Does Zero Calcium Score Always Mean Clear Arteries?
If your calcium score is ZERO, how confident should you feel about not having heart disease, and having nice clean arteries?
Did you recently get your coronary calcium score measured and it was zero, but you’re wondering if this absolutely for SURE means you have crystal clear arteries?
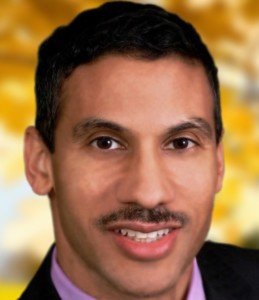
“It may not mean totally clear arteries,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“There may be some very mild plaques that are essentially clinically insignificant and are not calcified enough to be detected on the calcium score,” continues Dr. Sayeed. “Technically it does mean clear arteries in the big scheme.”
How to Help Prevent Clogging of Your Coronary Arteries
So if you are concerned that you may still have some mild heart disease or not perfectly clear arteries despite having a coronary calcium score of zero, there are several things you can do to dramatically reduce the risk of eventually developing significant levels of coronary heart disease.
AVOID TRANS FATS AT ALL COSTS.
While consuming trans fats a few times a month might not seem harmful, it’s crucial to ensure that this frequency doesn’t escalate to a few times a week.
Even occasional consumption can add up over time, leading to significant trans fat intake over a decade.
Since there is no definitive data on the long-term risks associated with occasional trans fat consumption, it’s prudent to err on the side of caution.
To protect your health, it’s best to avoid trans fats altogether and focus on a diet rich in healthier fats, such as those from nuts, seeds and fish.
LIMIT PROCESSED FOODS (even if they don’t contain trans fats) as much as you can.
Make a homemade chicken pot pie; forget Marie Callender’s.
To limit processed foods, focus on preparing fresh, whole foods at home.
Choose fruits, vegetables, lean proteins and whole grains. Read ingredient labels carefully to avoid hidden sugars, unhealthy fats and additives.
Plan meals ahead of time and cook in batches to reduce the temptation of convenience foods.
Gradually replace processed snacks with healthier alternatives like nuts, yogurt and fresh fruit.
Replace bottled juice with whole fruit.
There are numerous other ways to protect against developing coronary artery plaque buildup and maintaining clean arteries and keeping your calcium score at zero.
These include taking the supplements of green tea extract, turmeric, garlic and krill oil, and eating omega-3-rich fish several times a week.
Fish offers numerous benefits, including reducing inflammation, improving heart health by lowering blood pressure and cholesterol levels, supporting brain function and enhancing joint health.
It can also contribute to better mood and cognitive function.
And finally, DO HIGH INTENSITY INTERVAL TRAINING.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
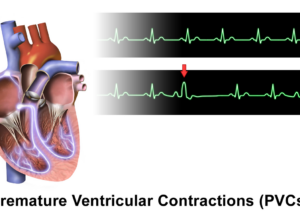
Why Does Anxiety Cause Premature Ventricular Contractions?

Anxiety can cause PVCs (premature ventricular contractions), especially if you have anxiety over PVCs.
But just how does this happen; what is the mechanism?
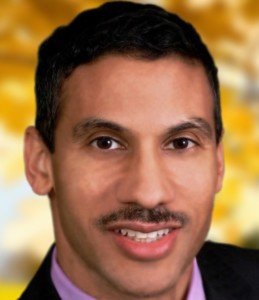
“Anxiety causes increased stimulation of beta receptors on the heart, which can cause increased heart rate and cause other parts of the ventricle to have electrical impulse formation (PVCs) due to increased beta agonism,” explains Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
Beta receptors are located on the cells of the heart. They are part of the physiological response that occurs when a person suffers from anxiety or stress.
Beta receptors are part of the sympathetic nervous system; this is the system that causes changes in the body to prepare it for a fight or flight (e.g., heightened senses, increased respiration, rapid heart rate).
So amid these physiological changes, the ventricles of the heart may end up not quite pumping in perfect rhythm.
