Feel Like Passing Out While Exercising? Here’s Why
You can solve the problem of passing out while exercising once you know what’s causing it, & this may include heart problems or diabetes which can creep up on a person.
I was a personal trainer for five years at a major health club, and I can recall two clients who nearly passed out while exercising. (more…)
Exercises that May Be Harmful to Obese and Overweight People

There’s two reasons that an overweight or obese man or woman should avoid particular exercises.
There are exercises that personal trainers actually have their obese clients doing.
These are exercises that people of very large size should NEVER be doing!
There are two issues at play here.
The first reason concerns safety and risk of injury.
The second reason concerns worthlessness of the exercise. (more…)
Is It Safe for Children to Lift Weights?

It’s actually safer for kids to lift weights than it is for them to do many things their parents permit them to do. (more…)
What Is Steady State Cardio & Some Examples?

You’ve probably come across the term steady state cardio many times in reading about exercise and fat burning. (more…)
9 Exercises to Reduce Calf Cramps & Strengthen Calves

Weight training exercises for calves should be part of any man’s or woman’s exercise program.
Calf muscles can be prone to muscle pain that can send you through the roof. (more…)
Most Over Diagnosed Diseases Include Bipolar and Alzheimer’s
Don’t panic yet if you or a loved-one have been diagnosed with bipolar or Alzheimer’s, as these are among the most over-diagnosed conditions, says Dr. Jacob Teitelbaum.
Strength Training Moves You Can Do with Rotator Cuff Problem
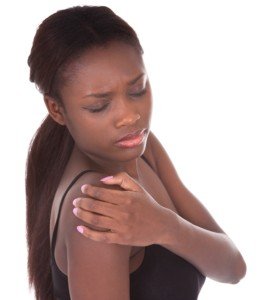
What are the best kinds of strength training routines for people with rotator cuff pain?
You have more options that you believe.
There are many weightlifting moves that you can do despite having a problem with your rotator cuff.
Your strength training options are not as limited as you think.
I’m a former personal trainer who has had rotator cuff problems in the past.
These tendon problems come in varying degrees, sometimes requiring surgery.
But for rotator cuff issues that don’t require surgery, but rather, patience and the right exercises, you can still do plenty of strength training.
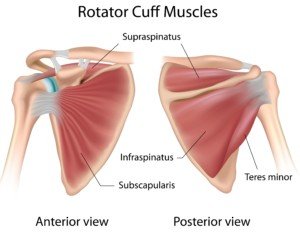
Shutterstock/Alila Medical Media
Best Strength Training Exercises for a Tricky Rotator Cuff
Rowing motions tend to least aggravate a bad RC tendon.
This is why a person with a painful rotator cuff — upon bench pressing, doing pushups or shoulder presses — will still be able to knock off heavy seated rows, at least if the grip isn’t wide, as well as more-narrow-grip chin-ups and even possibly pull-ups.
A wide grip, however, will likely cause problems.
Bent-over dumbbell rows are a good strength training exercise that tends to spare pain in a troublesome rotator cuff. Just keep the arm close to your side; do not flare it out.

Bent-over barbell rows with a supinated (palms facing outward) grip are sometimes another nice strength training exercise for people with rotator cuff pain.
Face the palms inward, however, and you may feel pain.
The “corner” or prone row is also a good exercise for those whose rotator cuff area pipes up during pressing movements. Note: A wide grip is not recommended. Use a narrow grip.

Shutterstock/martvisionlk
Another good strength training routine that’s very friendly to the rotator cuff is shoulder shrugs: dumbbells, plates, Smith machine, tension bands.

Other strength training moves that someone with rotator cuff pain can do:
1) Narrow grip lat pull-downs; avoid a wide grip.
A supinated grip works best, followed by a neutral grip (choose the appropriate handles).
2) Any kind of biceps curling motion may be friendly towards a finicky rotator cuff.

