Cardio Exercise for Plantar Fasciitis: 3 Aerobic Routines
I’ve had plantar fasciitis and have discovered that you don’t need to limit your cardio exercise routines to the stationary bike with this painful heel condition.
I used to have a very nasty case of plantar fasciitis in both feet, and my first instinct was to just use the stationary bike until the condition resolved.
But why stop at the stationary bike just because you have plantar fasciitis? If you have this condition, then you know that it comes and goes, often without warning.
If you’ve read up about it, or have seen a doctor, then you also know that stretching the bottom of the foot is one of the treatment modalities for this stubborn condition.
Cardio like jogging, step aerobics, dancing, tennis, jump rope and inline skating are not recommended for people with plantar fasciitis, if for no other reason that these activities can bring on searing heel pain.
However, when I had plantar fasciitis, I discovered that walking uphill made it feel better, and of course, uphill walking is a form of cardio exercise.

Shutterstock/G-Stock Studio
I recommend gentle, slow hiking, and do it nearby your car, in case the plantar fasciitis flares up mid-hike. You don’t want this happening when you’re a mile from your car.
If the pain is bad before you start hiking, postpone it. If it’s mild, proceed slowly, but if it gets worse, turn back and postpone the activity.
Hiking or walking uphill, however, should produce largely benefits for plantar fasciitis, as it stretches the plantar fascia.
Remember, stretching this tissue is what doctors recommend anyways, so why not give it some stretching while at the same time getting in some aerobics uphill?
Try walking slowly using a treadmill incline as well. However, walking uphill on a hiking trail may prove to be more beneficial, since the uneven terrain will cause more stretching and motion of the plantar fascia of the foot.
If you use a treadmill, let your arms swing naturally. Holding on will interfere with a normal gait pattern.
If it hurts to use a treadmill, then postpone this activity.
If any cardio activity aggravates your plantar fasciitis, even the stationary bike, then STOP the activity.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Pamela Au
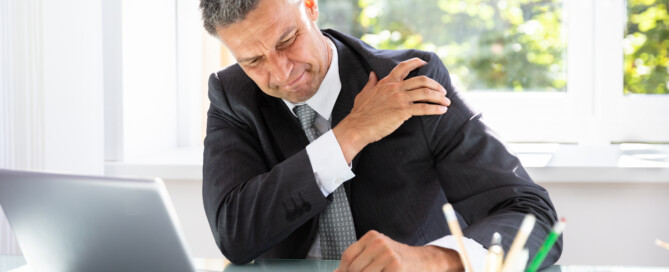
Why an Imminent Heart Attack Causes Shoulder Pain

Ever wonder how a heart attack about to happen can cause shoulder pain?
There are people who’ve experienced recurring shoulder pain thinking it was only a rotator cuff problem or arthritis.
But some of these cases are not caused by a problem in the shoulder joint; they are caused by a problem with the heart: a warning that a heart attack is right around the corner.
“Most commonly, pain of a heart attack occurs in the center of the chest, but may radiate down the left arm into the shoulders, into the throat or jaw, and at times only occur across the shoulders or the upper back,” explains Dr. Ronald Scheib, MD, past Medical Director at Pritikin Longevity Center & Spa in Miami.
“Referred pain is the description of pains caused by internal organs, which are felt at some area distal on the surface.
“That area can be, in the case of heart attacks, jaw, shoulders, chest, upper abdomen, and occasionally in very unusual places, possibly related to an individual’s prior illnesses.”
Does this mean that if you suddenly start developing shoulder pain, that you should rush to the ER to get your heart evaluated?
Pain in this joint is extremely common. As a certified personal trainer, I know this for a fact.
A person must review the entire picture, however, when it comes to shoulder pain.
Do you recall straining the joint recently? Is the pain just like the pain you had when you first strained the shoulder lifting something above your head?
What are your risk factors for heart attack?
A lean person who exercises, doesn’t smoke, sleeps well, limits processed food, has low blood pressure and a normal lipid profile, need not fear an impending heart attack as much as, say, a woman over the age of 50 with excess abdominal fat, who never exercises and has very high triglycerides. This described my mother.
I was alarmed at her triglyceride levels and actually said to her, “You could be dead from a heart attack in six months!”
She went to bed that night worried sick over my comment, but made no changes in her diet after that point, and still refused to exercise.
Recurring episodes of shoulder pain were a common complaint from her, and I never made the connection between these “pain attacks” in her shoulder and the condition of her heart, especially since she had had a total of three surgeries on her rotator cuff.
As a fitness expert, it’s never surprising to me that a senior-aged person, who has never exercised her shoulders, eventually develops problems in this versatile but vulnerable joint.
About four months after I made my comment, I took my mother to the ER for chest pains. The day after that she underwent quintuple bypass surgery.
The surgeon had told me that a “massive” heart attack was imminent, possibly within a week, without the surgery.
Once my mother was recovered from the surgery, she reported that the bouts of shoulder pain had disappeared.
This sounds like more than a coincidence. It has always been the same kind of pain, same general location of the joint.
Dr. Scheib explains, “On occasion, the location may vary based on the specific coronary artery, but in general it tends to be repetitive in the same location.”
 Dr. Scheib passed away in 2018. To Pritikin he brought a career in cardiology spanning four decades, including Miami Heart Institute Chief of the Section of Cardiovascular Medicine, and President of the Medical Staff.
Dr. Scheib passed away in 2018. To Pritikin he brought a career in cardiology spanning four decades, including Miami Heart Institute Chief of the Section of Cardiovascular Medicine, and President of the Medical Staff.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Andrey_Popov
Why a Looming Heart Attack Can Cause Nausea, Vomiting

