Does a Zero Calcium Score Always Mean a Healthy Heart?

The coronary calcium scoring procedure is very accurate at predicting the likelihood of the presence of heart disease, but does this mean that a result of zero automatically means you can’t possibly have any heart disease?
“Yes, even if the calcium score is zero, one can still have some form of heart disease,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
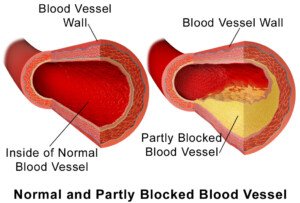
“A calcium score of 0 usually means that there is no significant coronary artery disease, or there may be coronary artery disease in the form of a soft non-calcified plaque that can still rupture and cause a heart attack.”
The test that can show this soft, non-calcified plaque is the CT angiogram.
If you have soft plaque, it won’t necessarily be built up enough to restrict blood flow in your heart (and cause chest pain).
The type of plaque that restricts blood flow is the hard, calcified type.
Thus, if a person has angina (chest pain from “clogged” arteries restricting blood flow), this doesn’t mean they also have a lot of soft plaque too; in fact, there’s no correlation.
A person can have a calcium score of 1,000 and chest pain from exertion, yet have very little soft plaque.
He may never have a heart attack — unless the hard plaque builds up enough to literally obstruct the vessel, blocking 100 percent of the blood flow through it.
This isn’t a rupture. A rupture of soft plaque means a piece of it has broken off and has lodged in what can be an otherwise clear vessel, blocking blood flow.
Imagine a pea inside an otherwise clean straw. Imagine that the pea-sized blockage broke off from a larger mass of the “pea” further upstream from that point, in a wider vessel.
“Even though there may be a minor buildup of soft plaque, it can still rupture,” says Dr. Sayeed.
“A zero calcium score only tends to rule out significant coronary disease, but it doesn’t mean that the structure of the heart is normal or that the pump function or the valvular function of the heart is normal,” says Dr. Sayeed.
“These could all be a problem and yet the calcium score can be 0 and be misleading.”
An echocardiogram will reveal cardiac structure, pump and valvular function.
“Even if the calcium score is 0 and no soft plaques are obviously detected, there may still be vulnerable plaques that are too small to be seen and can cause the so-called healthy person heart attack or sudden death.”
What can you do to reduce soft plaque or stop the progression of soft plaque?
BruceBlaus
- Green tea supplementation
- Magnesium citrate supplementation
- Krill or cod liver oil supplementation (high doses)
- Avoid manmade sugars as much as possible.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/goodluz
Can Resting Pulse in 90s from Stress Harm the Heart?

Find out what can happen if stress is causing your resting heart rate to be in the 90s.
Have you noticed that whenever you take your resting heart rate, it’s in the 90s, even though you’ve been at rest, have not smoked, have not ingested a lot of caffeine and are negative for hyperthyroidism or anemia (which both cause high resting heart rate)?
Frequently being in a state of anxiety or chronic stress can cause the resting heart rate to often register in the 90s.
Anxiety and stress trigger the body’s “fight or flight” response, which elevates heart rate as part of the body’s way of preparing to deal with perceived threats.
When this occurs often enough, it can lead to a persistently high resting heart rate.
The body remains in a heightened state of arousal, causing the heart to beat faster even when you are at rest.
Can this cause harm to your heart, even though otherwise you’re healthy?
“Resting heart rate in the 90s is still usually considered normal,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“The Mayo Clinic defines a normal heart rate as between 60 and 100. So being in the 90s is still considered to be normal and likely won’t harm the heart.”
But isn’t a slower resting heart rate better?
“Of course, if possible, it is always better to have a lower resting heart rate if possible, closer to the 60 goal,” says Dr. Sayeed.
“This is due to the fact that higher heart rates tend to cause increased production of inflammatory molecules and reactive oxygen species which can damage the heart, and a higher heart rate tends to cause more mechanical stress on the heart.”
If you can’t avoid situations that cause stress, or are prone to feeling a lot of anxiety, even to trivial triggers, you can fight against a resting pulse in the 90s by consuming a lot of fresh vegetables and fruits, which are high in antioxidants, and these will help neutralize the reactive oxygen species.
Another way to help bring the resting pulse down from the 90s is to regularly engage in rigorous or even moderate-intensity cardio exercise.

Shutterstock/Liderina
“In someone with coronary disease or heart disease already present, higher heart rates can lead to ischemia (blocked oxygen supply) and further damage to the heart,” says Dr. Sayeed.
When you engage in consistent aerobic activity, your heart becomes more efficient at pumping blood.
This efficiency means that with each heartbeat, your heart will pump a larger volume of blood, so it won’t need to beat as frequently to circulate the same amount of blood throughout your body.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE certified personal trainer.
Can Angina Occur at Rest but Not During Exercise?

