Causes of Piercing, Stabbing Chest Pain: Get to ER Fast

If you’ve been having ripping, stabbing or excruciating chest pain out of the blue, even if it comes and goes, get to the ER immediately.
You may have minutes to live…
“Stabbing or ripping chest pain always raises the specter of what we call ‘aortic dissection,’ says Dr. John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
“Aortic dissection means internal tearing of the aorta, separating the inner from the outer layers of the aorta.”
It’s not hard to understand why many people die within minutes of an aortic dissection — the aorta is the body’s largest blood vessel.
Blood that’s pumped by the heart goes into the aorta to be distributed to the rest of the body.
This great blood vessel has several branches that lead out from it, through which blood flows, and this includes to the brain.
What is an aortic dissection?
“This is exactly a ripping apart of the layers of the aorta, just as the term implies,” says Dr. Elefteriades.
“This is a very serious condition that usually requires an immediate operation.”
This situation never goes away on its own; it’s a ripped blood vessel!
It only gets worse; the course of it will lead to death unless it is promptly treated—and treatment is always surgery.
Aortic dissection results in massive internal bleeding. Some patients will die within minutes, while others have delayed the ER visit, not realizing how serious their situation was, and because the dissection was of a slower nature, they survived despite delaying the ER visit by up to a few days.
A “slower” dissection, however, will ultimately lead to death if it is not surgically repaired.
So if you or someone you know has been complaining of agonizing or ripping chest pain, don’t wait another second in getting to the ER.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
,
Top image: Shutterstock/ Robert Kneschke
Intestinal Gas Bubbles: Sharp, Stabbing Rib Pain Explained

Here’s information on why gas bubbles in the intestines can cause so much pain, including in the rib area.
It can stop you dead in your tracks: sudden, stabbing pain in a specific region of your abdomen, and when it’s in the rib area, it can really take your breath away.
Why can a gas bubble in the intestines be so painful?
“Intestinal gas causes pain because of distension of the intestine,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“When your intestinal wall becomes abnormally distended, this usually results in discomfort.
“It usually resolves when the distension resolves, mostly by either passing gas or belching, depending on where the distension is.”
Keep track of when this nasty symptom strikes you. You should become acutely aware that within a rather brief time from the onset of this symptom, you’ll start passing gas (or burping).
In fact, don’t be surprised if you have more flatulence than usual, or if it’s frequent over the next few hours or more.
Rib Pain
“Most of the time, intestinal gas is from swallowed air,” says Dr. Blume.
“One can get abdominal distension from structural or functional problems in the gastrointestinal tract.
“However, if one has significant abdominal distension, it can cause discomfort around the rib area as a result of this.”
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Anus Wax Buildup: Causes and Solutions

Find out what a doctor says about the causes of anus “wax” buildup…
Many people want to know what can cause a buildup of “wax” in their anus.
Now, what’s really interesting about this question is that what an individual perceives as a wax-like substance, in fact, isn’t wax at all.
Wax, like the type of substance that accumulates in the ears, does not accumulate in or near the anus.
What does a person actually see, then, or even feel, if it’s not similar to the wax that collects in the ears?
“If you mean passing mucous per rectum, these are usually normal secretions,” begins Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“Your colon normally secretes mucous to function as a lubricant for helping with bowel movements.
“When one’s colon becomes somewhat irritable for whatever reason, it often secretes more mucous, and one sees it in the stool.
“As a rule, it looks scarier than it actually is, and most of the time does not require specific intervention.”
As this mucous squirts out of the anus as you strain with a bowel movement, or even with an easy bowel movement, it may have a slimy feel to it as it passes through.
You look in the toilet and see white or whitish-clear gobs of something. Don’t panic; think lubricant. Let it be.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ANN PATCHANAN
Doctor Explains Cause of Chest Burning from Running
Find out why hard running causes a burning sensation in your chest.
What causes “burning” in the chest (or lungs) from running?
“From a digestive point of view, hard running may cause burning in the chest through various mechanisms,” begins Steven Fleisher, MD, a gastroenterologist in Rosedale, Maryland, with 20+ years of experience.
“Unfortunately, most research associating chest pain, burning or discomfort and exercise focus on the heart.
“And since the heart and the esophagus share a common nerve supply, distinguishing between cardiac and esophageal chest discomfort may prove difficult since exercise may provoke both.”
Nerve Involvement
“The sensation of ‘burning’ implies a nerve, or inflammatory (nerve irritation) cause of the pain.
“In my opinion, the following are the three most likely esophageal mechanistic causes of chest burning that may be exacerbated by hard running.”
#1. Reflux
“Gastroesophageal reflux tops the list and is responsible for causing chest discomfort in upwards of 30% of patients complaining of chest pain at baseline.
