What If a Patient Pulls Burr Hole Brain Drain Tube Out?

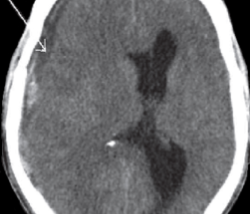
After a burr hole craniostomy for chronic subdural hematoma, a “drain” tube is left in the patient’s skull. This was the case of my mother.
She had a chronic subdural hematoma, and the drain tube that was placed in her head, after her second surgery, accidentally came out after she was shifting in her bed while propped up, and – according to her report – sat on the short tube, causing it to get tugged.
She immediately reported this to the staff via her nurse call button. If you clicked on this article, I needn’t explain to you what the burr hole drain looks like as it feeds into the patient’s head.
In the case of my mother, all that was there were small bandages, but the tube, as it entered the shaved portion of her head, was visible.
Will blood and cerebrospinal fluid spurt all over the place if the tube is pulled out (or comes out by accident, at least)? Not in the case of my mother.
I wouldn’t think any spurting would occur unless the burr hole tube came out the same day of the surgery.
In the case of my mother, it was tugged out on Friday; she had had the surgery two days prior on Wednesday. So by then, there wasn’t heavy draining.
I saw spots of a mixture of blood and cerebrospinal fluid here and there on the bed sheets, but nothing messy or alarming.
The burr hole is already draining in these cases, so if the tube comes out prematurely, of course the draining is going to continue.
But instead of the fluid draining into the tube, it will be “leaking” onto the scalp and will need someplace to go.
In this case, the fluid went onto the gauze that the nurse was sturdily applying to my mother’s scalp … after she paged the neurosurgeon for instructions.
Do not try to place the tube back in the burr hole! When the tube comes out, it immediately becomes contaminated! Instead, call the nurse if the patient already didn’t. Do not touch the hole.
When the nurse was applying compression, it was painful. Don’t panic if the nurse says that “brain juice” is coming out.
“Juice” means cerebrospinal fluid, possibly mixed with blood – which you already know is the objective of the draining in the first place when someone has chronic subdural hematoma.
You actually want this “juice” to continue to come out, because its collection in the brain is why the patient ended up having surgery in the first place.
As I watched the nurse maintain her compression on the burr hole, I asked how they were going to control the leaking.
She mentioned something about applying Vaseline which would create a barrier. Do we really want that, I asked, because the whole idea is to get the fluid out of the brain, not trap it in there with a barrier.
The nurse acknowledged my point, and then the neurosurgeon got back to her.
The final verdict was to wrap my mother’s head several times with a special wrapping, then have her lie on her side (the burr hole side against the pillow) as much as possible, so that gravity would allow continued draining.
A collection sheet was placed between her head and the pillow in case any fluid seeped through.
Why weren’t plans made to put in a new drain? This would require a sterile environment, i.e., another surgery in the OR, and also, the surgeon wasn’t available.
When my mother’s burr hole drain came out, it wasn’t an emergency situation. Again, the fluid is supposed to drain out anyways.
Next morning the bandages were removed and I was told that there had been minimal leaking, and the bandages remained off. Sutures were put in place.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Natalie Board
Antidepressant Losing Steam and Pooping Out? Solution