Find out if it’s possible to have angina at rest but not during or resulting from exercise or physical activity.
You may know that it’s possible to experience angina during exercise or physical exertion, but not at rest, since cessation of the activity brings down the body’s oxygen needs, imposing less burden on the heart.
This is called stable angina.
However, unstable angina is when an episode can occur at rest, even during sleep.
“In general, if someone has angina at rest, this angina will only get worse with exertion because the heart is beating faster and needs even more oxygen which it is not getting” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“There are rare instances where angina at rest may go away with exercise, and this could only happen if the heart were to recruit more collateral blood supply with exercise that might increase blood supply.
“But in general, this is usually extremely rare and not seen.”
But there is a specific condition that can cause angina while at rest, which is not related to coronary artery disease (plaque buildup), heart valve problems or chronic heart failure. It’s called Prinzmetal’s angina.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Korawat photo shoot
Why Resting Heart Rate Speeds Up Later in the Day
A cardiologist explains what causes resting heart rate to speed up as the day goes on.
“The resting heart rate is the lowest at night while sleeping as well as during the first minutes after awakening, provided the person did not wake up abruptly from a dream or jump out of bed,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
Take your pulse first thing in the morning, before exiting bed or eating anything.
“It is in the calm lazy waking type of day. The resting heart rate will not increase by too much over the course of the day, but will be higher than what it was during sleep or first wakening due to mainly physical activity, stress, anxiety, circadian rhythm, etc.,” says Dr. Sayeed.
“Caffeine in fact at doses in regular coffee that people drink will actually lower resting heart rate due to its blood pressure increasing effects.
“High doses of caffeine such as in energy drinks and maybe huge cups of coffee will increase resting heart rate as will nicotine.”
There is no heart disorder that causes the pulse to become fast as the day or evening wears on.
Cardiac conditions that cause a rapid heartbeat do not care what time of day it is. So don’t worry if your pulse becomes elevated only in the evening.
Free-floating anxiety, which is when a person persistently has elevated adrenaline levels due to frequently feeling anxious, nervous or fearful, will cause resting heart rate to climb over the course of the day, maybe topping out at about 20 BPM more than what it was in the morning.
How to Help Control an Evening Elevated Heart Rate
Stress management should be implemented. So should an inventory of things that usually happen to you later in the day.
You may find that stressful situations tend to concentrate later on or in the evening, thus jacking up resting heart rate.
Thirty minutes of rigorous exercise will do wonders to help neutralize stress hormones.
If you’re already exercising throughout the week, make sure that your workout time is actually dedicated to working out, rather than telling yourself, “I got my exercise cleaning up the kids’ rooms today.”
Examples of dedicated time for vigorous exercise includes brisk walking outdoors that includes hilly areas; jogging in a park; a fitness class; and a weight or resistance workout.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How Long Should Pulse Be Elevated After Intense Exercise?
Find out what a cardiologist has to say about how long resting heart rate should stay elevated after intense exercise.
Those who faithfully exercise will be curious about resting heart rate.
“Pulse should be elevated for only a brief time after intense exercise such as a stress test in a normal heart in a conditioned individual,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“This is called heart rate recovery. Normally, a rapid drop in heart rate after strenuous exercise within a given period of time indicates a healthy and conditioned heart.
“The heart rate should drop by 12 BPM or more, one minute after stopping exercise.
“If it does not, it could indicate a deconditioned heart or a heart that is not receiving enough parasympathetic and vagal nerve tone which usually slows the heart down.”
Biggest Predictor of All-Cause Mortality
“This poor heart rate recovery is usually a predictor of higher mortality from left ventricular systolic dysfunction, cardiac ischemic disease and chronotropic incompetence cardiac arrhythmia,” says Dr. Sayeed.
According to studies, a poor heart rate recovery is the biggest predictor of all-cause mortality. You should keep in mind that causal relationship is extremely important.
For example, a person who smokes and does not regularly exercise, very most likely will have a poor heart rate recovery and a resting pulse that stays quite elevated after physical activity or unexpected exertion.
It stands to reason that such an individual (sedentary smoker) won’t live a long life.
To bring heart rate back down more quickly after stopping exercise (e.g., improve heart rate recovery), you should do aerobic exercise at least three times a week, and two of those sessions should consist of interval training.
The other session should be long-duration, fixed-pace aerobics.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Black or Tarry Stools from Cancer vs. from Food or Drugs

Find out just what “tarry” stools look like when compared to black BMs from benign causes like food or medications.
How often have you read a pamphlet or online article about colon cancer and came upon the term, “tarry stools”? Tar? Have you even ever seen hot tar?
The reason that black stools are often referred to as “tarry” is because, says Michael Blume, MD, “Black stools from bleeding actually have a somewhat sticky appearance, much like tar, while this is often not the case if it is from foods or medications.”
Dr. Blume is a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“Tarry stools is a term that describes the appearance of the stool, where it looks sticky like tar.”