©Lorra Garrick
Vomiting and nausea can be a sign that a heart attack is imminent.
This is not about an actual heart attack in progress, but vomiting and nausea as a warning sign that a heart attack is in the very near future.
“Nausea and vomiting are very complex interactions between the brain and the stomach,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“The scientific thinking behind myocardial ischemia or infarction associated with nausea relates to the vagus nerve,” continues Dr. Fiocco.
Myocardial ischemia simply means depletion of oxygen to heart muscle. Infarction means tissue death.
The vagus nerve “arises from the brain and travels through the neck, along the esophagus, and gives off nerve fibers to the heart before continuing into the abdomen where it supplies nerves to the stomach,” explains Dr. Fiocco.
“So there is the stomach-heart-brain connection. Why people get nausea prior to a heart attack may be similar to why people get arm, neck or jaw pain rather than chest pain.
“A lot of overlapping circuits may cause the brain to misread the signals, leading to nausea or left arm pain rather than chest pain.”
Of course, being overcome with nausea, as a result of conditions ripe for a heart attack, can then lead to vomiting.
Vomiting was a tip-off to me that my mother might be having a heart attack, or that a heart attack was looming around the corner for her.
She awakened one morning reporting difficulty breathing.
I brushed it off as a panic attack, since trouble breathing is one of a panic attack’s classic symptoms.
She had a history of panic attacks, along with “labored breathing.”
That particular morning seemed like just another panic episode, especially since I knew that about five or six weeks prior, she had quit taking Effexor altogether. Effexor helps suppress panic and anxiety attacks.
I was staying with my parents because my father, just days prior, had back surgery.
About a half hour later I heard my mother call out to my father, “Quick, bring it over here!”
Intuition told me she was referring to a waste can and that she was about to vomit.
I raced upstairs to their bedroom and saw my mother upchucking into a small waste can.
Much of it was dry-heaving, actually, but yellow gunk definitely was coming out.
The bells went off because my mother had never vomited during a panic attack or after one subsided.
Since when did she vomit? I knew that an imminent heart attack can cause vomiting.
She just had a bout of breathing difficulty bad enough to make her weep.
Something told me to get her to the emergency room for a cardiac evaluation.
Two evenings later she was undergoing quintuple bypass surgery – just in time, said the cardiothoracic surgeon; though my mother had not suffered a heart attack, he said that a massive heart attack could have occurred any moment due to severe coronary artery blockage.
In my mother’s case, the vomiting was a sign that something was wrong with her heart, I believe.
Nothing she ate the day prior could explain the upchucking.
She had not been in any pain, either (pain can cause nausea). So in hindsight, it’s logical to conclude that my mother’s pending heart attack caused the vomiting (and difficulty breathing).
Does this mean that next time you feel nauseous or vomit, you should fear imminent heart attack?
Of course not. But take notice of any other symptoms like shortness of breath, trouble breathing, chest pain or tightness, sweating, and pain in the jaw, arm, neck or back that can’t be explained by other benign factors …
… and take into consideration if you have risk factors for a heart attack like smoking, excess weight, lack of exercise, diabetes and a junk food diet. Puking is no laughing matter.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
sscpywrt26
How Dangerous Is Low Blood Pressure? How to Raise It