An antidepressant may work wonders initially but then may lose its punch and can’t keep up with the depression.
You may be on an antidepressant that’s been working wonderfully…
But then soon after you go on the prescription drug, it begins losing its full effect. It has pooped out: the “poop-out effect.”
The antidepressant that my mother was on for clinical depression seemed to start pooping out less than two weeks after starting it.
The drug was Cymbalta and the prescription called for 30 mg the first week, then 60 mg the second week.
Oddly, the doctor prescribed only 30 capsules with no refill authorization.
I consulted with my brother, who had been working in the pharmaceutical industry as a chemist for many years.
When an antidepressant poops out, this means it has lost its fire or power when it comes to subduing depression symptoms.
This doesn’t mean it’s lost all of its effect, but enough to cause concern in the patient and/or family members. The regression in my mother was noticeable.
With my mother, the poop-out effect took place on day 13 and day 14 of being on Cymbalta.
I assumed that she’d have to go up to 90 mg so that the drug could resume its full effectiveness.
I also wondered if her doctor would switch to a different drug, or, keep her on Cymbalta but add a second drug.
In the case of my mother, it turned out that the antidepressant hadn’t pooped out at all.
On day 15 she did great, and the next day we were in the doctor’s office.
The doctor explained that it takes a while for antidepressant drugs to take full effect.
Some days will be better than others, but as long as the overall picture looks good, then the drug is working.
On day 12, in the evening, my mother received some alarming news about a family member — a divorce, and I surmise that the shock had not sunk in that evening — until she went to bed.
Next morning she reported she hardly slept, having been kept awake thinking about the family member.
The second half of next day, my mother had what appeared to be the beginnings of a relapse into the depression. This repeated next day, and was worse.
But the day after, she was hopping. And I figured that the relapse had to have been related to news of the divorce.
Though my mother had setbacks, the drug was still working because without the antidepressant, she would have been debilitated, weeping and hardly eating.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Atrial Fibrillation, Elevated Troponin: How Much Heart Damage?
Can enough atrial fibrillation episodes, over time in someone with heart disease, cause cardiac damage that’s equal to a heart attack?
“Generally, A-fib does not result in significant heart damage,” says Dr. Simon Dixon, chairman of cardiovascular medicine for Beaumont Health System in Michigan.
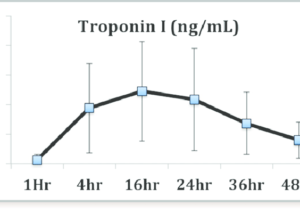
You may already know that the higher the troponin level, the more damage that’s been done to the heart. The higher the troponin elevation, the worse the long-term prognosis is.
Over a certain level means a heart attack. Under that cut-off point, the result is deemed “indeterminate” or a “grey area.”
I wondered if a lot of “indeterminate” elevations of troponin, from atrial fibrillation in a patient with heart disease, would, over time, “equal” a heart attack.
So for example, suppose the elevations range from 0.11 to 0.30 – many of these over an extended period of time from episodes of A-fib that occur between sporadically and frequently.
Wouldn’t eventually all of these fractions “add up” to a heart attack?
Dr. Dixon explains, “Some patients have chronic low levels of troponin elevation (for example, 0.14 ng/mL).
“This can be ‘normal’ in some patients, or associated with disorders such as heart failure and kidney failure.
“This level of troponin elevation does not necessarily cause the same level of damage as a heart attack.”

Dr. Dixon specializes in the treatment of acute and chronic coronary artery disease, with research focusing on pioneering treatments to save heart muscle in patients having heart attacks.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/megaflopp
Why Can A-Fib with Heart Disease Cause Troponin Elevation?

There’s a specific reason why an episode of atrial fibrillation can elevate troponin levels if you already have heart disease.
Troponin is a protein enzyme that leaks from heart muscle when that muscle sustains damage, such as from a heart attack or blunt chest trauma.
But an episode of atrial fibrillation — an abnormal heart rhythm – -can also cause a leak of troponin, which of course, means that some damage to the cardiac tissue has occurred—but not nearly as much as would occur from a heart attack.
In a person whose only condition is A-fib, an episode of this cardiac arrhythmia won’t cause a rise in troponin.
But if someone has severe coronary artery disease, it can. In severe coronary artery disease (or “heart disease”), the arteries that supply blood to the heart are at least 70 percent blocked with plaque.
This leaves a small diameter through which blood gets through, and can cause symptoms, usually shortness of breath with only mild exertion, and/or chest pain.
Atrial Fibrillation + Heart Disease = Rise in Troponin
“Patients with coronary artery disease are more likely to have a troponin elevation because the blockage in the artery limits the ability of the heart to increase blood flow to the muscle during the AF episode,” says Dr. Simon Dixon, chairman of cardiovascular medicine for Beaumont Health System in Michigan.
When a patient’s troponin test result is elevated, another one should be taken several hours later to see if the numerical result is higher.
The test may be repeated a few more times to see when the number stops rising and starts coming down.
If the patient has not exhibited any sign of a heart attack, such as chest pain or pressure, clammy skin, nausea, jaw or arm pain, or shortness of breath, but they have atrial fibrillation, then the reason for the elevated troponin will not likely be that of a heart attack.