Tarry stools
Think back to a time when, perhaps, you saw what tar looked like on a sidewalk before it dried. Now, imagine that being mixed in with your BMs.
“We often show patients something black to make sure that they actually mean black.”
Are you absolutely sure that your bowel movements are the same hue as your raven dress shoes or coal-colored attire?
What else is “solid” black?
Place a stool sampling on a paper plate and hold it right beside a charcoal-colored item for comparison.
You might find that your poop is actually a very dark brown.
“Tarry stools usually relate to their visual description. In additional to being black, when from bleeding, they also can look rather sticky.” Sticky is the key word.
This all does not mean that if a disease process is causing very dark BMs, that they are necessarily tarry.
Dr. Blume says, “I certainly would not use appearance as the sole criteria with which to base a decision as to whether it was related to bleeding.
“Usually when one is bleeding from the upper GI tract enough to cause tarry stools, the stools are often looser and occurring more frequently.
“Blood is actually quite a good laxative, so one often looks at stool frequency and consistency as a measure of how actively someone is bleeding.
“Black stools that are formed and not frequent are often less likely to be related to bleeding.”
Very dark BMs can be caused by spinach, beets and Pepto Bismol, says Dr. Blume.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Photology1971
Benign Causes of Greasy Oily Stools

A GI doctor describes benign causes of oily or greasy bowel movements.
Do your stools look slimy, oily or greasy?
If they appear different lately, you should see a gastroenterologist, since only a doctor can determine for sure what the cause is.
“Greasy or oily stools, assuming one is not ingesting mineral oil, etc., is often a sign of fat malabsorption,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
“This can have many causes, including certain infections, as well as small bowel or pancreatic problems.
“Determining the cause often involves taking a detailed history as well as some diagnostic testing.”
What about IBS?
“One needs to differentiate oily looking stools and mucous in the stool,” says Dr. Blume.
“Many people with IBS complain of having mucous in their stools and that their stools look slimy.”
But mucous in the stools is not the issue with the conditions (described below) that cause oily bowel movements.
When stools are oily or greasy, this is called steatorrhea.
Pancreatic Problems
“One usually malabsorbs fat (this is what makes stools oily) if there is a problem with pancreatic function, such as with chronic pancreatitis, or from problems in the small intestine where fats get absorbed, such as with celiac disease, certain infections, such as Giardiasis, small bowel bacterial overgrowth, or other inflammatory diseases.”
One such inflammatory disease is Crohn’s disease.
Benign Causes of Greasy Oily Stools
Benign causes of steatorrhea, or oily stools, often involve dietary factors or non-serious gastrointestinal issues.
One common benign cause is the consumption of high-fat foods or supplements, such as those rich in oils or fats, which can lead to temporary steatorrhea.
You’ll be able to see the “greasiness” in your poops.
Another cause can be the use of certain medications, like those containing bile acid sequestrants, or specific weight loss drugs, which can interfere with fat absorption.
Additionally, rapid gastric emptying, also known as dumping syndrome, can lead to steatorrhea.
This occurs when food moves too quickly from the stomach to the small intestine, leading to insufficient digestion of fats.
Similarly, lactose intolerance can occasionally result in oily stools if the body can’t properly digest dairy products, though it more commonly causes diarrhea and gas.
These benign causes typically resolve with dietary adjustments or discontinuation of specific medications.
Can cancer cause oily stools?
Yes, cancer can lead to steatorrhea.
Pancreatic Cancer: This is one of the most common causes of steatorrhea.
The pancreas produces digestive enzymes that help break down fats.
If pancreatic cancer impairs enzyme production or blocks the pancreatic duct, it can lead to poor fat digestion and absorption, resulting in oily stools.
Biliary Tract Cancer: Cancers affecting the bile ducts or gallbladder can interfere with bile flow.
Since bile is essential for the digestion and absorption of fats, obstruction or disruption in bile flow due to cancer can lead to steatorrhea.
Small Bowel Cancer: Tumors in the small intestine can disrupt the digestive process and lead to malabsorption of nutrients, including fats, causing oily stools.
] In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Blood Loss Symptoms of Black Blood in the Stools