“Beta agonisms” simply means that the beta cells are stimulated or activated.
You can get PVCs simply by worrying about them.
Just like sometimes muscles will begin twitching when a person with health anxiety begins fretting about twitching muscles, one’s heartbeat will start feeling jumpy or like there’s an extra or skipped beat — simply due to the anxiety that comes with worrying about this.
For the typical person, the biggest problem that premature ventricular contractions present is the way they feel.
Nobody likes to feel a fluttery or erratic type of beating in their chest. This is called cardiac awareness. And it is not easily ignored.
However, PVCs are rarely a significant issue or something that a cardiologist will worry about.
PVCs can occur in healthy hearts. Most cause no symptoms, don’t impair heart function and don’t increase risk of cardiovascular issues unless they are linked to structural heart disease.
In a heart with clogged arteries, PVCs are more relevant to your cardiologist.
The duo of premature ventricular contractions and plaque buildup in the coronary arteries can mean a higher risk for irritated heart muscle, reduced heart pumping ability or the development of an arrhythmia.
Cardiologists evaluate heart flutters in the context of patient history and any co-occurring conditions.
Your doctor will be concerned with any other symptoms with the premature ventricular contractions such as shortness of breath, chest pain, undue fatigue, dizziness, nausea or fainting spells.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Y Photo Studio
Can PVCs Be Caused By Seasonal Allergies?
A cardiologist addresses whether or not premature ventricular contractions can be caused by seasonal allergies.
Many people who have PVCs want to know if seasonal allergies can cause this sometimes very disturbing symptom.
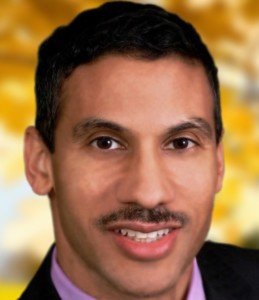
“This would be quite rare, and only if the allergies really caused a lot of stress and anxiety and excessive adrenaline release from a more severe allergy,” explains Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
PVCs can have a bark that’s bigger than their bite, which is why individuals who experience these can become quite alarmed.
Seasonal allergies are far more likely to cause headaches than premature ventricular contractions.
If you’ve been experiencing “cardiac awareness,” then you need to have a thorough checkup by a cardiologist.
They may then recommend additional testing that you’d need to make an appointment for.
Do not let all of this frighten you; multiple tests are modern medicine at work to help find the root causes of troubling symptoms.
Tests that turn out normal will give you substantial reassurance that you have a healthy heart.
PVCs may be relevant in people who have heart disease, but even then, this association has not been clearly defined by research.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can Angina Cause Vomiting?
Find out why angina can cause vomiting.
Angina is a condition in which insufficient blood flow occurs in the heart due to narrowing of the coronary arteries from disease (plaque buildup), and hallmark symptoms are chest pain and shortness of breath.
However, angina can also cause vomiting.
In fact, vomiting can signal an imminent heart attack (more on this shortly).
“Angina, especially if severe, can cause excessive stimulation of the autonomic nervous system leading to vomiting,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“The anginal vomiting would likely be accompanied by some other anginal equivalent such as excessive sweating or shortness of breath or chest pain,” continues Dr. Sayeed.
A few days before my mother was diagnosed with unstable angina, she upchucked.
That same morning she had an alarming episode of difficulty breathing.
Two days later (after being diagnosed with unstable angina) she had emergency quintuple bypass surgery and had been days away from a massive heart attack, said three doctors.
The day prior to the symptoms, she had not eaten anything unusual; why was she upchucking?
This was so unlike her. I quickly connected the dots: difficulty breathing plus vomiting, although mild — an imminent heart attack!
Usually, vomiting signals a benign cause, such as a bad food source or substantial anxiety.
Dr. Sayeed explains, “In some cases, it may be hard to differentiate from bad food or anxiety, but in general, the patient would likely have risk factors for angina or a prior history of heart disease.
