Herniated Disc Surgery: What’s Involved
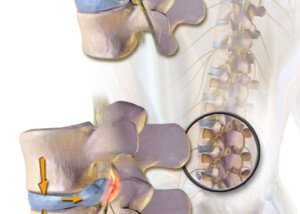
Find out what’s involved in surgery to treat a herniated (bulging) disc.
A herniated disc is common in the general population, but not all cases produce symptoms.
When symptoms do develop, they include the following:
- Pain in the lower back
- Pain that radiates down the butt and may extend down the leg
- Tingling or numbness in any of these areas
- Weakness in the leg and even the foot
There are numerous non-surgical treatments for a herniated disc. These are tried first before it becomes clear that surgery is the only option left.
These include physical therapy, stretching exercises, warm packs, cold packs, chiropractic, acupuncture, muscle relaxants, pain relievers and epidural steroid injections.
Surgery is often an anxiety-driving prospect, but when conservative treatments fail after being given a fair time trial, then a microdiscectomy is the only recourse.
Surgical Repair of a Herniated Disc
“What we’re doing is called a microdiscectomy and it takes about 45 minutes to an hour to perform,” says Dr. P. Justin Tortolani, an orthopedic surgeon and spine specialist with University of Maryland St. Joseph Medical Center.
General anesthesia is used to guarantee that the patient will not make even the slightest movement during the procedure.
“It’s accomplished through a small incision and generally, patients are discharged the same day with a two to three week recovery period. Their daily activities are restricted somewhat,” says Dr. Tortolani.
“Specifically, what is done is to create a small window opening in the spinal column and that’s called foraminotomy, and then after that the portion that is herniated is removed or excised.
“Usually we’re not touching the remainder of the disc itself and just removing the portion that is herniated.”
 Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Monkey Business Images
Causes of Chest Pain, Jaw Pressure in Middle of the Night

A cardiologist names some likely causes for chest pain and jaw pressure in the middle of the night.
The cause of pain in your chest or pressure in your jaw that awakens you in the middle of the night isn’t necessarily a heart attack.
“There are many possible causes,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
Angina As a Cause
“Cardiac causes can include coronary artery disease with rest angina, especially in those with lower heart rates at night,” says Dr. Sayeed.
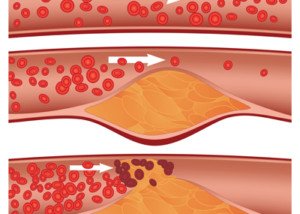
Coronary artery disease means plaque buildup in the arteries. This so-called sludge reduces blood flow through the heart.
Angina is a condition in which clogged coronary arteries lead to this reduced blood flow in the cardiac muscle, causing chest pain and/or shortness of breath.
When this occurs only upon physical exertion, exercise or highly charged emotions such as during a heated argument, it’s called stable angina. Jaw pressure may occur.
When it occurs during rest, such as during sleep or napping, it is called unstable angina. Here too, pressure in the jaw may occur.
Leaky Heart Valve As a Cause
Another cause of chest pain overnight that’s accompanied by jaw pressure is leaky valves in the heart.
An echocardiogram will detect if this is the case. Leaky valves as well can decrease cardiac blood flow.
Inflammation As a Cause
“Another cause can be pericarditis and inflammation of the sac around the heart, and pericardial effusion or fluid around the heart, which can be worse with lying down and flat, and can wake people up at night with chest pain,” explains Dr. Sayeed.
“This kind of pain can also occur in the setting of pulmonary embolus or blood clot in the lung. But the most common cause would be coronary disease with low flow as above.”

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/airdone
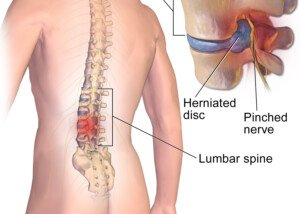
Best Exercises for a Low Back Herniated Disc
Here is what a pain specialist doctor recommends as best exercises for a herniated disc in the low back (lumbar region).
A herniated disc in the low back (lumbar spine) is very common, and also goes by the name of bulging disc.
The first line of treatment involves exercises. They are really quite simple; nothing complicated or difficult to do, no matter how “lazy” or “out of shape” you think you are.
What are the best exercises for treatment of a herniated disc in the low back?

