and test,” says Dr. Vegh-Goyarts.
What happens to specimen when it reaches the lab? The sample is processed, measured, tested, analyzed by licensed lab technologists.
A blood pathologist will carefully examine results, then construct a report and diagnosis. Your doctor will receive a final diagnostic report.
What is a biopsy? A biopsy means removing a sample of cells, fluid or tissue for analysis. Ask what kinds of tests will be done.
Most frequently, a blood pathologist will test for CBC (complete blood count), red and white blood cell count, hematocrit, platelet count, red blood cell volume, concentration of hemoglobin, and differential blood count. What if CBC results are abnormal? Further testing is warranted.
What can I learn from these tests? Results can determine diagnosis of lymphoma, leukemia and other diseases.
How fast will I get the test results? Your doctor normally gets results within 24 hours, though a specialty test may require several days. Your doctor should then immediately contact you.
Dr. Vegh-Goyarts explains, “It is important that your doctor sends samples to an experienced hematopathologist within an established and accredited diagnostics laboratory in order to receive the most accurate results, and ultimately allowing for the best patient care.
“On the other hand the hematologist relies on the clinical data from the patient’s physician to establish a diagnosis.
“Laboratory data are always viewed in the light of all the clinical background and all test results.
“Physician and hematopathologist often discuss the case before the final conclusion is reached regarding the diagnosis.”
Blood diseases affect hundreds of thousands of people in the United States every year, according to the Leukemia and Lymphoma Society.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Viktoriia Hnatiuk
Source: www.acupath.com
Why Does Being Fat Raise the Risk of Uterine Cancer ?

Being fat increases the risk of uterine cancer, plain and simple.
DNA mutations that lead to uterine cancer do NOT care if you love your larger-than-life body or hate it.
Fat is a risk factor for uterine cancer, and the only way around this is to lose weight. Learning to “love your skin” will not nullify this well-established risk factor.
Obesity or being “fat” and good health should never be in the same sentence, unless it’s to say that obesity and good health cannot co-exist in the same body.
So it’s no surprise that a fat body is a risk factor for uterine cancer.

ParentingPatch, CreativeCommons
“The adipose tissue or fat tissue in obese patients has an enzyme called aromatase that can convert other hormones in the body to a weak estrogen,” says Diane Yamada, MD, Chief, Gynecologic Oncology, University of Chicago Medical Center.
In essence, the patient is getting significantly more estrogen than the ovaries would normally produce.
This constant, higher level of estrogen is not counteracted by progesterone.
It may stimulate the lining of the uterine cavity (the endometrium) to develop precancerous change, and then cancer.”
In other words, the more lifetime exposure that a woman has to circulating estrogen, the higher her chances of developing the malignancy.
Of course, this risk is her baseline risk, and the baseline varies from one woman to the next.
Genetics may play a part, and genetics cannot be changed. However, obesity is primarily linked to lifestyle habits.
Uterine cancer is also known as endometrial cancer, and some risk factors are tied to the exposure to estrogen.
You now know how a lot of excess fat in the body influences the risk for uterine cancer. But here are other factors tied to estrogen:
Many years of menstruation (beginning before age 12, and/or late menopause).
The more monthly cycles a woman has, the more her uterus is exposed to estrogen.
Which is why never having been pregnant, and even having just one pregnancy, is another risk factor for this disease. However, researchers aren’t sure why this increases risk for the condition.
It may be because pregnancy increases levels of progesterone, which offset the effects of estrogen.
According to the American Cancer Society, obese women have triple the risk of uterine cancer, and overweight women have double the chance.
But if you’re medium weight or even skinny, don’t think this makes you immune to this disease! Thin women can get it, too.
A high fat diet is another risk factor for uterine cancer, not just because it promotes obesity, but because some fatty foods may influence estrogen metabolism.
Keep in mind that a non-overweight woman can still have a high fat diet.
The fats at issue here are the so-called “bad” fats: the saturated and trans (manmade) variety, found in animal products and processed foods (e.g., commercially baked goods), respectively.
Other risk factors for uterine cancer are estrogen-only hormone replacement therapy, tamoxifen for breast cancer, ovarian tumors and diabetes.
Non-obese women with diabetes actually have an increased risk of uterine cancer. The majority of cases occur in women over the age of 55.
It’s never too late to lose weight, and food intake has everthing to do with obesity.
 Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Yves Picq, CC BY-SA
Why Do Spouses of Bedridden Obese Overfeed Them?