“Black stools are often a sign of bleeding from a site in the upper GI tract, such as an ulcer, etc.,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
What else can make your bowel movements appear black?
“Common causes of this could include medications such as iron or Pepto Bismol,” says Dr. Blume, “as well as certain foods, such as spinach or beets.”
Black licorice has been known to turn bowel movements a very dark color. And even though spinach is green, a generous amount of this nutrient-dense vegetable can turn poops very dark.
Dr. Blume continues, “Symptoms are not usually the best guide, as many people who have bleeding ulcers often have no pain associated with their ulcer, and present with a complication of their ulcer, such as bleeding.
“Certainly, if one feels weak or dizzy, especially on standing up, it may be a sign that one is bleeding significantly.
“Additionally, one may have other signs of significant blood loss, such as cardiac symptoms and shortness of breath.
“Being anemic can impair your blood’s oxygen-carrying capacity and cause cardiac symptoms.”
Anemia can be caused by internal blood loss, such as that from an ulcer or a cancerous tumor in the colon.
Risk Factors for Bleeding Ulcers
Dr. Blume explains, “One may want to examine if they have risk factors for ulcers such as cigarette smoking, taking anti-arthritics, etc.
“One should be aware of the context in which one sees the black stools to best interpret this finding.”
Take note of what you eat.
If you see nearly black poops in the toilet bowl the day or two after you ate a lot of licorice, spinach, shellfish or organ meats (the last three are high in iron), that can very well be the explanation.
If there’s no correlation with food intake, see your doctor.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Blood in Stools, No Other Symptoms: Colon Cancer?
Find out if bloody stools can be the only symptom of colon cancer.
How likely is it that if you see blood in your stools, but do not have any other symptoms (e.g., unexplained weight loss, abdominal pain), that you can actually have colon cancer?
“Colon cancer often presents with no symptoms,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
You’re probably wondering how such a patient’s colon cancer is then discovered if there are no symptoms.
It may be found incidentally, via imaging for an unrelated issue, or during a routine colonoscopy.
“Not all colon cancers bleed, and when they do bleed, it’s often is not visible, i.e., occult bleeding, which can be picked up on chemical tests, but not visible,” says Dr. Blume.
“This is why it is very important to have screening colonoscopies at the appropriate time, even if you have no symptoms. Remember that lack of symptoms does not mean lack of a problem.”
Blood in Bowel Movements and Colon Cancer
“Colon cancers usually do not cause tarry stools,” continues Dr. Blume.
“The bleeding that one sees is usually bright red or maroon. Bleeding may be the only sign that one may see, even with an advanced cancer.
“One can see pain, bowel dysfunction, weight loss, etc., with colon cancer.
“Usually, when one sees these symptoms when they are related to a colon cancer, it is often quite advanced.
“It is important to understand, however, that if one sees bleeding per rectum, the lack of other symptoms, such as pain, bowel dysfunction, weight loss, etc., does not mean that one does not have a cancer.”
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/yanalya
sscpywrt26
Can Menstruation Be Affected by Irritable Bowel Syndrome?

It’s not true that irritable bowel syndrome can affect menstruation.
“IBS, while a disorder that can cause rather inconvenient symptoms, is not a dangerous disease, and is not associated with any increased risk for other serious diseases,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
Irritable Bowel Syndrome and Your Period
“If one is having menstrual problems, it is usually caused by some other issue, not related, except perhaps peripherally, to IBS,” says Dr. Blume.
“What I mean is that the IBS itself is usually not the immediate cause of menstrual problems.
“It would suggest that there is some other issue going on that is not only causing the menstrual abnormalities, but also contributing to that person’s IBS-like symptoms.”
In short, two issues going on at once does not mean there is a causal relationship between the two.
There may be a third issue at hand, causing the first two issues.
For any suspicious gynecological or gastroenterological symptoms, always see the appropriate medical specialist.
The Reverse: Worsening of IBS Symptoms from Menstruation
IBS can become worse during menstruation – according to subjective reports by patients in a study by Whitehead et al.
However, the mechanism – if one even exists – of how a woman’s period can amplify her irritable bowel syndrome process is not known.
Cause and effect, or any kind of direct association between IBS and menstruation is challenging to decipher.
What makes the investigation into this so vexing is that irritable bowel syndrome and the monthly cycle have a symptom overlap.
For instance, the monthly cycle can cause diarrhea and lower abdominal cramps.
It’s also notorious for causing bloating. Some women report constipation as well.
A study in the British Medical Journal found that in women with IBS, menstruation increased rectal sensitivity.
The study authors believe that this suggests that patients with IBS respond differently to the fluctuations in hormones when compared to subjects without IBS.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.