Source: myupchar. com
The two types of exercises are Pilates and walking, says Neil B. Kirschen, MD, chief of pain management, Department of Anesthesiology at South Nassau Communities Hospital in Oceanside, New York.
If you use a treadmill do not hold on other than for momentary steadiness such as when drinking some water.
Holding on as part of your walking will disrupt natural gait patterns and will often cause poor posture.
These are the last things you need when you have a back problem.
Walking sessions done consistently strengthen the muscles that support the spine, which can alleviate pressure on the back and improve posture.
Walking encourages the release of endorphins, which are natural pain relievers.
It can also help maintain a healthy weight, reducing the strain on the back caused by excess body weight.
Unlike high-impact exercises, walking is gentle on the joints and minimizes the risk of exacerbating back pain.
Beginning with short, manageable walks and gradually increasing duration can be beneficial for those with back pain from disc herniation.
Pilates focuses on core strength, flexibility and overall body alignment.
By emphasizing controlled movements and proper breathing, Pilates helps strengthen the muscles that support the spine, including the abdominal, back and pelvic muscles.
This core strengthening enhances spinal stability and can reduce the strain on the back.
Pilates exercises promote flexibility and improve posture, which can help relieve pressure on the spine and reduce discomfort.
The emphasis on precise movements and proper alignment helps correct muscle imbalances and misalignments that may contribute to back pain.
What about yoga and stretching?
You do not need to be able to bend like a pretzel to do yoga.
There are basic poses, and even the difficult poses have beginner’s variations.


Shutterstock/Maridav
Dr. Kirschen also says, “Lying on back with legs elevated on a stack of shelves, gradually lowering the legs on each shelf until flat on the ground.”
He really stresses stretching, however, as a major component in pain relief.
He also emphasizes “Including pelvic tilts [below] and basic calisthenics we used to practice in gym class — the more you do this movement, the better it will feel.

Shutterstock/Mangostar
All in all, what is the most effective treatment for lower back disc herniation?
Dr. Kirschen also recommends the “application of moist or dry heat along the lumbar spine.”
Dr. Kirschen says that the “best treatments for acute and sub-acute pain from disc herniation are the epidural steroid injections and performance of acupuncture.”
 Dr. Kirschen is board certified in anesthesiology, pain medicine, acupuncture and massage therapy, and has extensive postgraduate training in osteopathic and manual medicine.
Dr. Kirschen is board certified in anesthesiology, pain medicine, acupuncture and massage therapy, and has extensive postgraduate training in osteopathic and manual medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/tommaso79
About this Site
Knowledge Is Power