Anxiety and bad food would be short-lived causes, while the vomiting from angina could occur with each episode and perhaps persist until the underlying problem was fixed.”

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/InesBazdar
Can Muscle Twitching Be Caused by Chronic Fatigue Syndrome?

A doctor answers the question, Can chronic fatigue syndrome cause twitching muscles.
“Chronic fatigue might cause muscle twitching in some people, but the mechanism is not clear,” says Dr. Moshe Lewis, MD, board certified in physical medicine and rehabilitation.
“Chronic fatigue remains controversial because, while sometimes a virus can be identified such as EBV or Lyme or Parvo immediately preceding the onset of the fatigue, in many cases such a well-defined time correlation remains elusive,” continues Dr. Lewis.
“When it comes to muscle twitches themselves there are a host of causes which include benign fasciculations, low grade seizure activity, decreased mineral levels like calcium and magnesium, amongst others.”
If you suspect that muscle twitching is, indeed, being caused by your chronic fatigue syndrome, then find out what can be causing the CFS.
Dr. Lewis cites the following possible causes: allergies such as to gluten; toxicity; mismanagement of stress; prior physical trauma; hormonal imbalance; lack of exercise; slowed metabolism; aging; side effects of medication; improper medication; and irritable bowel syndrome.
Chronic fatigue syndrome is a diagnosis of exclusion, meaning, other possible causes for one’s symptoms must first be ruled out.
There is no blood test or imaging study that shows the presence of chronic fatigue syndrome.
Because the symptoms of CFS can overlap with those of many other conditions, it’s important for doctors to rule out other possible causes of the symptoms through a series of tests. These include imaging and blood tests.
As for Twitching Muscles
As for twitching muscles, anxiety over a diagnosis of chronic fatigue syndrome can bring on anxiety that leads to harmless twitching.
Muscle twitching can be triggered by anxiety, stress or nervousness.
When someone is anxious or worried about a diagnosis like CFS, the body’s “fight or flight” response can be activated, leading to a variety of physical symptoms, including fasciculations.
This kind of twitching is generally harmless and is usually temporary.
It’s also possible for a person to have (simply by chance) both chronic fatigue syndrome and benign fasciculation syndrome.
BFS is a disorder characterized by a lot of muscle twitching — but also of cramping of the muscles and fatiguing easily from exertion.
Chronic fatigue syndrome does not cause benign fasciculation syndrome, nor vice versa.
CFS can also cause sleep disturbances, muscle and joint pain, headaches and even a sore throat.
Again, CFS is a condition of exclusion. All other possible causes for one’s troubling symptoms need to be ruled out in order for a diagnosis of CFS.
Though exercise can be problematic with both CFS and benign fasciculation syndrome, exercise also may be the very thing that will help improve symptoms of both conditions!
 Dr. Lewis is the founder and CEO of Golden Gate Institute for Physical Medicine in CA, which provides education and clinical management of pain.
Dr. Lewis is the founder and CEO of Golden Gate Institute for Physical Medicine in CA, which provides education and clinical management of pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ fizkes
Why Does Inactivity Make Back Pain WORSE?
![]()
Find out why inactivity is perhaps the worst thing you can do for low back pain.
Bed rest and inactivity are bad for low back pain, you may already know, but do you know why?
“Muscles need to move, as this is their key function in life,” says Dr. Moshe Lewis, MD, board certified in physical medicine and rehabilitation.
“Inactivity thus leads to muscles contracting and shortening because they have a decreased distance to traverse.
“While this process is slow, it can be quickly exacerbated by back pain or an injury.
“While it may seem natural to rest after an injury, this should be limited to two or three days. The longer one takes to move, the harder it is to get moving again.
“This presents a challenge however, because when there is evidence of significant tissue trauma such as fracture or disc herniation, or significant bone involvement such as spinal stenosis or spondylolisthesis, people will find several movements, if not all, very, very painful.”
Suppose, however, your back pain or ache is due simply to lack of exercise, and there is no bone or nerve involvement.