Dr. Dixon specializes in the treatment of acute and chronic coronary artery disease, with research focusing on pioneering treatments to save heart muscle in patients having heart attacks.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/designer491
Does Every Episode of Atrial Fibrillation Damage the Heart?
In someone with coronary artery disease, does every episode of atrial fibrillation mean damage to the heart?
Damage to cardiac tissue can result from an episode of atrial fibrillation in a person with coronary artery disease.
Not all people with CAD experience A-fib, and not all people who have periods of atrial fibrillation have coronary heart disease.
Arial fibrillation is a rhythm disorder that increases the risk of blood clots that can lead to a heart attack or stroke.
In fact, A-fib is a major risk factor for a massive stroke, which could be fatal.
This arrhythmia is characterized by a sudden increase in heart rate — but it’s not a steady rate. It jumps all over the place.
This erratic beat can be felt in the pulse with fingers to the wrist.
The numbers on a heart rate screen will be jumping all over the place.
Atrial fibrillation and coronary artery disease can exist in the same patient, and there are times when an event of atrial fibrillation results in a mild elevation of troponin, the protein enzyme that leaks from the heart muscle—indicating that damage was sustained.
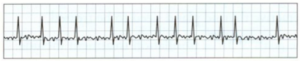
An EKG showing A-fib
Does every incidence of A-fib in someone with coronary artery disease necessarily damage the heart?
“Most episodes of AF do not cause the troponin to be elevated,” says Dr. Simon Dixon, chairman of cardiovascular medicine for Beaumont Health System in Michigan.
“This depends a lot on the heart rate during episodes as well as other factors such as blood count and the extent of coronary disease.”
Thus, if someone with heart disease has several A-fib episodes per week, this does not necessarily mean that the patient’s heart gets damaged (as revealed by elevated troponin) every time.
“Atrial fibrillation can occur in episodes (paroxysms) or be present all the time (permanent),” says Dr. Dixon.
“Most patients with AF do not sustain muscle damage unless the heart rate becomes quite uncontrolled, or there are other medical factors such as fever, low blood oxygen level or low blood count.”

Dr. Dixon specializes in the treatment of acute and chronic coronary artery disease, with research focusing on pioneering treatments to save heart muscle in patients having heart attacks.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/TippaPatt
What’s the Elevated Troponin Range from A-Fib Episodes?