Chronic low blood pressure may be harmless or extremely dangerous; low blood pressure can cause damage to your organs, not to mention cause you to take a serious fall from fainting.
Low blood pressure is called hypotension, and as mentioned, it can be a harmless condition as well, or cause only mild problems.
Low blood pressure has many causes including heart conditions, nutritional deficiencies and medications. The cut-off for normal BP readings and high readings is 140 over 90.
So when does blood pressure get too low?
“The first question to address is if the blood pressure is really too low,” says Teresa Caulin-Glaser, MD, a cardiologist and senior vice president with Service Lines, OhioHealth.
“In general, if patients are asymptomatic and the systolic (“top number”) blood pressure is approximately 90mmHg or better, you do not need to treat.
“However, if the person is developing symptoms such as dizziness, fatigue, and/or passing out, there needs to be a full history and medical evaluation.”
If you believe your blood pressure is too low, review any medications you’ve been taking.
Explains Dr. Caulin-Glaser: “If the evaluation determines there are no medical problems and/or medications such as diuretics, ace-inhibitors, beta blockers, calcium channel blockers causing low blood pressure and symptoms, then there are non-pharmacologic treatments that can be implemented.”
Other symptoms of low blood pressure: lack of concentration, blurred vision, fatigue, nausea, thirst, cold and clammy skin, and rapid shallow breathing.
A big danger of low blood pressure is organ damage due to insufficient blood supply to them.
As you can see, low blood pressure can present with an assortment of symptoms, while high BP (also known as hypertension), which is a major risk factor for stroke, offers up no symptoms, which is why hypertension is nicknamed “the silent killer.”
So how do you raise low blood pressure that’s creating symptoms?
Dr. Caulin-Glaser says, “Some simple options for treatment are drinking fluids to decrease the risk of dehydration, increasing the amount of sodium in the diet, and decreasing alcohol intake.
“There are medications such as fludrocortisone that can be considered in the treatment of symptomatic low blood pressure, but this would be under the direction of a physician after a full medical evaluation.”
Other causes of low blood pressure: vitamin B12 deficiency causing anemia (result of a vegan diet, since this vitamin is found in animal-derived foods); pregnancy; low blood sugar; severe infection.
The low blood pressure that’s caused by infections of the urinary tract, lungs or abdomen, can be fatal.
(High BP can be life-threatening, but there are natural ways to bring high BP down to normal levels.)
Typically whenever one sees a doctor for any reason, a BP reading is taken. It’s perfectly okay to request that your BP be taken at the conclusion of the doctor visit, because by then, much of your anxiety will be diminished.
Otherwise, your readings may be uncharacteristically high if taken at the beginning of the visit, due to anxiety; this is known as white-coat syndrome.
Low blood pressure has many causes, but if there are no accompanying symptoms, then you need not worry about having BP that is below normal.

Dr. Caulin-Glaser is an experienced physician, teacher and researcher in the specialty of cardiovascular disease, and formerly the system vice president for Heart & Vascular Services at OhioHealth.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/kurhan
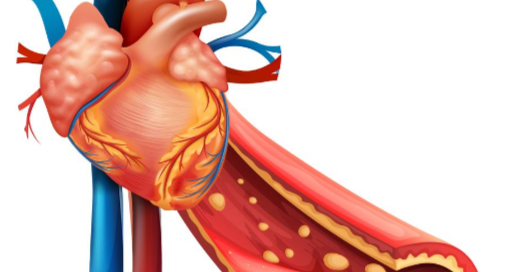
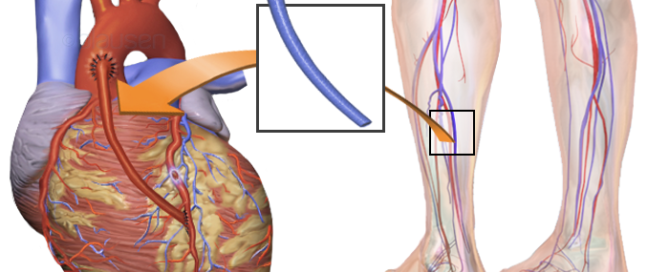
Life Expectancy in Elderly After Coronary Bypass Surgery