The muscles have shrunk and shortened. They are not being used the way nature designed them to be used, and quite literally, the adage of, “If you don’t use it, you’ll lose it,” applies here.
I’m a former personal trainer and, I hate to admit this, but some years ago I began noticing a persistent aching in my low back.
I’d lifted weights and had done other physical things for years, yet my low back developed a daily ache.
I ramped up my low back floor exercises; no change. I’d always done exercises for the lats and rhomboids, but obviously, these failed to prevent the development of this low back pain.
It was interfering with my hanging leg lifts. I tried massage therapy; no change.
I wondered what ELSE could I do, as far as exercise. There HAD to be something that would cure this low back ache.
Well, there was one particular exercise that I had not considered as a solution. I gave it a try, and within eight weeks, my low back discomfort was GONE.
I’ve been doing this exercise ever since, and it’s my favorite!
It’s the deadlift — and even those who are new to strength training can do this exercise — which also helps burn excess body fat.
 Dr. Lewis is the founder and CEO of Golden Gate Institute for Physical Medicine in CA, which provides education and clinical management of pain.
Dr. Lewis is the founder and CEO of Golden Gate Institute for Physical Medicine in CA, which provides education and clinical management of pain.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shuttertstock/Pixel-Shot
Causes of Calf Cramps in the Middle of the Night

Cramping in your calves overnight has a number of possible causes.
Many people have suffered from the sudden spasm of a calf muscle in the middle of the night, caused by tensing it a bit too much while stretching.
This pain is excruciating to high heaven, enough to make a grown man cry, but it is not a serious condition.
But what if the calf pain occurs in the absence of some careless stretching of a muscle that’s been stiffened by several hours of sleep?
This problem can occur even to physically fit people.
“Typically cramps in an athlete are caused by decreased circulation with oxygen after prolonged activity,” says Dr. Moshe Lewis, MD, board certified in physical medicine and rehabilitation.
“This phenomenon can also be seen in diabetics and smokers who also have poor circulation for different reasons.
“Classically these two groups of patients also have pain when they walk — called claudication.”
Claudication, often called intermittent claudication, is a sign of poor blood flow to the legs, causing pain or cramping during activity, typically walking, that resolves with rest.
What are some other causes of calf pain or cramps overnight?
Dr. Lewis says, “In the non-athlete or someone who has not had prolonged activity that day, night cramps are due to sciatica.
“When nerves get pinched or impinged, positional changes at night can cause muscles to go into spasm.
“This occurs because nerves send key information to muscles which lets them work correctly. When those signals are disrupted, muscles spasm.”
Sciatica is a pain that radiates down one leg, and it often begins in the lower back or buttocks.
It’s caused by irritation or compression of the sciatic nerve.
This nerve, the largest in the body, can be affected by various factors, including a herniated or bulging lumbar disc, and spinal stenosis (narrowing of the spinal canal).
There are still yet other variables that can cause calf pain or cramping in the middle of the night, though these other causes can also cause symptoms during the day as well.
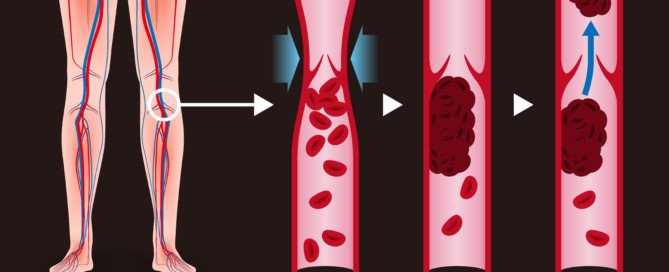
These variables are vasculitis, phlebitis, potassium deficiency and a DVT.
DVT, or deep vein thrombosis, is a blood clot that requires immediate medical attention, as it can dislodge and travel to the lungs, causing a fatal pulmonary embolism.
Risk factors for this include birth control pills, long air travel with very little movement, smoking, recent major surgery and obesity.