An episode of atrial fibrillation can elevate troponin, but what would be the typical range of this elevation?
Atrial fibrillation (A-fib) is a serious heart rhythm disorder that can have significant consequences if left untreated.
While some patients may not experience symptoms, A-fib poses a major risk due to the potential for blood pooling in the heart.
This stagnation increases the risk of ischemic stroke, particularly in individuals over 65 and those with additional stroke risk factors, such as a family history or smoking.
Additionally, A-fib can lead to elevated levels of troponin, an enzyme released by the heart when the cardiac muscle is damaged.
Elevated troponin levels indicate that the heart is under stress or experiencing damage, further complicating the management of A-fib and its associated risks.
Atrial fibrillation. BruceBlaus
“Some patients with atrial fibrillation develop a fast heart rate (rapid ventricular rate) in the setting of infection, bleeding or other medical conditions,” says Dr. Simon Dixon, chairman of cardiovascular medicine for Beaumont Health System in Michigan.
One such medical condition is coronary artery disease: buildup of fatty deposits inside the arteries.
These arteries supply blood to the heart muscle, and when plaques accumulate, they narrow and harden the arteries, reducing blood flow.
When an episode of A-fib occurs, says Dr. Dixon, “the heart muscle needs greater blood supply to provide oxygen and glucose [blood sugar].
“At times, however, the ‘demand’ outstrips the ‘supply,’ resulting in damage to the muscle (especially on the inside wall of the heart, or subendocardial layer).
“Generally the troponin elevation in these cases is small, for example, 0.1-2.0 ng/mL (the upper limit for the normal range of troponin in our hospital is 0.06 ng/mL).”
This troponin range is called “indeterminate,” because it can have numerous causes other than an episode of atrial fibrillation, but this range isn’t high enough to arouse the suspicion for a heart attack.
Troponin elevation of unknown origin is far more common in elderly people, but should always be followed up.
Age of Patient with Elevated Troponin
The younger a person is, the more significant an elevated result is.
In the younger adult population, elevated troponin levels are less likely to be attributed to age-related conditions and more likely to indicate acute or significant cardiac issues, such as a heart attack or severe heart inflammation.
In contrast, older adults may have elevated troponin levels due to chronic conditions or age-related changes in heart function that are less immediately alarming.
Therefore, in younger adults, an elevated troponin level typically means a more urgent investigation to find out what the cause is.

Dr. Dixon specializes in the treatment of acute and chronic coronary artery disease, with his research focusing on pioneering treatments to save heart muscle in patients who are having heart attacks.
 Lorra Garrick has been covering medical, fitness and cyber security topics for many years, having written thousands of articles for print magazines and websites, and this includes as a ghostwriter. She is also a former ACE certified personal trainer.
Lorra Garrick has been covering medical, fitness and cyber security topics for many years, having written thousands of articles for print magazines and websites, and this includes as a ghostwriter. She is also a former ACE certified personal trainer.
.
Top image: Shutterstock/ designer491
How to Get Relief from Fibromyalgia with Cymbalta

How does Cymbalta help relieve fibromyalgia pain?
You can get fibromyalgia relief with Cymbalta, a drug commonly prescribed for depression and also prescribed for panic attacks and anxiety.
You’ve probably seen the Cymbalta commercials, which begin with, “Where does depression hurt? Everywhere.”
Another of Cymbalta’s on-label uses is for the nerve pain of diabetes neuropathy.
There are a few ways in which Cymbalta relieves the pain of fibromyalgia, which is a pain disorder of the entire body.
Now, from an anecdotal standpoint, Cymbalta can bring on fibromyalgia relief by perhaps suppressing the patient’s perception of physical discomfort (which clinical depression will amplify).
This happened with my mother, but she didn’t have fibromyalgia; she had severe depression.
Coinciding with the depression were a few orthopedic issues, and while in a depressed state of mind, my mother complained that the orthopedic pain was excruciating.
Orthopedic discomfort indeed can be excruciating, but …. carpal tunnel syndrome?
Post-surgical discomfort from knee arthroscopy? (After my mother began taking Cymbalta, suddenly, the pain was no longer excruciating; it was merely inconvenient!)
Asking the Expert
How was it that an antidepressant like Cymbalta would end up with an on-label use for fibromyalgia relief?
“Pain management specialists prescribe Cymbalta for two reasons,” says Joe Wegmann, psychopharmacologist and licensed clinical social worker, author of Psychopharmacology: Straight Talk on Mental Health Medications.
“First, they are aware that that anyone with a chronic illness, especially a debilitating one like fibromyalgia, is at risk for depression.
“So physicians take this into account when treating fibromyalgia even if depression/anxiety is not present when treatment begins.
“Prolonged pain in anyone can cause changes in brain chemistry that can lead to depression.
“So physicians prescribe Cymbalta to cover for the depression that so often, at some point, develops in those with fibromyalgia.
“So brain chemistry does change as a result of this often debilitating physical illness.
“It’s impossible to separate the physical from the emotional; this is why depression rates are high in these patients.”
But even if a person with this disorder does not have depression, this SNRI antidepressant has been known to provide relief from the symptoms of discomfort associated with this condition.
Wegmann continues: “Another reason Cymbalta is prescribed for fibromyalgia is due to its powerful serotonin effects. Serotonin is a powerful vasoconstrictor, and since pain is linked to vascular vasodilation, Cymbalta’s constrictive effects help moderate pain.”
If your fibromyalgia is not responding to holistic treatments, and the pain is impossible to live with, your doctor may end up prescribing Cymbalta for pain relief.
 Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How to Get a Very Depressed Person Who Refuses to Eat to Eat

