Can Celiac Gene Raise Cancer Risk if You Don’t Have Celiac Disease?

Celiac disease specialist, Dr. Stefano Guandalini, addresses the cancer issue.
You may know that having celiac disease increases your risk of developing intestinal cancer.
This is because as celiac disease progresses, the damage to the inner lining of the small intestine progresses, making it more vulnerable to cancer.
I wondered, however, if merely having the gene(s) for celiac disease could somehow raise the risk of cancer.
The gene(s) for celiac disease has been identified, and if you do not have the gene, you cannot get CD.
However, having the gene does not guarantee you will develop this illness, either, which is when the body mounts an ongoing immune response to the consumption of gluten-containing foods.
So does having the celiac gene, in and of itself, predispose a person to a higher risk of cancer?
“It does not appear that this is the case; there is in fact no evidence that intestinal malignancies occur more frequently in people with only the gene(s),” says Stefano Guandalini, MD, Founder and Medical Director, The University of Chicago Celiac Disease Center.
Mayoclinic.com states: People with celiac disease who don’t maintain a gluten-free diet also have a greater chance of getting one of several forms of cancer, including intestinal lymphoma and bowel cancer.
Suppose you find out that you have the genetic predisposition to CD, but you are not experiencing symptoms of this disorder, which include digestive disturbances such as diarrhea; joint pain; mouth sores; muscle cramps; tingling in the feet and legs; anemia; unexplained weight loss; nausea/vomiting; constipation; chronic diarrhea; brain fog; fatigue and grayish stools. Should you go gluten-free?
Most people with celiac disease do not have symptoms, so if you have the gene(s) for this condition, yet feel perfectly fine, the illness may still be in full swing. And in that case, you do have a heightened risk for certain cancers.
If you have the gene for celiac disease yet no symptoms, it would not be practical, at that point, to eliminate gluten-containing foods.
After all, only about 5 percent of people with the gene actually develop CD.
“First-degree relatives of those with biopsy-diagnosed celiac disease who have the genetic predisposition are a high-risk group that should be screened every three years or immediately upon symptoms,” says Dr. Guandalini.
An antibody blood test called transglutaminase is used for screening. But in rare cases, this test can be negative in someone who has the illness.
The gold standard for diagnosis is an endoscopic biopsy of the small intestine.
You will need to discuss your options with a gastroenterologist, especially if family members have celiac disease.
 Dr. Guandalini is an internationally recognized expert on celiac disease, Professor Emeritus, University of Chicago, and the founder of the University of Chicago Celiac Disease Center. His clinical and research efforts have greatly influenced how celiac disease is diagnosed and treated today.
Dr. Guandalini is an internationally recognized expert on celiac disease, Professor Emeritus, University of Chicago, and the founder of the University of Chicago Celiac Disease Center. His clinical and research efforts have greatly influenced how celiac disease is diagnosed and treated today.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/KongNoi.
Sources: mayoclinic.com/health/celiac-disease/DS00319/DSECTION=complications; mayoclinic.com/health/celiac-disease/DS00319/DSECTION=symptoms
Sjogren’s Syndrome: How Common Are Memory Problems?

How many people with Sjogren’s syndrome suffer memory problems?
Sjogren’s syndrome indeed can cause memory problems, even though this autoimmune condition is associated with dry mouth and dry eyes.
Because Sjogren’s (pronounced show-grens) syndrome is potentially systemic, the entire body can be affected, including organs, and this can mean the brain.
“Patients with Sjogren’s syndrome may suffer from a number of different neurologic abnormalities,” says Ali D. Askari, MD, Professor of Medicine – Case Western Reserve University; Chief, Division of Rheumatology – University Hospitals Case Medical Center; Director, Rheumatology – University Hospitals Case Medical Center.
Rheumatologists often deal with Sjogren’s syndrome patients, since the disease often initially manifests with joint pain or stiffness.
