Here is where you may find the answers to your symptom questions about chronic subdural hematoma—right from a neurosurgeon.
Here are three questions about chronic subdural hematoma symptoms answered by Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
How much time must pass (“incubation period” or “grace period”) after the head trauma before the patient can know he won’t develop a chronic subdural hematoma, that he’s in the clear?
Of course, let’s assume that the initial CT scans, that were taken soon after the incident, were normal, and the patient had no symptoms.
“There is no clearly defined maximum ‘incubation period,’ but I agree that if someone will repeat CT scan of his head after three months of head injury and study will be normal, most likely patient is ‘in the clear,’” says Dr. Mikolaenko.
“I usually recommend to repeat CT scan in 3-4 weeks after head injury in patients older than 60 years.
“Yes, seizure can occur actually at any time after brain injury; even smallest scar on the brain might become epileptogenic focus for the rest of the patient’s life.”
Percentage of people with normal CT scans after hitting head who eventually develop a chronic subdural hematoma?
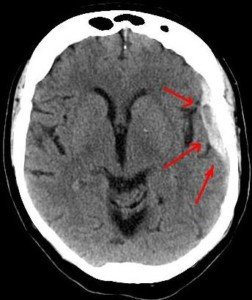
Dr. Mikolaenko says, “CSDH generally occurs in elderly, with average age being 63 years old, and head trauma is identified in almost 50% of these patients whose initial CT head [scan] was normal.”
Is the presence or absence of neurological symptoms at the time of head injury (fall on head, getting hit in head) predictive of likelihood of a chronic subdural hematoma developing?
In other words, if a patient can’t remember what happened to him and can’t follow instructions right after the accident, is he more likely to develop a cSDH than if he displayed no neurological symptoms whatsoever (he was lucid)?
“Yes, many cSDHs probably start out as acute SDHs,” says Dr. Mikolaenko.
“More severe symptoms at presentation very often indicate more severe head injury with even negligible blood within the subdural space, not visible on imaging, but enough to evoke inflammatory response and trigger complex chain of events on molecular level leading to formation of cSDH.”
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.