It’s really scary when severe depression prevents a person from wanting to eat; right before your eyes you see your loved-one wasting away from malnourishment.
Clinical depression can destroy appetite and cause a life-threatening issue of malnourishment, especially if the clinically depressed individual is elderly.
Not too long ago my mother developed a bout of clinical depression that is now under control with Cymbalta.
When my mother’s depression first began developing (it was a gradual process, not an overnight event), she commented that she “had no appetite.”
I didn’t take this seriously until I began noticing about two weeks later a visible loss of muscle.
My mother is of senior age, and it is dangerous for seniors, especially women, to lose muscle tissue.
It reached a point where I, and my father, had to prompt her to eat nearly every bite of food, and most of these prompts netted a refusal.
So how did I get my depressed mother to eat?
#1: Buy Walgreen’s “Balanced Nutritional Drink Plus.” Amazingly, I managed to get my mother to drink 1-2 cans a day. One can is 350 calories. Substitutes would be Ensure Plus or Boost Plus.

If you can get your depressed family member to consume two of these 8 ounce cans, that’s a good foundation of 700 calories for the day.
#2: When giving your depressed family member a beverage, include a straw. A straw guarantees more of the liquid will get consumed.
#3: Do not ask your depressed family member if they want something to eat or drink.
My father would ask this to my mother, and every single time, she’d say “No.” He’d then give up. BIG MISTAKE.
I decided to take the bull by the horns and instead of asking if my mother wanted to eat, I’d just bring the food to her mouth.
I strongly suggest that you don’t even TELL your depressed family member you’re going to give him or her some food or drink, because this will give them an opportunity to refuse.
Don’t inform them at all of your plan. JUST DO IT: Bring them the food.
When the food is in front of them, they are likely to take a bite or sip.
My mother has always enjoyed eggs. My father would ask her if she wanted eggs. She’d say no. He’d give up.
I insisted, “Don’t ask. Just make her the eggs. She’ll eat some once they’re cooked and in front of her.”
My father at first didn’t go along with this, but he eventually learned that it was true:
Once the eggs were actually prepared and placed before my mother, she’d eat some.
#4: Don’t be passive. Be kindly aggressive. Again, my father (along with my brother) one evening were enjoying salmon while my mother refused any food at all and sat withered in another room.
I gathered some salmon scraps and not only took a plate to her, but literally fork-fed her.
She consumed six forkfuls (about 15 grams of protein) that she would have never eaten had I not taken an assertive stand.
DO NOT BE AFRAID TO GET ASSERTIVE with your depressed family member who refuses to eat. It really works.
There were many instances in which I just verbally nagged my mother until she agreed to eat something, if for no other reason to get me off her back. Every bite counts. Every sip counts.
#5: When presenting your depressed family member with unexpected food (review #3), don’t just set it before them and walk away. Spoon feed them if that’s what it takes.
I spoon fed my mother pudding, chicken, and placed pretzels between her lips. I also placed cups to her mouth.
- Do not hesitate to make statements like, “If you don’t eat this, you may have to be tube-fed at a hospital.”
- I also told my mother, “I’m going to hover right over you until you drink this juice.”
These tactics worked, though often, my mother refused to finish the item. But hey, half a cup of juice is better than nothing.
Don’t assume that a depressed person who refuses to eat, absolutely will never eat while in bed.
I’d bring my mother quite a few nutrition cans with a bent straw, and while propped up, she drank the beverage.
She also ate eggs in bed while propped up; she didn’t ask for the eggs; I brought them to her and told her she was going to eat them.
#6: Don’t get concerned about nutrition; the issue is to just get calories into the depressed family member’s mouth, even if it’s junk food.
I was actually encouraging my mother to eat bacon and sausage — these have calories and protein.
BIG MISTAKE: Pointing out to a depressed family member who’s lost their appetite that something they’re suddenly interested in eating is not healthy.
#7: Do not make any comments within earshot of the depressed family member that might discourage eating.
Example: My father poured a can of soup into a pot. I removed another can from the cupboard: one for my mother, one for him.
He told me no, he was going to eat half the soup in the pot, while my mother would get the other half.
He said, “There is too much soup here for your mother to eat; I have to take half of it.”
This possibly gave my mother, in her depressed, vulnerable state of mind, the idea that she could eat only half the can.
She ended up eating half of what was in the pot because my father divided it into two bowls.
Had my father poured two cans in the pot, and then divided THAT into two bowls, my mother would have ultimately eaten more, even if she didn’t finish the bowl: 100 percent of half a can is LESS than 75 percent of one whole can.
#8: Sneak calories into the food. If I poured half a can of the Walgreens product into a paper cup, I’d then give her the remaining portion straight from the can and tell her it was “half full,” when in actuality, I had added a little milk to it.
#9: When your depressed family member, after eating at your insistence, says for the first time, “I’ve had enough,” or, “No more,” etc., this means they can actually take two or three more bites.
This was very predictable — but you’re the only one who has to know. Spoon/fork-feed those two or three more bites.
Thus, do not stop feeding your depressed family member after their first “Enough.”
The above tactics enabled me to get my mother to consume about 1,300 calories a day.
In order to get a depressed person, who refuses to eat, to consume this many calories, it’s essential to include, daily, two cans of the “Plus” Walgreens, Ensure or Boost products.
Secretly add a tablespoon of olive oil or chocolate syrup for even more calories.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Cymbalta for Pain and Depression: Helpful Information