Founded in 2012, Scarysymptoms.com has established itself as a leader for providing visitors in-depth information about their symptoms — not the template information of most other medical sites, but information straight from interviewed doctors that digs very deep into the issue.
What sets Scarysymptoms.com apart from the rest?
Most of the information here comes straight from interviewed physicians and other medical professionals who give detailed explanations that go beyond the generic, recycled symptom information found on other medical sites.
The expert sources for Scarysymptoms.com are respected and credible leaders in their medical field.
Furthermore, there is considerable content based on the firsthand caregiving experience of Scarysymptom.com’s founder, Lorra Garrick, regarding the following medical conditions that have affected her parents:
• Quintuple bypass surgery
• Mitral valve replacement
• Pacemaker implant
• Congestive/chronic heart failure
• Two total knee replacements
• One knee revision surgery
• Two total hip replacements
• Chronic subdural hematoma
• Two brain surgeries
• Three back surgeries
• Three shoulder surgeries
• Knee arthroscopy
• Herniated disc/sciatica
• Double carpal tunnel syndrome/surgery
• Pneumonia
• Low thyroid
• Clinical depression
• Peripheral neuropathy
• Diverticulitis
• Side effects from medications
• Mobility issues
In addition, Lorra writes about her own experiences with the following:
• Changing moles and mole removal
• Seborrheic keratosis
• Seborrheic dermatitis
• Finger pain/cramp (annular flexor pulley injury)
• Shoulder pain (rotator cuff injury)
• Biceps tendonitis
• Low backache
• Heel pain/burning heels (plantar fasciitis)
• Chondromalacia patella
• Quadriceps tendonitis
• Sudden-onset diarrhea (microscopic colitis)
• Change in stool caliber/color (microscopic colitis)
• Missed periods
• Headaches
• Sudden-onset dry mouth
• Continuous coughing (acid reflux)
• Beeturia
• Medial epichondylitis (golfer’s elbow)
• Hamstring injury
• Clicking jaw
• Blocked ears upon awakening
• Ganglion cyst
• Sprained ankle
• Sprained wrist
• PVCs
• Twitching muscles
• Panic attacks
• Actinic keratosis
• Benign paroxysmal positional vertigo
• Prophylactic double mastectomy (sister diagnosed with breast cancer)
• Broken collarbone
• ASD-1
Scarysymptoms.com, then, provides content that burrows deep into all facets of symptoms, from both the professional perspectives of esteemed physicians and also from a prolific writer who has been passionate since high school about health, fitness and strength.
Let’s put it this way: If you want to know the symptoms of colon cancer, any medical site will list these.
But if you want to know just what exactly “constipation alternating with diarrhea” actually means (and this symptom is definitely open to subjective interpretation), Scarysymptom.com covers it.
And if all the melanoma pamphlets and online guidelines say to look out for moles that are at least the size of a pencil eraser…does this mean that a one-millimeter spot can’t be melanoma?
And just why do ALS sites appear on the first page of a search for “cause of muscle twitching”?
Scarysymptoms.com picks up where all the pamphlet-type information of other medical sites leaves off.
The Autistic Advantage

In spring of 2022, Lorra received a clinical diagnosis that for some time, she’d been strongly suspecting she had. It was Autism Spectrum Disorder.
Having an Autistic brain enables Lorra to take deep dives into many medical topics of interest and dig hard right down to the bottom to present all the details, all the possibilities and variations, every single hypothetical and every potential aspect of a condition, symptom or set of symptoms to readers.
And she never tires of this venture, since Autism brings with it the capacity for sustained, deep, complex thinking and concentration on highly specific topics, and the ability to creatively and analogously present explanations in a way that’s easily understandable — yet brimming with all the details that readers seek.
Being on the Spectrum means that thinking outside the box comes easily to Lorra when developing content ideas and presenting subject matter.
Physical Fitness Aspect
Scarysymptoms.com also covers all aspects of fitness, exercise and weight loss.
After all, struggling to burn stubborn fat is a worrisome symptom for many men and women. So is failure to build muscle or gain more strength.
Lorra’s background as an ACE certified personal trainer, plus her own experience with strength training, powerlifting, interval training and injury recovery, have been converted to electrifying content that will empower anyone, be they a 90 pound weakling, someone who is very self-conscious due to obesity, a middle-ager with an expanding waistline or a senior-age person who has never exercised before.
Targeted Audience
• Men and women of all backgrounds, ages and lifestyle habits who want to know more about their symptoms or those of a loved-one without getting confused by conflicting, generic or vague information.
• Those who are simply annoyed by a symptom.
• Those who are worried sick over a symptom.
• People who have developed a fear of having a potentially fatal condition after googling what seems to be a minor symptom.
• Anyone who wants to lose fat, build muscle, sculpt their physique, run faster, lift heavier and live longer, plus improve their self-esteem and mental health.
The purpose of this site is to provide answers—from doctors with whom Lorra has personally corresponded with as a medical writer—to all the possible questions you may have about:
• Symptoms: alarming ones that mean nothing or that may mean danger
• Symptoms: minor ones that may mean a life threatening illness
• Differential diagnoses
• Misdiagnoses
• When to see a doctor and what kind of doctor
In addition, Scarysymptoms.com includes articles written by medical doctors and other medical professionals, plus articles by people who’ve experienced firsthand the condition they’ve written about.
*****
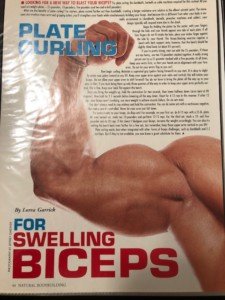
Lorra’s feature articles have appeared in the following print publications (below):
Abilities Magazine
ACE Certified News
American Institute for Cancer Research newsletter
Anchor Magazine
Blackbelt
Exercise for Men Only
Fitness & Physique Magazine
MAMM
Ms. Fitness
Natural Bodybuilding
OnFitness Magazine
Personal Fitness Professional
Taekwon Do Times
Today’s Latino Magazine
Vibrant Life
Images of Some Print Publications