Another Cause of Painful Nighttime Calf Cramping
A most innocent cause, that may happen to just about anybody, is that of stretching a stiffened body upon awakening in the middle of the night.
Because one is just coming out of slumber, they’re not fully awake and hence, not alert enough to thoughtfully regulate a reflexive stretch.
The stretch is overdone, and the calf muscle gets the brunt of this, tightening up in response. The pain is excruciating.
This has happened to me, and I eventually finally came up with a solution: The moment I feel the cramp coming on, I flex my foot (moving top of foot towards shin).
This elongates the main calf muscle (gastrocnemius), opposing the tightening-up and relaxing it to its natural state: no cramp develops!
 Dr. Lewis is the founder and CEO of Golden Gate Institute for Physical Medicine in CA, which provides education and clinical management of pain.
Dr. Lewis is the founder and CEO of Golden Gate Institute for Physical Medicine in CA, which provides education and clinical management of pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Prostock-studio
How Old Is Too Old for Total Knee Replacement Surgery?

Are you getting up there in years or know someone of very old age and wondering if you can be TOO OLD for total knee replacement surgery?
This surgery is invasive and comes with notorious risks such as infection and blood clots.
Age Cutoff for Total Knee Replacement Surgery
Perhaps you’ve been wondering if there’s an age cutoff for major knee procedures such as replacement or revision (of a failed replacement).
How important is old age in the consideration of surgical candidacy for knee replacements?
“Revision surgery can be done at any age if the joint has failed and the patient’s quality of life is suffering because of it,” says orthopedic surgeon David Fisher, MD, Director of the Total Joint Center at the Indiana Orthopedic Hospital.

Ravedave, CC BY-SA
He continues, “Medical conditions do need to be under control and they require medical clearance, as this is a major surgery with potential complications.”
A person who’s considering joint replacement or revision surgery will need to get this clearance from the primary care physician.
Other conditions such as diabetes, kidney problems or congestive heart failure have a high potential for complicating the operation.
In other words, old age, in and of itself, is not a consideration for a total knee replacement.

Dronainfotech, CreativeCommons
Other things must be considered, such as if the patient has a weak heart, diabetes or kidney problems.
A person in his 70s, but who has congestive heart failure and obesity, can very easily be a much poorer candidate for total knee replacement surgery than a 92-year-old who’s at an ideal body weight and does not have congestive heart failure or any other serious medical problem — other than being slowed down and pained by osteoarthritis in the knees.
In short, you can’t be too old for total knee replacement surgery; the bigger patient picture needs to be considered.
 Dr. Fisher has been involved in research and development of total hip and knee implants and has had numerous articles published in professional journals, and has participated in many research projects.
Dr. Fisher has been involved in research and development of total hip and knee implants and has had numerous articles published in professional journals, and has participated in many research projects.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Best Ways to Prevent a DVT after Joint Replacement Surgery
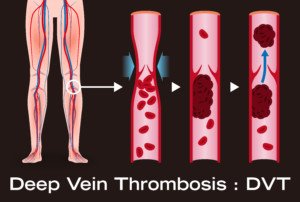
The complication of DVT following joint replacement surgery can lead to a fatal pulmonary embolism.
Therefore, the best prevention tactics for a DVT must be put into place.
Other high risk surgeries for DVT are that of pelvic and intra-abdominal, says David Fisher, MD, Director of the Total Joint Center at the Indiana Orthopedic Hospital.
“There are several options available to reduce the risk of DVT/PE including a combination of pharmacologic agents (blood thinners), sequential compression devices worn on the outside of the legs or feet, and rapid mobilization postoperatively,” says Dr. Fisher.
What the Patient Should Do Preop for DVT Prevention
If you’re planning on having joint replacement surgery, the smart thing is to ask your doctor what measures will be taken to help prevent deep vein thromboses.
Don’t just assume everything will be taken care of, and don’t think for a second that you, as the patient, don’t have the right to inquire about this.