Cymbalta is prescribed for depression and pain, and here is helpful information for people considering Cymbalta or who have already started taking this drug.
Cymbalta belongs to a class of medications called SNRI: serotonin and norepinephrine reuptake inhibitors.
When Cymbalta is prescribed strictly for pain (the patient does not have depression), what is the usual starting dose?
“Thirty mg a day for 3-6 weeks; if side effects are not a problem and pain persists, increase to 60 mg a day,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “From Fatigued to Fantastic!”
“Higher doses add significantly higher side effects but minimal improvement in pain relief over the 60 mg a day dose. Unlike most medications, Cymbalta tablets cannot be broken in half.”
I understand that getting off Cymbalta can be very troublesome.
Is this because many people quit cold turkey, or can it be difficult to get off it (withdrawal symptoms, discontinuation syndrome) even if it’s tapered (gradually decreasing dose)?
Dr. Teitelbaum: “Like all serotonin antidepressants (Prozac family), this is the case, and it can take months to taper off the medication.”
Is it true that a person’s body would necessarily build up a tolerance to Cymbalta, such that over time, the prescribed dose loses effectiveness, and then the patient must take a higher prescription? How common is this?
Dr. Teitelbaum: “Not very common.”
How would Cymbalta, at least a starting dose anyways, affect someone who does not have nerve pain, depression or anxiety? Would an SNRI produce exaggerated side effects?
Dr. Teitelbaum: “Likely make them hyper.”
It’s really fascinating how SNRI and SSRI (selective serotonin reuptake inhibitor) drugs work for depression, so here’s a basic chemistry lesson.
First of all, feeling depression is part of being human and having a higher-functioning brain. Depression can be caused by life events; side effects from medications; and for unknown reasons.
Depression can be mild, moderate or severe. For some depressions, there is an association between the level of serotonin in the brain and the presence of this mood disorder. The association is a reduced amount of serotonin.
However, researchers do not know whether this is cause or effect; i.e., does depression result in diminished serotonin, or does diminished serotonin cause depression?
And if the latter is the case, can stressful life events trigger this disruption of serotonin levels?
In the brain are neurons (nerve cells) that have receptor sites for neurotransmitters like serotonin.
After the receptor sites receive serotonin, a chemical process “destroys” the serotonin at that point.
This process is called reuptake. If too much reuptake occurs, low levels of serotonin result — which is associated with depression.
Drugs like Cymbalta inhibit, or put some brakes, on this reuptake process. The result is a higher level of serotonin, and in many cases, a complete vanishing of depression symptoms.
Cymbalta and other SNRIs, and SSRIs, don’t come without side effects. So before taking Cymbalta, do a risk-benefit assessment, and also keep in mind that if Cymbalta doesn’t work for your body chemistry, there are other similar drugs on the market.
And no matter what you decide, remember, a program of rigorous exercise and sound nutrition will go a long way to fight depression.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Phovoir
Kefir Is Great for Microscopic Colitis Relief!