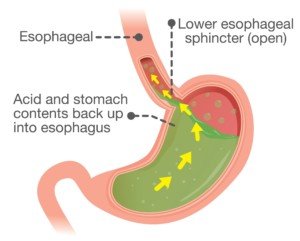
Acid reflux. Shutterstock/solar22
“Hard running after a large meal or eating while running may predispose to reflux and chest burning through mechanisms that include increased abdominal pressure associated with the respiratory effort of hard running, as well as the type of food consumed before or during running.
“Food types that are spicy or high in fat concentration may lower the pressure in the valve at the end of the esophagus and predispose to regurgitation, irritation and chest burning.
“Other factors promoting reflux include delayed emptying of the stomach secondary to reduced blood flow, impaired secretion of protective factors by the stomach and esophageal lining.”
#2. Esophageal Hypersensitivity
“Secondly, patients may have baseline esophageal hypersensitivity with lower threshold for esophageal burning in response to normal secretions; this may be exacerbated by exercise.”
#3. Dysmotility
“Thirdly, and more speculatively, hard running may induce abnormal contraction (dysmotility) of the esophagus that is often associated with chest discomfort.”
Other Causes
“Chest burning can also be associated with non-digestive causes including airway irritation particularly in cold weather, or when hard running is undertaken when not physically fit or accustomed to the respiratory effort associated.”
For some people, they may find that over time, as they improve their cardiovascular condition, the burning sensation in their chest (or lungs) will disappear.
Consistency with running is key.
Realize that you may become quite adapted to a particular cardio mode such as running fast on level courses or running up hills.
But then, for the first time in ages you decide to do “sprints” on an elliptical machine.
Don’t be surprised if this change in mode shocks your body and produces that chest or lung burning sensation.
Dr. Fleisher was named a 2015-2018 “Top Doc” by Baltimore Magazine for gastroenterology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/KamranAydinov
How Many Americans Under 65 Get Esophageal Cancer Every Year?
A GI doctor addresses the question of percentage of people younger than 65 years who develop esophageal cancer.
*****
Even though esophageal cancer is most prevalent in people over the age of 65, this does not mean that younger adults can’t develop this disease.
“The following is from a SEER database, and represents data collected between 2005 and 2009,” says Steven Fleisher, MD, a gastroenterologist in Rosedale, Maryland, with 20+ years of experience.
The Data
Dr. Fleisher explains, “From 2005-2009, the median age at diagnosis for cancer of the esophagus was 68 years of age.
- Approximately 0.0% were diagnosed under age 20
- 0.3% between 20 and 34
- 2.3% between 35 and 44
- 12.2% between 45 and 54
- 26.1% between 55 and 64
- 27.4% between 65 and 74
- 23.7% between 75 and 84
- 8.0% 85+ years of age.”
You may be wondering why the percentage drops as the age exceeds 74, since the older one gets, the weaker their body’s cancer surveillance system gets.
The drop in percentage reflects (not necessarily to the full degree) the fact that many people simply do not live beyond age 75 due to succumbing to America’s No. 1 killer: heart disease.
Other cancers, followed by stroke, also take out a significant number of people every year before their 75th birthday.
It is also believed by many researchers that if one’s genes (“super genes”) allow them to live past 85, they would not be as vulnerable to malignancies.
Acid Reflux and Esophageal Cancer
“The type of esophageal cancer associated with GERD is called adenocarcinoma,” says Dr. Fleisher.
“This type of esophageal cancer has been rising in incidence in the United States over the last three decades, particularly in Caucasian men.
“Between 2000 and 2004 one U.S. cancer registry had the incidence of adenocarcinoma of the esophagus in white men at 5.69 per 100 000.
“GERD is a risk factor for adenocarcinoma, and a history of heartburn is found in up to 60% of those diagnosed with esophageal adenocarcinoma.”
Dr. Fleisher was named a 2015-2018 “Top Doc” by Baltimore Magazine for gastroenterology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Kateryna Kon
How Long Can Esophageal Spasms Last?
Find out what a gastroenterologist says about how long or short an esophageal spasm might last.
*****
You may be wondering for how long or for how brief an esophageal spasm may be.
They can be quite painful, but at other times the pain can be at a more moderate level.
The “Esophageal Spasm”
“‘Esophageal spasm’ is a lay term,” begins Steven Fleisher, MD, a gastroenterologist in Rosedale, Maryland, with 20+ years of experience.
“It implies some form of discomfort, or clinical symptom such as difficulty swallowing associated with or purportedly due to abnormal function of the esophagus with intense or abnormal contraction or ‘spasm.’”
Dr. Fleisher says that an esophageal motility study is the “best test of esophageal dysfunction supporting evidence of increased pressure in the esophagus and hence ‘spasm.’”