Dr. Askari continues, “Unlike lupus (another autoimmune disorder which can affect the joints), which has more of central nervous system involvement, Sjogren’s syndrome has peripheral nerve involvement more commonly.”
Neurological problems affect as many as 20 percent of patients. However, Dr. Askari says that dementia is a rare complication of Sjogren’s syndrome.
“In our own study reported to the international SS conference in Japan, we found 14 of 200 patients having neurological abnormality.
“Six had variety of central nervous system involvement; only one had dementia. Dementia therefore is rare and can happen at any time.”
Though Sjogren’s syndrome is most associated with dry eyes and dry mouth, these aren’t necessarily the first presenting symptoms.
The very first symptom may be dementia, though, again, it’s a rare complication.
Dr. Askari continues, “The abnormalities of the central nervous system include abnormal MRI without any abnormal serologic findings, but also brain abnormalities such as shrinking of the brain and dementia.”
It’s possible for a person diagnosed with Alzheimer’s disease, which is terminal, to actually have Sjogren’s syndrome, which is not terminal if treated and managed.
“Although this is difficult to differentiate from Alzheimer’s disease, neurologists believe that the cerebrospinal fluid contains a specific protein found mainly in Alzheimer’s.
“This protein is called Tau which is not found in Sjogren’s syndrome and dementia.
“Fogginess and slight memory loss can happen in both systemic lupus and Sjogren’s syndrome, and may respond to anti-inflammatory medicines; if not it may be associated with permanent brain changes.”
Dr. Askari adds, “The peripheral nerve involvement as mentioned is more commonly associated with Sjogren’s syndrome and that includes peripheral neuropathy or injury to the nerve fibers of the lower or upper extremities.
“In particular pure sensory neuropathy, meaning that just lack of sensation found by nerve conduction tests (EMG), is specific for Sjogren’s syndrome.”
High doses of corticosteroids and other immunosuppressant drugs, when administered early in the course of these symptoms, can bring on improvement.
If you’re suffering from what seems to be neurological or memory impairment, request tests for SS.
Dr. Askari explains, “It is prudent to consider Sjogren’s syndrome in the differential diagnosis of neurologic abnormalities and particularly abnormal findings on MRI of the brain or spinal cord, or peripheral neuropathy.”
Update: As of April 2024, Sjogren’s syndrome is now known as Sjogren’s disease.
Dr. Askari’s special interests include diseases of the muscles, fibromyalgia, general rheumatology, lupus and Sjögren’s syndrome.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Shutterstock/Vadim Zakharishchev
sscpywrt26
Does Sjogren’s Syndrome Shorten Life Span?

How much does Sjogren’s syndrome affect life span?
Sjogren’s syndrome may bring to mind simply that of chronic dry mouth and dry eyes, which don’t sound too serious.
Many people with Sjogren’s syndrome suffer only from dry mouth and dry eyes, and often experience joint pain.
However, some patients with Sjogren’s (pronounced show-grens) suffer more serious complications of this autoimmune disorder, which affects about two to four million Americans, with 90 percent of patients being female (for reasons not known).
Since Sjogren’s syndrome often affects joints, specialists in this disease are usually rheumatologists.
“Rheumatic diseases by in large cause pain and stiffness and don’t impose death threats,” says Ali D. Askari, MD, Professor of Medicine – Case Western Reserve University; Chief, Division of Rheumatology – University Hospitals Case Medical Center; Director, Rheumatology – University Hospitals Case Medical Center.
“In general, inflammatory states such as rheumatoid and lupus lead to more coronary artery disease and short life span.
“In Sjogren’s syndrome this matter is not settled (not well-studied), and the disease in general is benign but annoying, and people have their regular life expectancy. By-and-large patients without complications live a normal life.”
However, living with just dry mouth and dry eyes can be arduous.