Online publications include:
- Blackdoctor.org
- Howtobefit.com
- Verywellfit.com
Amazon Kindle Publications
- Crucify Fat with HIIT Workouts!
- Fitness Walking the Right Way for Fat Loss
- Maximum Fat Burn with Hormonal Walking
- Top 10 Worst Weight Exercises for the Rotator Cuff
- Shed Belly Fat and Get Ripped Abs
Lorra Garrick
Top image: Shutterstock/docstockmedia
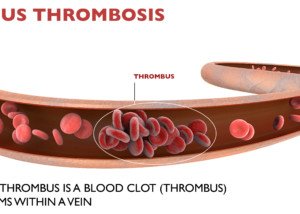
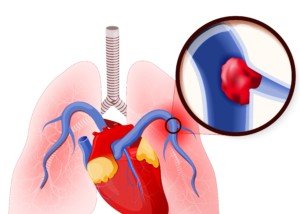
Can a Pulmonary Embolism Kill You on the Way to a CT Scan?
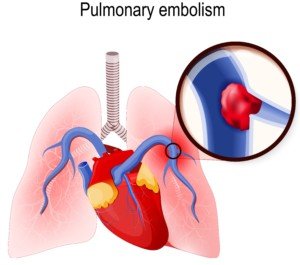
A pulmonary embolism is suspected, and the patient is being taken to the CT scanner to confirm this.
The D-dimer was positive and the patient is exhibiting the classic symptoms of a pulmonary embolism.
But the CT scan is needed for a verification before any powerful clot-busting drug is given. Doctors also need to see where the clot is specifically.
Yet on the way to the CT scan suite, the patient could go into cardiac arrest from the pulmonary embolism.
I wondered why isn’t the clot-busting drug immediately administered, right there in the hospital room — at least at a lower level — and THEN take the patient for his CT scan?
After all, it takes time to get to and on the CT scanner bed, take the image, then get a doctor to read the image results.
Certainly, the pulmonary embolism can cause death while the patient is enroute to the CT scanner or even during the scan?
Regarding the hospital patient presenting with sudden difficulty breathing and chest pain, “Clinically this scenario is one with a high index of suspicion for a pulmonary embolism,” says Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“Of course if the patient is on a cardiac monitor, you can look for tachycardia, EKG changes with signs of right heart strain, etc., to strengthen that suspicion.
“In most cases what you do next is start anticoagulation with IV Heparin immediately if it is not contraindicated; you do not need a confirmation with a CT to start treatment.”
Anticoagulation drugs are contraindicated in patients prone to internal bleeding.
Dr. Gashti explains, “In certain post-op patients such as spine surgery or neurosurgical patients, thrombolytics — clot busting drugs, and to some extent even Heparin is absolutely contraindicated because of risk of bleeding.”
Filter Can Prevent Pulmonary Embolism
“In these patients, you would place a filter, and if they are not in cardiac shock, you would support them.”
This filter (shown below) will prevent any deep vein thrombosis from getting into the lungs and embolizing.