An esophageal motility study measures how well the esophagus moves food to the stomach using pressure sensors during swallowing.
Duration of Spasms
“In these studies, the duration of contractions or ‘spasms’ is important,” says Dr. Fleisher.
“For example, to meet the criteria for the entity ‘diffuse esophageal spasm,’ one is required to have contractions that last for greater than six seconds, are repetitive, and do not often progress down the esophagus in the normal way.
“Other important criteria include increased pressure in the esophagus.”
He continues: “Esophageal spasms can vary in duration. Clinically important contractions need to persist for more than six seconds.”
If pain in the esophageal area lasts only a second to a few seconds, it could be a spasm of a skeletal muscle.
When that happens, ask yourself if you did an upper body workout within the past few days.
As far as getting the correct diagnosis, Dr. Fleisher explains that an esophageal spasm is “often a clinical diagnosis, and a diagnosis of exclusion.
Endoscopy is a poor test for evaluation. X-ray study such as a barium swallow will provide better physiological information suggesting disordered contraction but are poor at associating symptoms with the observed abnormality.”
Dr. Fleisher was named a 2015-2018 “Top Doc” by Baltimore Magazine for gastroenterology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
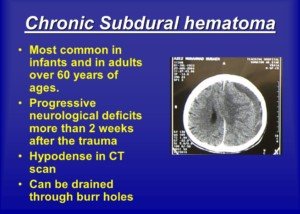
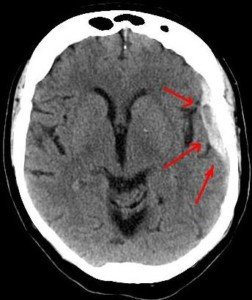
Anti-Seizure Drug Prophylactically after Head Trauma?
A neurosurgeon addresses taking anti-seizure drugs after head trauma even if there are no symptoms, just in case to prevent a seizure.
Keppra is an anti-seizure drug that may be given to a patient who has been diagnosed with a chronic subdural hematoma following a head trauma, such as hitting the head in a fall.
A chronic subdural hematoma is a slow brain bleed which may not start causing symptoms until two or three months after the trauma.
The drug is given when there are neurological symptoms from the head trauma, but not necessarily a seizure-type symptom.
After my mother underwent surgical draining of a chronic subdural hematoma, she was prescribed Keppra, because the risk of a seizure exists post-surgically for this condition, which affects mostly people over 65, though younger people can suffer from it.
Seizures are one of the more uncommon symptoms that arise from a chronic subdural hematoma prior to treatment.
More common symptoms are headaches, mental changes and weakness on one side of the body.
If you know that seizures (though not commonly) can result from a chronic subdural hematoma (that develops after head trauma), you then might wonder this:
Why not take an anti-seizure drug even if the CT scan is normal and the patient has no symptoms — just to play it safe?
After all, a normal CT scan doesn’t predict a future normal CT scan.
Remember, a chronic subdural hematoma may take up to 90 days to develop enough to start causing symptoms, which as mentioned, can include a seizure.
So why not be ready for a seizure by taking an anti-convulsant medication on a “just in case” basis?
Otherwise, the patient, unaware that a brain bleed is developing, might have a seizure from it while driving or walking down a flight of stairs.
To all of this, here is what Ivan Mikolaenko, MD, says:
“No prophylactic antiepileptic drugs are recommended in a patient with normal CT scan and no seizure following head injury!!!”
Dr. Mikolaenko is a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Masha Petrakova
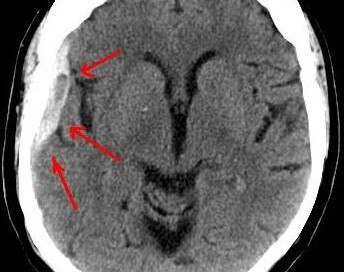
How Soon after a Normal Head CT Can You Drive?
It’s a fair question: For how long should you avoid driving after hitting your head, even though the CT scan is normal and you have no symptoms?
You hit your head and that day, get a CT scan to see if there’s any sign of subdural hematoma. The CT scan is normal.
However, you also know that a normal CT scan the day of head trauma, and even 24 hours later, doesn’t guarantee you can’t develop a slow brain bleed (chronic subdural hematoma) over the next few months…causing disturbing neurological symptoms.
Some of the symptoms that a chronic subdural hematoma can cause are sudden and profound weakness of one or both legs or arms; a seizure; cognitive impairment; and a searing headache.
In fact, a symptom from chronic subdural hematoma can mimic that of stroke or transient ischemic attack. Imagine driving while a symptom (or two) suddenly strikes.
Could you control the car while your brain is bleeding?
You may not even KNOW you’re having a symptom, and thus, begin losing control of the car and not even know it!
This begs the question:
For how long should a person (particularly elderly) avoid driving even if their CT scan (and next-day follow-up CT scan) is normal, and they are sent home with no symptoms?