The reduced saliva flow predisposes a patient to:
- a high risk of dental decay
- bad breath
- chapped lips
- and a burning sensation in the lips, tongue and throat, not to mention difficulty swallowing food that necessitates sipping water before every mouthful of food.
Dr. Askari continues, “The development of lymphoma (cancer) occurs in less than 5 percent of patients having SS in which the life expectancy shortens.
“The undesired complications with Sjogren’s syndrome include a renal condition referred to as renal tubular acidosis in which more kidney stones are formed.
“Kidney failure, however, is rare and is due to inflammation of the cortex of the kidney, unlike lupus in which this complication is more frequent.”
Lupus is also an autoimmune disease that can affect the entire body.
“Patients with Sjogren’s syndrome could have lung inflammation with cough and shortness of breath which could affect life span expectancy.
“The most important rare complication in Sjogren’s syndrome is the inflammatory changes of the vessel walls, or vasculitis, which leads to the presence of a rash on the skin, and inflammatory changes within the different organ systems such as the kidneys, lungs and brain.
“In each complication mentioned, however, there are sufficient treatments available, which are effective and control the complications.”
Update: As of April 2024, Sjogren’s syndrome is now known as Sjogren’s disease.
Dr. Askari’s special interests include diseases of the muscles, fibromyalgia, general rheumatology, lupus and Sjögren’s syndrome.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick sscpywrt26
The Youngest a Child Can Get Melanoma Skin Cancer?

How young is too young for a child to get melanoma?
Children CAN develop melanoma — the deadliest type of tumor that can arise from a type of skin cell known as the melanocyte: a pigment producing cell.
“There is no age that is too young to develop melanoma as a child,” says Dr. Joel Schlessinger, MD, a dermatologist with a private practice in Omaha, NE.
“In my practice I have seen melanoma in many young patients and have one 17-year-old who nearly needed to have an amputation due to melanoma of the toe.”
What’s with the increase in melanoma cases in younger and younger people, including children?
This seems to contradict our evolutionary biology; after all, ancient man spent hours every day smack in the sun, before umbrellas, tents, wide-brimmed hats and sunglasses were invented.
Researchers point to the intermittency of sun exposure as a risk factor for melanoma.
Intermittent blasts of sun exposure shock the DNA and damage it, causing changes that can, over time, give rise to melanoma.
Dr. Schlessinger continues, “Sadly, we are now seeing a huge spike in melanoma cases due to indoor tanning and the trend of tanning before proms, weddings and all other events.
“Additionally, damage to the skin as well as moles is being done on a daily basis when going to tanning booths.”
Tanning booths are not safer than the sun; in fact, their dose of radiation is much more concentrated, which is why you can get burned in just five minutes.
“Moles often go through a process whereby they change from innocent moles to more concerning moles over time,” says Dr. Schlessinger.
“Eventually, many moles become what is called ‘dysplastic’ or unusual under the microscope and to the eye.
“These moles can ultimately end up turning into melanoma, but they don’t have as great a chance if the skin is protected.”
There is a strong correlation between childhood protection from the sun, and low incidence of melanoma later in adulthood, as well as during childhood.
Next time you’re tempted to encourage your pasty-faced child to “get more sun,” think of “get some color in your skin” as synonymous with “get some melanoma in your skin.”
Moles that are present since birth are more likely to develop melanoma, says Dr. Schlessinger.
If your child has congenital (since birth) moles, this doesn’t mean they all must be removed.
However, the parent should keep a close watch on these moles in their child for any signs of melanoma.
Don’t obsess and live your life in fear, though. Just make sure you know your child’s moles, and have a dermatologist evaluate them once every year or two.
“Dermatologists frequently encounter moles that are ‘on the fence’ and at that time may choose to either carefully observe them or remove them,” continues Dr. Schlessinger.
“There are some moles that are both congenital and quite large that simply can’t be removed.
“These are frequently the ones that are the most concerning of all and need to be evaluated on a yearly basis.