The life expectancy (long-term survival) of elderly people after coronary bypass surgery is receiving increasing attention, since the population of advanced age people is ever-growing.
This means more and more elderly people, including octogenarians, are having coronary bypass surgery (a.k.a. CABG).
“Life expectancy after CABG is difficult to determine because so many factors are involved,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital, one of the nation’s top 50 heart hospitals.
And this applies to the elderly population.
“Mortality within 30 days of CABG is less than 2 percent, and that is including some very sick patients undergoing CABG,” says Dr. Fiocco.
When an elderly person has coronary bypass surgery, other factors still remain an important part of the life-expectancy equation:
In other words, the CABG and post-op may have gone without a hitch, but an elderly individual inherently is at risk for other serious conditions such as cancer, Alzheimer’s disease and dying in a car accident that otherwise would result in only moderate injuries for someone much younger.
Thus, the question of “What is the life expectancy for the very old patient after coronary bypass surgery” almost doesn’t seem to make a lot of sense.
Again, this is about life expectancy, rather than a more immediate survival rate.
Once the elderly patient is out of the woods in terms of possible post-op complications (e.g., internal bleeding, pneumonia, infection, stroke), the life expectancy is extremely variable.
But of course, it’s within the confines of how much longer any 80-year-old (CABG or not) is expected to live.

For elective coronary bypass surgery (meaning, it’s not performed on an emergency basis), the mortality rate falls below 1 percent 30 days post-op.
Dr. Fiocco explains, “Life expectancy beyond that is determined by so many factors it is hard to quantify.
“Was the patient 50 years old when the surgery was performed or 80?
“Did the patient stop smoking?
“Change their diet?
}Exercise regularly?
Control blood sugar levels after CABG or did they continue in the ways that led them to surgery in the first place?”
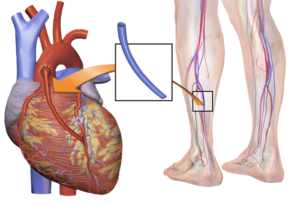
Though the patient’s new “plumbing” consists of cleaner veins harvested from either the leg or arm, to replace the clogged, plaque-caked coronary arteries, don’t assume that the elderly patient can get away with bad health habits — with the idea that it will take another 20 years for the grafted blood vessels to develop severe blockage —
— so why bother being health-conscious if the patient would have to live to 100 or older by the time another bypass surgery is needed?
Well, here’s the deal:
The grafted vessels are veins from the legs and arms; they were not designed by nature to endure the blood pressure forces that coronary arteries are!
They aren’t as durable, and if the patient takes excellent care of his body, the replacement vessels should last 10-15 years.
So imagine the potential disaster if the elderly CABG patient fails to quit smoking or lose weight, and/or won’t stick to an exercise program and eat healthfully!
The plaque-buildup rate in the grafted veins that came from the leg or arm is much faster than the plaque-buildup rate in coronary arteries.
Dr. Fiocco adds, “A large study did show average life expectancy after CABG was approximately 17 years, but this was from the 1980s and it is likely even higher now.
“Again, what determines anyone’s life expectancy after CABG is what got you there and what you change going forward.”