Dr. Fisher continues, “The pharmacologic agents include Coumadin (warfarin), Lovenox (low molecular weight heparin), Arixtra, Xarelto, and actually aspirin.
These agents affect the clotting cascade at different locations and act as anticoagulants.”
These drugs, but least likely aspirin, pose the potential risk of internal bleeding, since they thin the blood.
Nevertheless, in general, they definitely do reduce risk of deep vein thromboses.
Without preventive or prophylactic measures, the risk is 45 percent, says Dr. Fisher. With preventive measures, DVT risk drops to one to two percent.
One-tenth to one-half percent of joint replacement patients develop a PE, which comes from a DVT when the blood clot breaks loose and travels to the lungs.
Sudden chest pain and difficulty breathing are the two most common symptoms of a pulmonary embolus.
Is any particular preventive measure the most effective for DVT prevention?
“It is not clear which is ‘The Best,’ as they have all been proven effective,” says Dr. Fisher.
“Many surgeons like the simplicity and safety profile of aspirin and compression stockings, but there is controversy regarding the effectiveness of that combination and lack of acceptance by the American College of Chest Surgeons and the Center for Medicare Services, making it harder for surgeons to utilize this strategy,” explains Dr. Fisher.
As mentioned, the non-aspirin blood thinners are more effective than aspirin, but do come with postoperative bleeding as a possible side effect, and this can require additional surgery to correct.
“My preference is a pharmacologic agent with compression stockings and rapid mobilization (up in a chair the same day of surgery),” says Dr. Fisher.
“We have used Coumadin, Arixtra, and currently use Xarelto with the other strategies, and have maintained a DVT rate of one percent and PE rate of 0.2 percent over the past 20 years.”
 Dr. Fisher has been involved in research and development of total hip and knee implants and has had numerous articles published in professional journals, and has participated in many research projects.
Dr. Fisher has been involved in research and development of total hip and knee implants and has had numerous articles published in professional journals, and has participated in many research projects.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/metamorworks
Failed Loosened Knee Replacement Missed by Bone Scan

Should you rely entirely on what a bone scan shows if you suspect that your total knee replacement has “loosened” or failed?
It is important to discuss this with your orthopedic surgeon.
A failed total knee replacement (TKR) can produce symptoms that are strikingly similar to those caused by other conditions such as nerve damage or spinal stenosis (narrowing of the spinal canal).
When a patient who’s had a total knee replacement presents to a doctor with complaints of knee pain, swelling, warmth and instability in walking, one consideration might be that the implants/prostheses have loosened, or have “failed.”
The doctor may then order a bone scan to see if anything suspect shows up — but how effective is this tool?
“A bone scan is a study that detects changes in bone metabolism and is nonspecific in providing results,” says orthopedic surgeon David Fisher, MD, Director of the Total Joint Center at the Indiana Orthopedic Hospital.
“Increased bone activity can be caused by trauma, infection, prosthetic loosening, metabolic bone disorder.
Failed total knees may or may not stimulate a bone response depending on the cause of failure.”
Causes of Failed Knee Replacements
• Friction. The joint surfaces rub against each other, causing wear and tear over time of the implant surface.
• Infection. Bacteria can flourish on the metal and plastic components.
• Stiffness. Reduced range of motion can result in a functional deficit.
• Instability. The patient may feel that the knee might “give way” when walking. This indicates that the soft tissue that surrounds the joint is just too weak so support body weight.
• Improperly placed implants. This can cause instability.
• Fracture. A fracture around the joint can lessen stability.
Second Opinion of Bone Scan Can Be Useful
“So a bone scan is not usually necessary to determine problems with a total knee replacement and can miss many causes,” says Dr. Fisher.
 Dr. Fisher has been involved in research and development of total hip and knee implants and has had numerous articles published in professional journals, and has participated in many research projects.
Dr. Fisher has been involved in research and development of total hip and knee implants and has had numerous articles published in professional journals, and has participated in many research projects.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.