What about the enablers of super morbidly obese bedridden people: spouses or family members who keep feeding them tons of food?
Have you seen any of those TV shows about 700, 800, even 900 pound men and women who literally live out of their beds, while a family member (usually a spouse) continues to bring them enormous quantities of food?
These are popular shows, and in so many cases is the mind-boggling enabler.
Usually, the “caretaker” enabler is a spouse, but sometimes it’s a significant other, or family members such as older children or even a niece.
In the case of 800 pound Billy Robbins, the enabler was his mother!

Billy Robbins
What causes enabling behavior towards the super morbidly obese who can’t leave their bed to get food?
For this article I interviewed two medical doctors: an obesity specialist and an addiction specialist.
“Enabling is a complex psychological behavior with multiple etiologies,” says Michael Nusbaum, MD, founder of Nusbaum Medical Centers of New Jersey which specializes in weight loss treatments.
Dr. Nusbaum says that the enabler typically functions out of a “warped sense of love.”
Enablers of the super morbidly obese have ulterior motives, he says, including that of “creating a situation where the patient is physically unable to leave them,” and making that person “undesirable to others.”
Dr. Nusbaum also explains that an enabler may be “compensating for a perceived failure to nurture in the past.”
This last explanation to a small degree explains why Billy Robbins, who at age 18 weighed over 800 pounds, was enabled by his mother.
But wanting to re-create a deceased baby does not explain why a woman brings 20,000 calories a day to her 900 pound husband, or why 960 pound Renee Williams’ daughters kept bringing her food.
Enablers Keep Bringing Huge Amounts of Food to Obese Who Can’t Get Out of Bed
“The person who enables the food addict or compulsive eater supplies food for the same reasons a loved-one buys more alcohol for a nearly unconscious alcoholic or lends money to a drug addict knowing it’ll be spent on drugs,” explains David Sack, MD, a psychiatrist specializing in addiction disorders, and CEO of Promises Treatment Centers in Malibu and Los Angeles.
Yes, “Who keeps feeding them?!” is a fair question when super morbidly obese individuals can’t even leave their bed.
TV programs almost always show the food source as their spouses, family members or significant others, rather than pizza or other food delivery workers coming into their bedrooms.
Dr. Sack says that often, enablers think they’re helping their overfed loved-one.
“They want to show their unconditional love and acceptance for the obese individual or make them happy, even if just for a moment.
“Providing ‘help’ gives them some sense of control in an unmanageable situation.”
Kenneth Brumley, confined to bed at over 1,000 pounds, admits to eating 30,000 calories a day — catered to him by girlfriend Serena.
But what’s going on with Serena and other enablers like her?
“Some are in denial about the problem,” says Dr. Sack. “Others are codependent: Their self-esteem depends on their ability to help others, even if the help actually hurts.
“Once someone begins enabling, it can be difficult to break the cycle.
“The addictive behavior continues or worsens and the enabler gets drawn in further.”
Many enablers, he continues, avoid the task of correcting the problem to avoid conflict or because they’ve learned to feel helpless.
“Over time, the enabler loses their identity outside of their caretaking role,” says Dr. Sack.
Imagine how much time every day Serena must expend making sure Brumley gets his food.
Imagine how much time Cheryl must have invested feeding her husband Ricky Naputi (now deceased) enough food daily to keep him at around 900 pounds.
A man at Brumley’s house commented that outside the garage, he could smell the stench: like “one huge baby diaper.”
Brumley hadn’t bathed in four years. How could Serena enable this?
Dr. Sack points out that solving the problem involves a lot more than just, for instance, Serena one day announcing, “Kenny, from this point forward, I’m bringing you only 2,000 calories a day. If food delivery comes to the house, I’m not letting them in. Complain all you want. I’m no longer your enabler.”
The solution, says Dr. Sack, often “requires the entire family to see a mental health professional to address the underlying issues.”
One of the comments to an online New York Daily News article about Ricky Naputi is as follows:
So basically he couldn’t move and she had complete power over what he would eat. I think she basically murdered him.
 Dr. Nusbaum is a bariatric surgeon, board certified by the American Board of Surgery, and a Fellow and member of the American Collage of Surgeons.
Dr. Nusbaum is a bariatric surgeon, board certified by the American Board of Surgery, and a Fellow and member of the American Collage of Surgeons.
 Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Sources:
dailymail.co.uk/news/article-505198/The-half-ton-mum-Tragic-story-worlds-heaviest-woman.html
nydailynews.com/life-style/health/world-fattest-man-died-900-pounds-article-1.1353829
Enablers of the Super Morbidly Obese Partly to Blame for Overfeeding