Shutterstock/Interpass
Some elderly coronary artery bypass patients will continue living on a food pyramid whose bottom tier is comprised of foods that damage the heart.
They will also continue to avoid exercise and maintain other habits hazardous to the heart.
And likewise, other elderly coronary bypass patients will completely overhaul their lifestyle habits:
Quit smoking, lose weight, avoid trans fats and limit saturated fats, take up aerobic and strength exercise, practice better stress management and be compliant with appropriate medications.
It’s intuitive who will have the much longer life expectancy.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
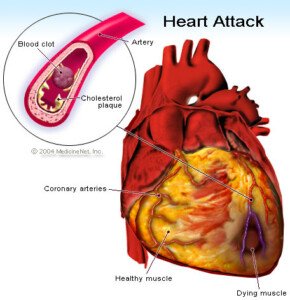
Does Normal Blood Pressure Mean You Don’t Have Heart Disease?
The answer is NO!
In fact, you can have life-threatening heart disease — extensive coronary artery blockage — and still have consistently normal blood pressure readings.
“High blood pressure (Htn) causes the occlusions (blockages), but occluded arteries do not cause Htn,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Blood pressure can be normal even in patients with severe coronary artery disease because they still may have diabetes, elevated cholesterol, genetic abnormalities, and/or a smoking history, all of which can cause coronary artery disease.
“But sometimes the blood pressure is normal.”
In fact, you can have 97 percent blockage in your coronary arteries – an emergency situation – yet have perfectly normal blood pressure.
This was the case with my mother. She faithfully took her blood pressure almost daily with a home device, and the always-normal blood pressure readings gave her peace of mind when it came to her heart health.
However, little did she know that her coronary arteries were becoming dangerously blocked. In fact, the catheter angiogram report said “sub-optimal occlusion.”
The heart surgeon told me this meant about 97 percent blockage. He took one look at the angiogram and decided that my mother needed quintuple bypass surgery ASAP; about two hours later she was wheeled into the operating room.
Yet right up to that point, her blood pressure was in the normal range. So if you have good blood pressure readings, don’t be fooled and think you can’t possibly have heart disease.
Though high blood pressure (hypertension) is one of many risk factors for heart disease, the absence of hypertension does not in any way get you off the hook from America’s #1 killer of both men and women.
Other factors can cause heart disease even if you have normal blood pressure:
1) Lack of structured exercise
2) Poor diet such as high sodium
3) Smoking
4) Overweight/BMI greater than 25
5) Chronic emotional stress
6) Insomnia/sleep deprivation/sleep apnea
7) Sleep exceeding 9 hours/day including naps
8) Family histor
9) Diabetes/prediabetes
10) Poor cholesterol profile. Do you have any of these risk factors for heart disease?
So don’t be deceived by normal or low blood pressure readings.
The risks of heart disease are numerous, and the absence of one of these risk factors in no way means you can’t possibly have dangerous blockage in your coronary arteries.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Images: vecteezy.com
Coronary Bypass Surgery Post-op Complications that Seem Scary
If a loved-one has coronary bypass surgery, you as the visitor may become aware of a lot of interesting things that occur post-op.
Some of these will be considered “complications,” and they may seem very alarming, when in fact, they’re not as bad as they seem.
Atrial Fibrillation
The first complication that my mother had, while in the ICU after coronary bypass surgery, was “A-fib.”
You, as the visitor, will become aware of this when the heart rate monitor starts giving off a warning beep.
The monitor should be silent otherwise, so the sudden beeping will get your attention and be scary.
Staff will rush into the room and may awaken the patient if the patient is asleep during this event.
The first time my mother went A-fib, staff cleared her gown from her chest and attached monitors. This indeed looks frightening to the onlooking family member.
You may hear a nurse contacting a doctor by phone, describing the event and asking for directives.
You may see an EKG report being churned out of a computer and staff examining it.
And you will see, on the heart rate monitor, the heart rate continuously bouncing all over the place in the high range.
You will hear the word “A-fib” more than once being spoken. You may also remember that the heart surgeon told you, pre-op, that one possible complication of coronary bypass surgery is atrial fibrillation.
And you will remember, as I did, that the surgeon said it could easily be controlled, and that the more serious complication is ventricular fibrillation (V-fib).
Nevertheless, witnessing my mother’s first A-fib was nerve racking. So was the second one.
But each subsequent one was less alarming; you will notice that staff increasingly acts more casually, and that no doctors are present: a good sign.
You’ll learn that drugs control the situation, and that sometimes, the patient will spontaneously “pop out” of A-fib and the heart rate will return to normal.
If you witness several A-fibs, you’ll become very sensitized to the heart rate monitor’s distinctive beeping.
So that when you hear the monitors of other patients start beeping, you may have a conditioned response of anxiety and your own racing heart. Over time you’ll become desensitized to the beeping.
Kidney Function
Coronary bypass surgery may affect kidney function. A kidney doctor was called in to see my mother and explained she had mild kidney failure, and that they’d be just “watching it for now.”
Coronary bypass surgery causes the kidneys to be shorted of blood, and hence, they may “fail.”
The “failure” may only be mild, and is measured by a daily creatinine test. The doctor will be on top of this to see if the number gets above a certain value.
In the meantime, treatment will include fluid restriction.
The worst case scenario impression that I got was that if the kidneys didn’t “bounce back,” my mother would need dialysis. No mention of possible kidney transplant was ever made.
Mental State
The coronary bypass patient (or other type of surgery) may be delirious or confused even several days out from surgery; a definite alteration in normal mental status.