“Dermatologists may look at parts of them by biopsy or perform a small incision to test them.
“Additionally, there are tools to magnify the mole without having to do a biopsy, known as dermoscopy.
“Many dermatologists have these tools and can perform an initial evaluation of the mole using this technology.”
All in all, melanoma is still very rare in children, but this rarity is no consolation to parents who find out that their child has melanoma, especially when the disease was caught later, rather than sooner, when it was much more treatable, even curable.
 Dr. Schlessinger, founder of LovelySkin.com, has 25+ years of experience treating many skin conditions including melanoma. He’s founder of the Advanced Skin Research Center, a clinical facility that investigates new medications and treatments.
Dr. Schlessinger, founder of LovelySkin.com, has 25+ years of experience treating many skin conditions including melanoma. He’s founder of the Advanced Skin Research Center, a clinical facility that investigates new medications and treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Andrey_Popov
Are Teens Really at Risk for Skin Cancer from Tanning Beds?

Teens who use tanning beds increase their risk of deadly melanoma skin cancer risk.
More and more teens are using tanning beds, such as in about a million visits daily in the U.S.
Using a tanning bed before age 35 increases risk of melanoma skin cancer by up to 75 percent, says a study reported in the March 2007 International Journal of Cancer.
Does your teen use a tanning bed?
The most significant known risk factor for this cancer is the unprotected exposure of the skin to ultraviolet light – essentially the modus operandi of a tanning bed,” says George Hollenberg, MD, a dermatopathology specialist in Plainview, NY, and former medical director of Acupath Laboratories.
Melanoma rates in the U.S. continue to rise, relative to the increasing population, and these increased rates have particularly occurred in children and young adults.
Dr. Hollenberg says, “Melanoma diagnoses are increasing at a rate of 3 percent each year for children ages 10-19, and more rapidly for young women in their 20s and 30s.” Melanoma is the leading cause of death for women 25-29.
And here’s more frightening news, from the American Academy of Dermatology: The Academy predicts that by 2025, melanoma may be the # 1 cause of cancer death for Americans. Even naturally dark people can get melanoma.
As a responsible parent, you certainly care about your teen’s teeth; his or her posture; and perhaps you’ve ordered your kids to eat their vegetables. Why not include melanoma awareness in your parenting program?
Over two dozen states actually restrict access by teenagers to tanning salons.
This restriction ranges from the requirement that teens have parental consent to use the tanning bed, to absolute prohibition of teens using tanning facilities.
It’s tough to make a stubborn teen start wearing sunblock for the very first time in his or her life.
But don’t let that stop you from enforcing its use. If your kids are very young, you have a far better chance of ingraining the sunblock habit into them.
Every so often, I see very young children with sunburns. This is inexcusable.
According to the Centers for Disease Control, only one in seven high school students reported using sunblock rated at least SPF 15.
You make your children brush their teeth every morning and every night before bed. Well, every morning make them put on sunblock, or, put it on them yourself.
If you require your kids to do yard work, send them out before 10 a.m. or after 3 p.m.
Yes, you need to get serious about this, because the National Cancer Institute says that melanoma is one of the fastest-spreading cancers.
How familiar are you with the moles on your kids’ or teens’ skin?
How familiar are THEY with them? I have two young nephews and a niece who are full of moles.
All three are dark from spending huge amounts of time in the sun without sunblock. Having over 100 moles is a significant risk factor for melanoma.
My 14-year-old nephew has a ton of moles on his bronzed back, and he’ll undoubtedly acquire more before age 20.
Your teens should be familiar with their moles, so that if one ever starts changing, they will know it.
Melanoma can also arise from non-mole areas of the skin. If you find a suspicious growth on your child or teen’s skin, don’t wait:
Take him or her to a dermatologist and insist on a biopsy.