What is it with the spouses of bedridden super morbidly obese people who keep bringing them trays of food?
Being addicted to excessive amounts of eating is no excuse for bringing to the food addict, who weighs over 600 pounds and is bedridden, heaps and heaps of junky sugary items.
A study from the University of Georgia reveals that the behavior that drives a person to gorge abundantly on food is the same kind of impulsive behavior behind substance abuse. This is referred to as a compulsive personality.
But the difference between alcohol/drug addiction and that of food is that the former individual can easily ambulate to get the next fix.
A super morbidly obese person who’s confined to bed cannot do this.
Someone else supplies the food, prepares it, brings it to the bedside.
This is the enabler, and is almost always a spouse or significant other.
The journal Appetite (2014) has the University of Georgia report explaining that those with impulsive personalities are more apt to report greater levels of food addiction. This was associated with obesity.
“My lab generally studies alcohol, nicotine and other forms of drug addiction,” says James MacKillop in the paper, principal investigator of the study.
He continues, “…but we think it’s possible to think about impulsivity, food addiction and obesity using some of the same techniques.”
Have you ever noticed that those bedbound, super morbidly obese people on reality TV shows such as “My 600 Pound Life” and “Half-Ton Dad” never live alone?
That’s because it takes two people to create this horrendous situation: the food addict and the enabler. Sometimes there’s more than one enabler.
There’s growing research in the realm of food addiction, and significant research into the causes of obesity.
But where’s the research into what compels a person to become an enabler and help their loved-one kill themselves with food?
This is like bringing alcohol to a person with liver cirrhosis, or cigarettes to a person with lung cancer. Who’d ever do that?
But here we have all these enablers being depicted on reality TV shows bringing piles of fast food to their 600, 700, sometimes over 800-pound spouse or family member! This is mind-blowing.
And nobody seems to want to address it head-on. The enabling issue gets evaded on TLC’s shows, time and time again.
The only exception to this evasion is the “Half Ton Teen” show, in which the enabler dynamic to the 800 pound young man is explored.
MacKillop hopes that his research will guide physicians and other relevant experts in planning treatments and interventions for the food-addicted super morbidly obese.
However, what about their enablers, in cases where the obese are bedridden or housebound?
This is akin to an alcoholic struggling to abstain, while an enabler keeps bringing this person alcohol every time the addict expresses a desire for liquor.
In addiction, brain circuits are “hijacked,” says MacKillop, laying “the foundation for compulsive eating habits that are similar to drug addiction.”
But this doesn’t mean that those with compulsive behaviors will necessarily become obese, he adds.
Though most enablers to 600 pound individuals are obese themselves, some are not. Thus, the idea of “sharing” an addiction does not seem to apply in all the cases.