Shutterstock/Volodymyr Baleha
My mother thought I was her other daughter, for instance. Assume that off-the-wall comments, oddball questions and bizarre observations are the results of lingering anesthesia and/or the effects of powerful painkillers.
Chest Pain
The coronary bypass patient may complain of agonizing pain, particularly in the chest.
Don’t assume the patient is having a heart attack. Instead, remind yourself that the patient was very recently cut open in the chest.

Opening the chest. Shutterstock/sfam_photo
Complaints of severe pain may also center around the belly – where tubes will be inserted.
Very Swollen Legs
The coronary bypass patient will have significant visible swelling and bruising, especially in the legs if veins were harvested from the legs for the coronary artery grafting. This isn’t pretty, but it’s normal.
The coronary bypass patient will have fluid in the lungs; this is normal and is called pulmonary edema.
Fluid in the lining of the lungs, called pleural effusion, is also normal.
Drugs called diuretics treat this post-op condition.
Coronary bypass surgery is very frightening, but extremely lifesaving.
Enough visits to the coronary bypass patient and you’ll become acquainted with different kinds of beeping sounds that hospital equipment makes.
You may then develop a conditioned response of anxiety every time you hear things in daily life beeping, like your car when the seatbelt isn’t put on.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Blausen Medical Communications, Inc.
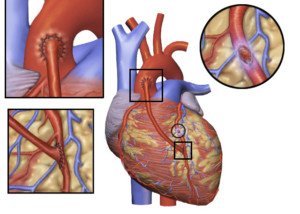
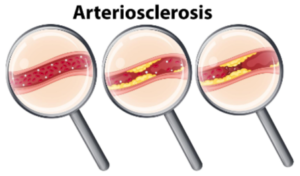
Can Stress Test Miss Severely Blocked Coronary Arteries?

If your stress test was normal, does this mean you can’t possibly have severely blocked coronary arteries?
How much faith should you put in the cardiac stress test?
“A stress echocardiogram or a nuclear stress test are each about 90 percent accurate in correctly identifying a severe coronary blockage, i.e., at least one of the coronary arteries has a narrowing greater than 70 percent).,” explains Dr. Larry Santora, MD, a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
“However about 10 percent of the time it will miss the blockage, and the stress test will be ‘falsely negative’,” explains Dr. Santora.
“These false negative stress tests are more common in women.
“It is more common to have a false negative if the blockage is in the circumflex artery which, on the back side of the heart, is more likely to be missed since it tends to be a smaller artery, and rarely, even if all three arteries are equally blocked (called ‘balanced ischemia’).”
The possibility of false negatives got me wondering, then, about someone with a high coronary calcium score who has a normal stress test.
They may worry that they might be in that 10 percent in which the test results are not accurate.
Dr. Santora explains, “There is no test in medicine that is 100 percent accurate; not a mammogram or colonoscopy, etc.
“If you have a high coronary calcium score and you are asymptomatic (no chest pain), and your stress test is normal, the probability of a severe blockage (meaning a narrowing more than 70 percent in one of the major coronaries) at that time is very, very low.
“If the patient had symptoms, even if the stress test is normal, then the chance of a severe blockage is perhaps 25 percent, and another test is needed, maybe a CT angiogram.”
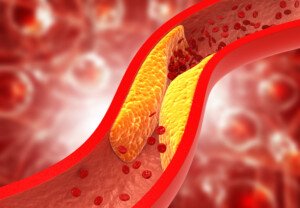
The CTA will reveal amount of soft plaque versus hard (stabilized) plaque.
Soft plaque can rupture and block an artery.
Shutterstock/OSweetNature
“Anyway, it is the CAC that tells you if you need an aggressive approach to lower cholesterol and other risk factors,” says Dr. Santora.
So if you had a high coronary calcium score and normal stress test, this does not excuse you from taking aggressive measures to improve the state of your coronary arteries.
“The high coronary calcium score tells you that you must take aggressive risk reduction measures,” continues Dr. Santora.
“You cannot put full faith in a stress test. But some 90 percent blockages in the more distal ends (towards the end of the artery) can be treated without surgery or a stent, with risk modification.
“In these there can be plaque stabilization or some reversal, and the development of collaterals; that is, new arteries grow from a normal coronary over to the artery that is blocked.
“This can be promoted by exercise and external counterpulsation.”
If one’s coronary calcium score is deemed too high to allow a CTA image to be read (usually over 800), then Dr. Santora says, “You can still feel comfortable if you have no symptoms and a normal stress test, with vigorous risk modification.”
Modification would mean exercise, change in diet (e.g., severe restriction of refined carbohydrates and sugars, as well as saturated and trans fats), supplements and perhaps a pharmaceutical agent.
If the stress test is not clear, and you have a very high CAC, “then do an invasive cardiac catheterization and coronary angiogram,” says Dr. Santora.