Dr. Hollenberg passed away in 2013.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Melanoma Sentinel Lymph Node Biopsy Technique Eliminates Second Surgery

A second surgery for sentinel lymph node removal, if you’ve just been diagnosed with melanoma, may not be necessary, if your doctor knows about the MCW Melanoma Cocktail.
As a new skin cancer patient, you may already know that a sentinel lymph node biopsy might be in order, to see if any melanoma cells are in nearby lymph nodes.
Key to five-year melanoma survival rate is the ability to detect metastasis in a fast, accurate manner.
The quicker that melanoma is “staged,” the sooner doctors know precisely what the treatment protocol is.
Acupath Laboratories has a technology that eliminates the need for a second surgery for newly diagnosed melanoma patients.
Not only is a second surgery eliminated, but the technology eliminates the 1-2 days’ anxiety that the patient must suffer awaiting results of the sentinel lymph node biopsy.
Depending on how “deep” the tumor is in the skin, the biopsy will be required.
The routine protocol for this consists of the initial surgery to remove the melanoma tumor, and then a biopsy of the sentinel lymph nodes is taken.
However, it takes 24-48 hours for the results of the sentinel lymph node biopsy to come back. During that time, the patient must endure anxiety.
Furthermore, if the biopsy of the sentinel lymph nodes comes back positive for melanoma cells, the patient must then return to the doctor for additional surgery, to remove the surrounding nodes.
With Acupath’s MCW Melanoma Cocktail, it can be determined, right then and there during the first surgery, if the sentinel lymph nodes test positive for cancer cells.
The MCW Melanoma Cocktail was developed by researchers at the University of Wisconsin.
- The MCW Melanoma Cocktail mixes together several antibodies that can detect cancerous cells in the sentinel lymph nodes.
- The surgeon takes tissue from the patient’s sentinel lymph nodes, during the first surgery to remove the malignant spot.
- The tissue is placed on slides; and the antibody mixture is applied to this tissue on the slides.
Because the mixture can detect cancer cells within 30 minutes, any need to remove the sentinel lymph nodes for additional study can be done right there, during the very same surgery.
“Surgeons and pathologists can now determine in the operating room during a patient’s first surgery whether the sentinel nodes show sign of metastasis,” says George Hollenberg, MD, a dermatopathology specialist in Plainview, NY, and former medical director of Acupath Laboratories.
“If so, the remaining nodes can be removed during that same surgical procedure, eliminating the second invasive surgery entirely.”
If surgery is planned to remove a spot that you think might be skin cancer, ask your surgeon if he or she knows about the MCW Melanoma Cocktail for on-the-spot sentinel lymph node biopsy results during the first surgery.
Dr. Hollenberg passed away in 2013.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How Accurate Are Melanoma Biopsies?

Biopsies for diagnosing melanoma aren’t as accurate as you may believe.
Biopsies for melanoma are not much more reliable than an 85 percent accuracy rate, according to chemistry professor Warren S. Warren, director of Duke University’s Center for Molecular and Biomolecular Imaging.
Warren headed the development of a laser-based tool that has the potential for diagnosing melanoma right in the dermatologist’s office.
This laser tool pumps tiny amounts of energy into a mole that a doctor may suspect is cancerous. The energy redistributes in skin cells, and this gets analyzed.
The Duke researchers discovered that a skin pigment called eumelanin is more prevalent in melanomas than in normal skin tissue.
Based on this, the researchers correctly identified the 11 malignant samples that were among 42 samples in the study.
The next step is to test the laser on thousands of archived slices of skin tissue.
Melanoma biopsies aren’t only less than reliable for diagnosing this disease, but are also capable of generating a false positive.
Warren says that even if the laser tool is only 50 percent more accurate than biopsy, it would actually prevent approximately 100,000 false-positive melanoma diagnoses; that is, normal tissue being diagnosed as melanoma.
A study in the Journal of American Academy of Dermatology (2010) says that pathologists would be in disagreement over whether or not a biopsy sample showed cancer … in 14 percent of biopsies.