IVC filter. BrusBlaus/CreativeCommons
Other patients may have hemodynamic problems. “If they are hemodynamically unstable, then they will need surgical thrombectomy — mechanically removing the blood clots (from the lungs),” says Dr. Gashti.
A patient who’s hemodynamically UNstable is NOT necessarily at risk for internal bleeding from thrombolytic drugs. Hemodynamics refers to primarily blood pressure.
“In a patient with hemodynamic instability in whom thrombolytics are not contraindicated, you can start IV thrombolytics, but this is not as effective as performing an angiogram and placing a catheter into the pulmonary artery where the blood clot is and delivering the medicine directly there; this of course requires a trip to the angio suite.”
This procedure is called intra-arterial infusion (of the thrombolytic drug), and is not to be confused with the surgical thrombectomy, which involves opening the chest, accessing the pulmonary artery and physically removing the blood clot—a major surgery.
Two Ways to Deliver Thrombolytics
IV and intra-arterially (through the femoral vein in the upper leg, feeding a catheter up to the pulmonary artery and delivering the clot-busting drug).
Dr. Gashti emphasizes that “in a patient with suspected or confirmed pulmonary embolism, who is hemodynamically stable (and not at risk for internal bleeding), all that is needed is systemic anticoagulation (which can be delivered via IV or intra-arterially). Most PE’s will not be fatal.
“So as you can see, this is not a condition where one treatment fits all. It really all depends on how the patient is doing.
“As you correctly mentioned, some patients are not stable enough to travel to the CT scanner, but a CT is only done for confirmation.
“If you suspect it, then treat it and worry about confirming it later.”

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Designua
Is Chest Pain, Breathing Trouble After Pulmonary Embolism Treatment Normal?

Is it normal to have trouble breathing and chest pain after successful treatment of a pulmonary embolism?
Might these symptoms reflect anxiety over the pulmonary embolism, or is it more likely that this means you have a new blood clot in your lung?
What a Doctor Says…
“If you are diagnosed with a DVT and a pulmonary embolism and being treated for it with systemic anticoagulation, and you are therapeutic on Heparin or Coumadin, the chance of having recurrent pulmonary embolism is low, but not zero,” says Seyed-Mojtaba (Moji) Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“So recurrent symptoms mandate new diagnostic workup—most likely a chest CT, and if recurrent PE is confirmed, patient has to have an IVC filter because this constitutes ‘failure of treatment,’ one of the indications to insert a filter.”
IVC stands for inferior vena cava. This is a large vein that carries blood into the lungs so that it can be re-oxygenated.
How long does the filter to prevent a pulmonary embolus stay in place?
Dr. Gashti explains, “If they suffer a PE, first or recurrent, while being anti-coagulated and therapeutic on their Coumadin, then this is a case of failure of therapy, and in most cases you would not remove their filter—it would be permanent.
“Having said this, you also need to look at the patient.
“If they are young and if their deep vein thrombosis was provoked, you may consider removing the filter but need to be careful with this.
“In any case, with current filters, the longest they can stay before having to be removed is 365 days.”
Symptoms of a Pulmonary Embolism
In addition to sudden chest pain, the patient may experience a sudden difficulty with breathing or getting air in, or may even pass out.
Coughing up blood is another possible symptom of a pulmonary embolism.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/peoplecreations
Pulmonary Embolism: What Can You Do Besides Call 9-1-1?