Dr. Santora’s areas of interest include interventional cardiology – coronary stenting; cardiac CT – CT angiography, and coronary calcium screening with EBCT. He is board certified in cardiovascular disease and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Djohan Shahrin
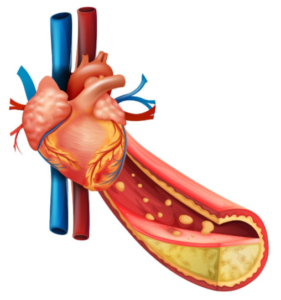
How to Make Diet Reverse Soft Plaque Buildup in Your Heart
There IS a way to make diet reverse the sludge plaque buildup in your heart’s arteries.
This dietary approach is not complicated. Coronary arteries are prone to getting clogged.
“Soft plaque can certainly be reversed, and so can some of the smaller areas of calcium,” says Dr. Larry Santora, MD, a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
There are two kinds of plaque buildup in coronary arteries: soft and hard.
The soft plaque is the dangerous kind that can rupture and cause a heart attack (a fragment of this soft plaque breaks away from its base and travels through the coronary artery, blocking blood flow)
When someone has harmful levels of soft plaque, the goal is to stabilize this soft plaque.
Dr. Santora explains, “This means the plaque becomes more adherent to the inner vessel wall, and the cap on the plaque becomes stable and less likely to rupture.
“This occurs as soon as diet and medications are instituted, even before the cholesterol levels change.”
The diet for reversing coronary soft plaque is not a temporary diet; it is a permanent diet.
Dr. Santora says, “If you eat well 90 percent of the time, that is a reasonable way to go. So as a rule of thumb, all high glycemic foods like white bread, white rice, can be eaten, but only 10 percent of the time.”
The glycemic value of a food is a numerical measurement of how quickly its carbohydrates (sugars) are absorbed into the bloodstream after being eaten.
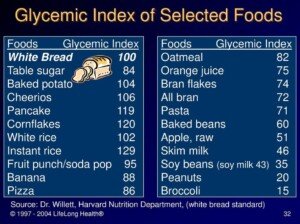
White sugars and simple, processed carbohydrates like white flour impose a terrible burden on the coronary arteries if eaten too often.
This means the occasional Boston cream pie is permissible, but knock out the white rice if you eat rice often; eat wild, basmati or brown rice instead.
Do you eat cereal every morning or most mornings?
It should be whole grain with no sugars added, and this includes high fructose corn syrup.
White flour is a ubiquitous food ingredient. Read ingredients lists. “Sugar” also shows up everywhere, including salad dressings and soups. Every “little bit” adds up.
What about whole eggs? Will whole eggs disrupt one’s dietary plan of reversing soft plaque?

Freepik.com
“As far as eggs go, they are now considered health foods; eating one or two per day, if not fried, are healthy since the cholesterol in eggs is not converted to cholesterol in the bloodstream,” says Dr. Santora.
What about going by the USDA Food Pyramid?
The food pyramid is ambiguous in that it names only food groups. At the bottom of the food pyramid are breads, for instance.
This does not mean make a staple out of a highly processed bread product like Wonder bread, bagels, English muffins or pancakes.
In fact, just about all commercial breads are full of synthetic chemicals; many contain high glycemic carbohydrates like molasses, corn syrup and even sugar.
Even breads at so-called health food stores may contain these heart-unhealthy items. Read ingredients lists.
The food pyramid doesn’t differentiate between carbohydrate sources and does not show information on “bad” fats.
A pancake mix labeled as “whole wheat” may still contain partially hydrogenated oil, which is a very bad fat: a trans fat.
So as far as the food pyramid, Dr. Santora explains, “The food pyramid is fine as long as the carbs are the good low glycemic type, and the fats are the good fats like monosaturated fats, and no trans fats. Simply avoid cookies, crackers and chips.”
A “little bit” (of a bad thing) can indeed hurt, because “a little bit” often morphs over time to a lot of “little bits.” Remember the 90 percent rule.
In order for diet to halt soft plaque progression, or even reverse soft plaque levels, you must not adopt an “a little bit won’t hurt” mindset.