A more accurate method of melanoma diagnosis is needed, says Warren, as false-positives result in expensive unnecessary treatments.
This laser tool is currently available commercially.
It just needs to be added to the microscopes that pathologists are already using to diagnose melanoma.
If you’re going to have a mole biopsied because your doctor ways it looks suspicious or because you’ve noticed it changing, you’ll want to inquire about the biopsy process — if the laser tool is in use.
Problem is, the cost to add the laser would be $100,000, but would more than offset the cost of unnecessary treatments for over-diagnosed cases of melanoma.
A more advanced step would be to develop the laser so that it can diagnose melanoma without the skin lesion even being removed from the patient.
This would be even more expensive than the tool being added onto a microscope, and this technology won’t be available for a few years, says Warren.
However, to get to that point, researchers plan on obtaining images of skin cancers grafted onto mice.
Conclusion: Standard biopsies of melanoma are nowhere near as reliable as people believe.
Currently, the technology exists to add the laser tool to microscopes for pathologists to more accurately diagnose melanoma. The full report is in Science Translational Medicine (Feb. 23, 2011).
In the meantime, make a habit of examining your skin every month, including behind the ears, between toes and on the bottoms of your feet, for suspicious lesions or moles.
And regardless of the reason you may ever have a mole removed, it should always be biopsied — even if it look perfectly normal and you want it removed for cosmetic reasons.
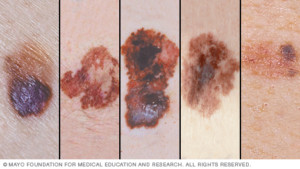
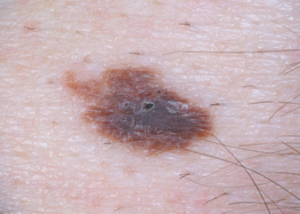
Examples of melanoma
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Peter Sobolev
Source: sciencedaily.com/releases/2011/02/110223151934.htm
Early Melanoma Detection: Mole Mapping Technology Helps Bring Peace of Mind

The earlier that melanoma is caught, the more likely you can be cured from this vicious cancer.
Most people are not aware of a groundbreaking technology that detects melanoma far earlier than any clinical exam can.
The technology is called digital dermoscopy, but this is a broad term, as this can refer to merely a hand-held device called a dermoscope that gives the physician a magnified view of moles.
A more in-depth version of “digital dermoscopy” involves a computer software program and serial photography of the patient’s moles.
Photos of moles, taken over a period of time, are taken, and then analyzed by the computer program to see if 1) they have endured changes over time, and 2) they have characteristics that, according to the computer’s database, resemble melanoma.
Digital dermoscopy with serial photography (around for about 10 years) is often referred to as “mole mapping,” though “mole mapping” is a broad term as well, and can simply refer to the patient’s crude drawing of his moles on a sketch pad.
I asked Dr. Theresa Pacheco, a dermatologist at the University of Colorado Hospital, about digital dermoscopy, aka mole mapping. UCH offers full-service digital dermoscopy including the computer software.
This technology is a godsend for people with many moles, and moles located in difficult-to-inspect areas like the back.
Elective removal of moles at increased risk for developing melanoma may make sense if the patient has only a handful of such moles.
But some people have literally hundreds of moles that require vigilant monitoring due to previous melanoma diagnosis, and/or nature of the moles (e.g., dysplastic).

Many atypical moles. Shutterstock/Mikel Ugarte Gil
How effective is digital dermoscopy at viewing obscure areas like the scalp and genitals?
Dr. Pacheco: You can shave the hair or part the hair and still use digital dermoscopy to examine the lesion.
Basically, how does the computer software “detect” that a mole looks suspicious?
Dr. Pacheco: The computer program utilizes certain variables like ‘color,’ ‘symmetry,’ etc., that it utilizes to compute a score… our mole mapper rates each lesion as red (abnormal), yellow (quasi normal) or white (normal)…. but it is really up to the physician to determine whether a biopsy is warranted.