Would you know what to do, besides call 911, if someone near you seemed to be showing signs of a pulmonary embolism?
After all, a PE can kill in minutes.
“Sudden onset of shortness of breath and chest pain are hallmarks of pulmonary embolism,” says Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
Another symptom may be coughing (including with blood).
“If you just had major surgery and you are at home and experience these symptoms, especially if one of your legs is also swollen, this would be a PE unless proven otherwise.
“Of course there are numerous other causes in a post-op patient with these symptoms—pneumonia, atelectasis, cardiac issues, CHF, etc., but a PE has to be on top of the differential and you need to call 9-1-1.”
But is there anything else that you, as the layperson, can do to help this individual with the suspected pulmonary embolism?
Dr. Gashti says, “Unfortunately, if you are not in a hospital, perhaps not a whole lot.”
Perhaps you’ve viewed a scene in a fictitious TV drama where it appears that someone with medical training thinks a collapsed person is suffering from a pulmonary embolism.
The bystander then takes a sharp object, incises the chest somewhere and inserts a makeshift medical device (such as a drinking straw), and performs crude surgery.
Dr. Gashti explains, “The situation you are describing on a TV show sounds like treatment for a pneumothorax—collapsed lung, rather than a pulmonary embolism.
“With a collapsed lung, the problem is getting enough air to the lungs ,but a PE prevents blood from getting to the lungs from the right side of your heart. So placing a ‘tube’ in your chest would not work.
“Other possibility is that they were talking about a ‘tracheostomy’ tube through the middle of your neck into your trachea to ventilate the patient.
“But the general public should not attempt this since there can be more harm than good if you do not know what you are doing.
“So the best thing the general public can do if they suspect PE is to call 9-1-1 and to provide basic CPR if patient is unconscious.”
We may have to wait several decades before “Star Trek medical technology” allows a bystander to whip out the pulmonary embolus dissolution kit from their handbag and apply it to the collapsed victim.
In the meantime, know the warning signs of a pulmonary embolism.
If someone is at risk, check their legs several times a day for swelling, redness, a blanched or pale appearance, warmth in the area or tenderness to the touch.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/fizkes
When Are IVC Filters Used for Pulmonary Embolus Prevention?
How many hospital patients would die from a pulmonary embolism every year if from this point on, all surgery patients received an IVC filter — patients undergoing surgeries that increase the risk of a DVT?
Surgeries that strongly increase the risk of a deep vein thrombosis include knee replacement, hip replacement, abdominal and cardiothoracic.
Inferior Venacava Filter
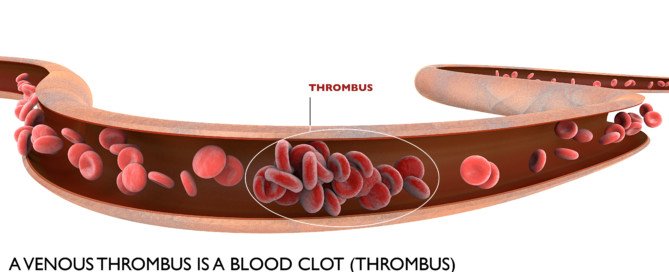
The IVC filter prevents a pulmonary embolism from developing by “trapping” a migrating DVT before it can enter a lung.
The IVC filter will not prevent development of deep vein thromboses.
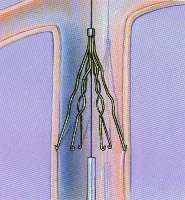
IVC Filter
Use of IVC Filters Prophylactically to Prevent Pulmonary Embolism
“We are doing this more and more in patients who are at very high risk for DVT (such as obese patients) or those who cannot be adequately anti-coagulated,” says Seyed-Mojtaba (Moji) Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
Some patients, such as trauma, are at high risk for dangerous internal bleeding if put on blood thinners.
“These filters are retrievable and would prevent a PE if they were to develop a DVT. Once they have recovered, the filter can be removed.”
Placement of the IVC filter for high risk patients has been the medical standard for years.
For example, a patient undergoing hip replacement may have a genetic blood clotting disorder that puts that person at high risk for a DVT even in normal everyday life. Such a patient would get the IVC filter.
However, placement of IVC filters is not the norm, not the standard, for the typical patient — one who does not have a high risk for DVT outside of what risk the surgery will bring on.
But such patients are not immune to DVT, and many indeed develop a blood clot that then becomes a pulmonary embolism.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Heart Attack after Normal Stress Test: How Does this Happen?
Yes, a person can have a normal stress test but a heart attack shortly after, says a cardiologist.
Ever wonder if you can have normal stress test results, then suffer a heart attack soon afterwards?
It can happen, says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.