Shuttersock/Nicholas Piccillo
Other kinds of shoulder injuries, however, can become aggravated with biceps curls.
So proceed with heightened awareness.
When my RC problem was flared up, I could still do heavy dumbbell curls.

3) Some triceps routines may be compatible with rotator cuff issues.
But stay away from dips! Triceps push-downs with the rope may be your best bet, compared to other isolating-triceps strength routines.

Need I say that the worst strength training routines for painful rotator cuffs involve chest pressing motions, shoulder pressing motions.
And perhaps the worst offenders: behind-neck military press, upright row and dumbbell lateral lift. These are nasty for strained RC tendons.
Interestingly, lateral lifts, when done with super light weight and straight arms, can actually help restore the rotator cuff.
So can chest pressing motions with dumbbells – very light dumbbells, that is.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Andrey_Popov
Tone the Back of Your Flabby Upper Arms with One Exercise

One exercise will tone the back of your upper arms.
Having trouble toning the back of your upper arms?
Ladies, I have a great exercise for you that will really tone and tighten the flab in the back of your upper arms.
Get Rid of Love Handles with Three Types of Workouts

What are the best exercises for replacing unsightly love handles with a tight trim waist?
If you hate your love handles, I have exercises that will get rid of them.
You don’t need to do any waist exercises to get rid of those awful love handles. (more…)
Should Beginners in Strength Training Do Barbell Squats?

If you’re new to lifting weights, don’t let this stop you from doing the barbell squat, one of the best strength training exercises around.
When I was a personal trainer I had my clients–who’d never before lifted weights–learning to do the barbell squat.
But not before I carefully “screened” them for compatibility with this compound, fat burning exercise.
- In general beginners are good to go with the barbell squat, as long as they understand proper, safe form.
- Many beginners and even more experienced people have poor form.
The squat targets the glutes, upper legs, lower back and abdominals, and can be a major component of a fat burning workout regimen.

Shutterstock/Oleksandr Zamuruiev
Should beginners dive right into a free-barbell squat or first start out with the Smith machine?
This has a two-pronged answer. If you’re just not meant to do free-barbell squats, you can benefit from the Smith machine.

Freepik.com, senivpetro
On the other hand if your body is better proportioned for the free-barbell squat, and you don’t have issues with your spinal column such as stenosis, you can begin with a very light bar — once you feel comfortable doing bodyweight squats.
Some beginners are able to just jump right in and start squatting the Olympic bar (45 pounds).
Rushing into making it heavier, though, will put the beginner at risk for pulling a muscle.
The reason novices need to be careful with the barbell squat free across their upper back is because often, the unsuspecting person will round their lower back.
This increases risk of low back injury.
The novice must also make sure their feet are aligned, not uneven, and that their body is not leaning more to one side while conducting the movement.
One of my clients was a 60-year-old, obese woman who was very lost with her body positioning when just trying to squat the bar — on the Smith machine!
So this is where a case-by-case basis applies. This client did well on the leg press; she was no weakling; but her mind and body just could not connect when it came to even a Smith machine squat.
She’s an exception. There are plenty of older women and men who take to the free-barbell squat — with proper instruction.
Beginner’s Rules for a Safe Barbell Squat
- Keep feet flat on floor, at least shoulder width apart.
- Keep an arch in your lower back.
- Keep head tilted up a little, your eyes straight ahead or slightly upward.
- Keep the chest “puffed out.” Aim to get your thighs parallel to the floor. Past parallel is okay but not necessary when you’re a beginner.
Beginners can start out with a rep range of eight to 12. Rest a few minutes and repeat. Increase weight load with reason over time.
Don’t get ahead of yourself and start piling on plates; you can end up with a lower back strain or pulled area where the hamstring ties into the glute muscle.
Just because few beginners are ever seen at the squat “rack” or “cage” doesn’t mean that this fat burning exercise is reserved only for the experienced.