Mmmm, a glass of chilled kefir just may relieve your microscopic colitis symptoms!
Give this probiotic a try; it will help re-balance the bacteria in your gut.
An imbalance may be causing or contributing to your microscopic colitis.
“Kefir or probiotic supplements can help to control the diarrhea in microscopic colitis,” says Lawrence Hoberman, MD, a board certified gastroenterologist and creator of EndoMune probiotic products.
“It is thought that there is a change in the healthy intestinal bacteria or microbiome which allows overgrowth of harmful bacteria, viruses or parasites.
“Taking kefir or probiotics that contain the healthy intestinal bacteria will rebalance the intestinal bacteria.
“This will modify the intestinal immune system and stop inflammation.”
Kefir Comes in Different Flavors

When I had a flare of microscopic colitis, kefir seemed to have a beneficial effect.
I won’t go the route of prescription or over-the-counter drugs because these only address the symptoms, if they even work at all.
In fact, Imodium may delay the inevitable by causing constipation.
Kefir works by actually treating microscopic colitis.
Essentially, kefir is yogurt in drinkable form, but it also contains live culture bacteria, or, the “good” bacteria, the beneficial bacteria that you need for optimum intestinal health.
Kefir is a probiotic; probiotics are good or “friendly” bacteria that are an integral part of a healthy balance of microorganisms in human intestines.
It’s believed by doctors that microscopic colitis can be caused by an overgrowth of bad bacteria; or, to put it another way, an imbalance in the ratio of good to bad bacteria in the intestinal tract.
There may be a genetic component to this, but that has not been proven.
Here are a few theories:
1) The body for some unknown reason “attacks” the good bacteria that grow in the colon, thereby offsetting the balance.
2) This can be triggered by NSAID’s and aspirin, antibiotics and eating certain foods that favor the growth of bad bacteria.
Because kefir is a probiotic, ingesting this drink helps restore a more optimal balance of good bacteria and bad in the gastrointestinal tract.
Years ago when my microscopic flare was in full force, I had gone off kefir several times, and every time, the symptoms returned.
My symptoms were a lot of diarrhea and large amounts of undigested food in my stools.
If you have microscopic colitis, go straight to the kefir, because it’s drinkable, which makes it more convenient than yogurt (which also comes in probiotic form).
You may also want to take probiotics in supplement form such as EndoMune if you don’t care for the taste of kefir or for times that you’ve run out of it.



























 With 40+ years’ experience, Dr. Hoberman is an expert in probiotics. He has extensive first-hand experience treating a variety of digestive health issues and has seen the dramatic results probiotics have had on his patients. endomune.com/meet-dr-hoberman
With 40+ years’ experience, Dr. Hoberman is an expert in probiotics. He has extensive first-hand experience treating a variety of digestive health issues and has seen the dramatic results probiotics have had on his patients. endomune.com/meet-dr-hoberman







