Plaque buildup in artery. Shutterstock/Explode
Dr. Sayeed explains, “A stress test can miss blockages that are less than 50% of coronary artery luminal diameter because they may not cause enough compromise in blood flow to be detected on a stress test.
“But it is these less severe blockages that tend to be more unstable and prone to rupture, causing a sudden heart attack when they do rupture, such as in the setting of vigorous exercise–snow shoveling.”
The reason these are more unstable is because when plaque buildup is less than 50 percent, it hasn’t been around long enough to harden.
Soft plaque is prone to breaking off in tiny fragments, and those fragments can obstruct a coronary artery, causing a heart attack by preventing blood flow to the portion of the heart that the affected artery feeds.
Strenuous exercise can cause the soft plaque to rupture in a person who’s not accustomed to strenuous activity such as shoveling snow.
This can explain why a seemingly “healthy” person literally drops from a heart attack while shoveling snow.
You may be thinking, Gee, if blockage under 50 percent can be so harmful, maybe I should eat up the cheeseburgers and fries to get that percentage up to like 80 percent.
But Dr. Sayeed points out, “No, what this means is that in some people, whether they have mild or severe blockages, if the plaque is soft, meaning it has not been around long enough to become calcified — natural response by the body — the soft plaques tend to be more susceptible to rupture or erosion compared to a hardened calcified plaque that is slightly more stable.”
To learn how much of your coronary arteries have calcified, get a coronary calcium score test.
“The higher percentage plaques tend to be more calcified because they have been around longer and have been increasing in severity over time, and have become calcified and remodeled and more stable over time if the person never had a plaque rupture and heart attack.
“This can occur in those with silent coronary artery disease where the plaques slowly develop, become calcified over years and the person is just lucky they never had an event.
“And they only develop symptoms once these calcified severe lesions block blood flow enough to cause symptoms such as chest pain.
“This is usually in someone who is pretty well-conditioned and healthy but had risk factors.”
This doesn’t mean that a very high coronary calcium score means you’re safe from a heart attack.
Dr. Sayeed adds that in general, smokers won’t last long enough for their coronary artery plaque buildup to reach a severely calcified state “because the cigarette smoke will cause a soft plaque to rupture.”
He also explains that “heart attacks can occur from other types of plaque pathology such as plaque erosion, not just rupture from a plaque that may not be detected on a stress test.”
What percentage of people, after being told their stress test was normal, have a heart attack soon after?
Dr. Sayeed says, “Hard to say what the percentage is, but probably around 5-10% depending on the sensitivity and specificity of the stress test that was performed.”

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Andrey_Popov
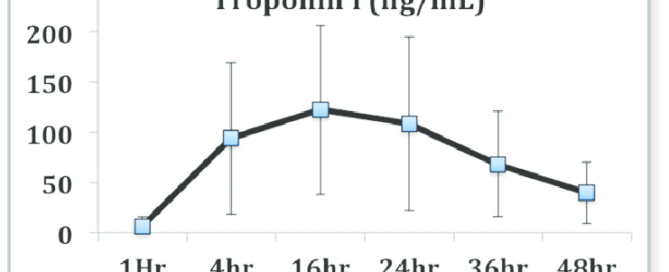
Can Troponin Elevation Mean Something Other than Heart Attack?

Patients who present in the emergency room with chest pain are given a troponin test (blood sample is taken by nurse).
Troponin is a protein enzyme that leaks from the heart when this muscle is damaged.
If the test result is elevated (in a range that indicates damage to heart tissue), this can mean that the patient had a heart attack very recently.
However, elevated troponin doesn’t always mean cardiac damage.
In fact, the test result isn’t either normal or elevated; there is another range — an in-between range.
It’s sometimes referred to as a gray area or indeterminate area, which (along with elevated status) warrants a follow-up blood draw several hours later to see if the result is of a higher value (meaning that even more troponin has leaked from the heart).
If elevated troponin doesn’t always mean damage to the heart, what else might it mean?
“It can mean a long list of non-cardiac things, the most common being from renal failure, heart failure, pulmonary embolus, cardiac contusion, sepsis, cardiotoxins, CNS disorders, excessive exercise,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
Generally, with modern assays and automated laboratory systems, troponin results can be returned within a few hours, often between one to three hours after the sample is taken.
Some rapid tests and point-of-care systems can provide results in as little as 20 to 60 minutes.
Other causes of elevated troponin not related to the heart muscle include:
1 High blood pressure (hypertension)
2 Drug toxicity
3 Low thyroid (hypothyroidism)
4 Rheumatoid arthritis
5 Transient ischemic attack and stroke