Dr. Santora’s areas of interest include interventional cardiology – coronary stenting; cardiac CT – CT angiography, and coronary calcium screening with EBCT. He is board certified in cardiovascular disease and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Explode
How to Lower Your Coronary Calcium Score

Yes, it’s possible to actually lower your calcium score–the number that’s calculated from a CT scan of your heart’s coronary calcified plaque.
You may have been led to believe that coronary calcium score cannot be lowered; that the coronary calcium score progression can only be slowed down, or at best, halted.
But according to cardiologist Larry Santora, MD, you can, indeed, lower your calcium score.
“Yes, you can reverse the plaque,” says Dr. Santora,a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
To achieve this, it’s through commitment to:
- A “clean” diet
- Exercising daily
- A statin drug
- Certain supplements
Sounds simple, right?
Well, it’s not as straightforward as you may think.
The statin part of lowering calcium score is as simple as taking it as prescribed.
Same with the supplements that are known to potentially lower calcium score and benefit heart health.
The confusion is with the diet and exercise part.
I can’t begin to tell you how many people whom I’ve encountered — including clients when I was a personal trainer — who truly believed they had a “healthy diet” — but just the opposite was true.
A perfect example of this is my mother. She was floored upon being told she needed emergency quintuple bypass surgery.
“How could this have happened to me?” She kept asking.
“I’ve always ate a healthy diet,” she’d say. “I’ve been on the Mediterranean diet! I’ve always been active!”
My mother has never had a coronary calcium score test; she had a catheter angiogram.
I can assume that had she had a calcium score test, the result would have been a very high number.
Re-evaluate your understanding.
Do YOU think you’re on the Mediterranean diet because you cook your white rice with olive oil, or because you dip potato chips in yogurt, or because you eat a daily salad with dressing that contains added sugar?
Is your idea of aerobic exercise doing housework and walking about at Walmart?
The calcium score can be lowered, says Dr. Santora, but not without pinpointed changes in diet and exercise habits.
Lowering Your Coronary Calcium Score

G.steph.rocket, CreativeCommons
Think whole foods in their natural state.
Not foods that come in a box, can or bag. Exceptions are all-natural whole grain foods, or the actual grains, that are sold in plastic bags.
• Go very light on red meat and eat only grass-fed beef; grain-fed beef contains a lot of “bad” fats.
• Replace chicken from frozen dinners with whole chicken.
• Eat a lot of wild-caught fish.
• Don’t even look at processed meats.
• Eliminate foods with white flour, high fructose corn syrup and sugar.
• Avoid partially hydrogenated vegetable oils.
• Eat as many raw vegetables as possible and snack on fruit.

• Adherence to such a drastic change in lifelong eating habits can be very daunting for most people.
If this means occasionally indulging in a single serving of forbidden foods (e.g., candy, cake, a donut, slice of pizza, pretzels) to prevent burning out from the natural diet, then do so…with control.
For many people, 100 percent elimination of favorite foods is simply not possible.
Otherwise, battling to achieve this could collapse their discipline.
Embrace Exercise
Exercise should include strength training (e.g., weight machines, free weights, tension tubing) and cardio workouts (e.g., group fitness classes, hiking, jogging, martial arts, inline skating).

Shutterstock/Straight 8 Photography
A lengthy visit to Costco does not replace your exercise session for that day.
Supplementation
Supplements that will help lower calcium score (in combination with the other lifestyle changes just mentioned) are niacin (vitamin B3) and vitamin D3, along with magnesium citrate, turmeric, green tea, aged garlic extract, fish oil and plant sterols.
Though there is some controversy over whether or not some of these supplements actually aid in lowering calcium score, there are plenty of studies (e.g., Malinski et al, Kuriyama et al), showing that all of these supplements are very beneficial to heart health.
Dr. Santora says, “I had my first heart scan in 1999, and then every two years since, and have had a reversal of some plaque.
“But remember, you do not have to reverse the plaque; you just need to stabilize the plaque so that it does not rupture.
“Studies [e.g., Journal of the American College of Cardiology, March 26, 2013] show that if the plaque does not progress more than >10 percent per year; the chance of a heart attack is low.”
If you’ve never had your calcium score taken, this is something you’ll want to consider — depending on your risk factors for coronary artery disease and your age.