Does the device look at only moles (the moles that the dermatologist has determined for mapping)?
Dr. Pacheco: Yes.
Does the instrument also have the capability of detecting early melanomas in non-mole areas of skin?
Dr. Pacheco: No.
Basically how does digital dermoscopy work?
Dr. Pacheco: The mole mapper should be considered as a tool for use by a trained dermatologist — the dermatologist determines which moles to map….and ultimately which moles to biopsy to look under the microscope.
It is not possible (time) to map every square inch of the body.
We do take overview of body areas (trunk, arm, hand, etc.).
We know melanoma arises in existing nevi (but most nevi are normal) and equally in normal skin … so we focus on new moles, changing moles, symptoms associated with moles, etc. (“nevi” means moles).
Suppose a patient decides to have digital dermoscopy every month. Is there any medical impracticality to this?
I’d think that monthly digital dermoscopy would be superior to the patient’s own layman’s naked eye inspections, especially since the patient can’t possibly get an accurate view of his back; and that digital dermoscopy would take substantial guesswork out of self-exams.
Dr. Pacheco: Sure… but I usually recommend a baseline and then in six months. If moles are stable, I have them come back in a year.
Mole mapping has been hailed as highly effective for people with many moles/dysplastic nevi and a history of melanoma. However, what is your take on someone without “high risk” skin having digital dermoscopy done, say, once every six months, just for 1) peace of mind, and 2) superior detection over the layman’s naked eye, especially when it comes to viewing the back?
Dr. Pacheco: No system or doctor is perfect – so I am fine with patients requesting mole mapping. It does lessen the anxiety.
Although – usually after a couple normal/stable mole mapping sessions – they are fine with coming less often and letting me dictate control of their skin examination.
Can digital dermoscopy detect changes in a pre-existing mole before those changes can be detected with the most scrutinizing naked eye?
Dr. Pacheco: Yes.
In that case, what percentage of such early detection (when mole is biopsied and declared melanoma) are stage 0 or in situ? (very early melanoma)
Dr. Pacheco: I am not aware of statistical reports.
Are you aware of any technology on the horizon that will be able to scan the entire skin surface and thus detect malignant changes in their most rudimentary stages in non-mole areas?
No.
So if you are interested in the earliest detection of melanoma and are concerned about your risk factors, inquire about digital dermoscopy with serial photography to your dermatologist.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: molecheck.co.nz/mole-map.html
Digital Dermoscopy for Melanoma Detection: First Person Account

I underwent serial digital dermoscopy at University of Colorado Hospital, and here’s what it’s like.
I finally decided to have serial digital dermoscopy done for melanoma screening, something I’ve been putting off for several years.
If you clicked on this article, you probably already know what serial digital dermoscopy is all about, as far as melanoma detection.
My insurance did not cover this, so be prepared in that your insurance may not cover it.
Serial digital dermoscopy is done at only a handful of facilities in the U.S., including at University of Colorado Hospital.
My dermatologist did not authorize the digital dermoscopy because I am not considered high risk for melanoma; thus, I paid out of pocket.
However, I also paid for some peace of mind, as this cutting-edge melanoma-screening technology has been proven to detect melanoma in its earliest stages.
I received a full-body skin exam from a third-year dermatology resident (University of Colorado Hospital is a teaching hospital), followed by a full-body skin exam by a dermatologist.
The doctor then decided to have three moles on my back imaged; no others.
Apparently, their digital dermoscopy is mostly for just the back, since this is the hardest-to-view area of the body.
The three moles on my back did not stand out from any of the moles elsewhere on my body (i.e., legs and arms).
However, I can’t view the back ones well, due to their location. Two of these moles are very small.
Apparently, the reason that larger moles on my leg were not included in the imaging was because I can readily inspect them.