“It depends on severity of initial presentation,” says Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
“I usually recommend to take a rest and don’t drive until all symptoms are gone, and I usually recommend to repeat CT scan in 3-4 weeks after head injury in patients older than 60 years.
“After that, given normal exam and normal imaging, patient can go back to driving.”
In other words, no symptoms at initial presentation in ER, and with a normal CT scan, mean that the patient is free to drive.
However, the patient should never drive TO the ER after hitting their head, since at that point, no diagnosis has been made.
You should always have someone drive you to the ER even if you “feel fine.”
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Mortality of Chronic Subdural Hematoma Soon After Drainage?
A certain percentage of people will die soon after having their chronic subdural hematoma drained.
The drainage procedure takes only 15 to 20 minutes, yet within 30 days, five percent of patients will be dead.
A 5% Mortality Rate within 30 Days of Burr Hole Drainage of a Chronic Subdural Hematoma
Just prior to my mother undergoing the 15-20 minute drainage procedure for her chronic subdural hematoma, the neurosurgeon told me that the biggest risks were infection and recurrence.
He made no mention of a mortality rate for the noninvasive procedure.
However, I’ve read in several online neurosurgery journals that there’s a well-documented mortality rate in patients within 30 days of the burr hole drainage of their chronic subdural hematoma.
One study said a 5 percent mortality rate. Another said a 6 percent mortality rate out of the 157 patients investigated.
“Although most of cSDHs often appear innocuous, severe complications may occur,” says Ivan Mikolaenko, MD, a board certified neurologist with subspecialty certification in neurocritical care, Neurological Surgery, P.C., New York.
Dr. Mikolaenko says those include the following.
“- Devastating intracerebral hemorrhage due to rapid brain decompression leading to hyperemia (increased blood flow) immediately beneath the hematoma or at any other area of the brain which was shifted and compressed for many days before surgery.
“- Failure of the brain to re-expand, especially in patients with pre-surgery low subdural fluid collection pressure: These people very often will have re-accumulation of the subdural fluid.
“- Intractable seizure post-op with or without status epilepticus.
“- Longstanding cSDH with conversion to subdural empyema (collection of subdural pus).
“- Untreated severe pneumocephalus (collection of bubble of air in place of evacuated subdural collection).”
As frightening as this mortality information all sounds to anyone who’s been diagnosed with a cSDH, it’s very important to realize that the death rate is still relatively low.
If you’ve hit your head recently, or know someone who has, be on the very vigilant lookout for any new-onset suspicious symptoms.
This includes out-of-character change in mood, memory issues, weakness, change in gait pattern, apathy, sudden headaches, or anything that just doesn’t seem right with the individual.
A chronic subdural hematoma is a slow bleeding in the brain, beneath the dura mater, and may take up to 90 days to begin producing symptoms.
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Volodymyr Baleha
Chronic Subdural Hematoma Questions Answered by Doctor
Here is where you may find the answers to your symptom questions about chronic subdural hematoma—right from a neurosurgeon.
Here are three questions about chronic subdural hematoma symptoms answered by Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
How much time must pass (“incubation period” or “grace period”) after the head trauma before the patient can know he won’t develop a chronic subdural hematoma, that he’s in the clear?
Of course, let’s assume that the initial CT scans, that were taken soon after the incident, were normal, and the patient had no symptoms.
“There is no clearly defined maximum ‘incubation period,’ but I agree that if someone will repeat CT scan of his head after three months of head injury and study will be normal, most likely patient is ‘in the clear,’” says Dr. Mikolaenko.
“I usually recommend to repeat CT scan in 3-4 weeks after head injury in patients older than 60 years.
“Yes, seizure can occur actually at any time after brain injury; even smallest scar on the brain might become epileptogenic focus for the rest of the patient’s life.”
Percentage of people with normal CT scans after hitting head who eventually develop a chronic subdural hematoma?
Dr. Mikolaenko says, “CSDH generally occurs in elderly, with average age being 63 years old, and head trauma is identified in almost 50% of these patients whose initial CT head [scan] was normal.”
Is the presence or absence of neurological symptoms at the time of head injury (fall on head, getting hit in head) predictive of likelihood of a chronic subdural hematoma developing?
In other words, if a patient can’t remember what happened to him and can’t follow instructions right after the accident, is he more likely to develop a cSDH than if he displayed no neurological symptoms whatsoever (he was lucid)?
“Yes, many cSDHs probably start out as acute SDHs,” says Dr. Mikolaenko.
“More severe symptoms at presentation very often indicate more severe head injury with even negligible blood within the subdural space, not visible on imaging, but enough to evoke inflammatory response and trigger complex chain of events on molecular level leading to formation of cSDH.”
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.