After the doctor marked, with ink near them, the moles on my back, I was led to the room next door for the digital dermoscopy.
I stood, back facing a nurse, who was at a computer console. She placed an imaging device to the moles (I couldn’t see the device, of course, but it obviously recorded the image into the computer).
My Moles Were on the Computer Screen
She then showed me the 20-times magnification of each mole on the screen.
What a mole looks like, magnified 20 times, is entirely different than what it looks like to the naked eye.
In fact, the appearance looks a little scary because it is much less exact, less defined, more diffuse, and (in the case of a normal mole) full of spidery-looking configurations that dermatologists refer to as the “network” of a mole’s pigment.
The nurse pointed out that the squiggly lines or network were actually very normal, and that if the image showed instead a more dense, solid mass of brown, it would be concerning.
In the computer system was also a full image of my back.
The images of the three moles, plus the full image of my upper and lower back, will comprise the baseline images, so that 12 months from now, new images of the same areas can be compared: serial digital dermoscopy.
It will be easy to detect early changes in moles with a 20-fold magnification – changes that even a doctor’s highly trained naked eye will not be able to detect, and changes that even a doctor’s handheld dermoscope will not detect.
The procedure was brief and after the third mole was imaged, the nurse sprayed cleanser on my back to wipe off the ink. And that was that.
Paying out of pocket is worth the peace of mind that serial digital dermoscopy will bring to “mole-conscious” folks concerned about melanoma.
However, serial digital dermoscopy does not replace monthly home skin exams or the yearly clinical exam.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Why Small Dogs Should Be Walked Even if They’re Normal Weight

My brother has had two small dogs (not fat, not even overweight) for a number of years and informed my mother that if she got a small dog, she wouldn’t have to walk it.
His exact words were: Small dogs don’t have to be walked.
Are you with him on this? And if so, is there a size cut-off? What if a small canine is part Chihuahua, part Golden Retriever? Hmmm.
It can get very confusing, trying to determine how small a dog needs to be to be exempt from being walked, and whether or not it’s a little overweight or moderately overweight, and taking into consideration its breed or mix of breeds — in order to require regimented walking for exercise. What a conundrum!
Whether or not your pet is overweight isn’t the issue; there are many other benefits to walking a small dog, says Dr. Liz Hanson, a doctor of veterinary medicine at Newport Animal Hospital in Newport Coast, CA.
Dr. Hanson points out that smaller breeds like the Maltese, Chihuahua and Pomeranian may be able to burn enough calories with normal activity inside the house to maintain a lean body.
But this doesn’t mean these small furry friends don’t need to be walked or given some form of outside exercise.
“Exercising your dog will help keep your small dog agile, limber and maintains good muscle tone which helps reduce arthritic pain as they get older,” explains Dr. Hanson.
“In addition, regular walks help keep your pet’s digestive system healthy and are beneficial to those with constipation issues.”
Does your small dog, that never gets walked because it’s trim, have unresolved constipation issues? Maybe it’s time to start taking Muffin for daily walks.
Or does little Princess bark too much? “Many small breed dogs have behavioral issues such as excessive barking, chewing, scratching and digging,” says Dr. Hanson.
“Walking your dog daily will help reduce and even eliminate many of these behavioral problems that often stem from boredom.”
Another reason to walk a small dog regardless of its weight is to help socialize it, says Dr. Hanson. “Smaller dogs kept mainly at home are often fearful of other dogs and people due to lack of exposure.”
Dr. Hanson notes that small breeds can be hyperactive; if your little pet has too much energy, chews furniture or jumps excessively, a regular walking program is just what the doctor ordered. This will help calm your pet down in the evening.
Do not let the absence of obesity or the presence of trimness guide you in whether or not to walk your small dog.
As you can see, taking a Pomeranian, Maltese or other tiny breed on regular walks can provide multiple benefits very unrelated to obesity or excess weight.