Trouble Breathing, Chest Pain After Joint Replacement Surgery

Trouble breathing with chest pain after joint replacement surgery never has a benign cause, says Barbara Bergin, MD, an orthopedic surgeon.
NEVER assume that chest pain with difficulty breathing following joint replacement surgery is a sign of anxiety.
What can chest pain and feeling like you can’t get enough air actually mean?
“This would be a bad sign,” says Dr. Bergin, board certified orthopedic surgeon at and co-founder of Texas Orthopedics, Sports & Rehabilitation Associates.
“I can’t think of a benign process which would cause chest pain and trouble breathing after a total joint replacement, unless you coincidentally sustained an injury to your chest or ribs.
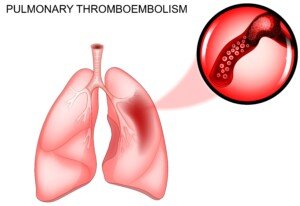
“Otherwise, you’re either experiencing a heart attack, or more likely…a pulmonary embolism, which is the result of a blood clot which has dislodged from the leg and entered the lungs.”
Father Had a Knee Revision Operation
I visited my father in his room three hours after his knee joint revision surgery.
On both feet were sequential compression devices that periodically inflate to squeeze against the patient’s feet to generate circulation in the legs to prevent blood clots.
He was also on the blood thinner Warfarin and was wearing knee high compression stockings.
Shortness of Breath and Chest Pain While Still in the Hospital
The hospital stay for a knee or hip replacement surgery is normally several days.
The patient himself, upon experiencing chest pain or diffiulty with breathing, may be able to press the nurse’s call button if alone.
The diagnosis of a pulmonary embolism, however, can only be made with a CT scan. There may be a few other tests as well.
Pulmonary Embolism
Only after this confirmation would the patient be givn a clot-busting drug via an I.V. — per doctor authorization.
Never would the patient receive such a drug without FIRST a diagnosis of a pulmonary embolus.
Naturally, I wondered what would happen if my father suddenly developed chest pain and shortness of breath, and on the way to the CT scanner, the pulmonary embolism got bigger and completely blocked his ability to breathe!
“A large blood clot to the lungs can kill you in short shrift,” says Dr. Bergin.
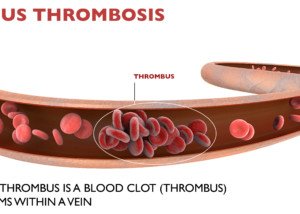
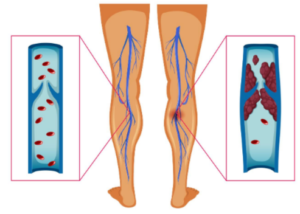
Why a Blood Clot Forms
“After surgery on the lower extremities, the blood coagulation process is in a heightened state,” says Dr. Bergin.
“This happens throughout the whole blood supply, in response to having a cut anywhere in the body.
“But in the leg, the circulation of venous blood gets sluggish because of the surgery and swelling.
“The movement of blood through the veins is assisted by movement of muscles.
“This helps pump venous blood out of the extremities, because veins have no ability to pump blood, like arteries do.
“What happens after surgery? We’re lying around in bed, not moving our leg, because it hurts [knee or hip replacement].
“So heightened coagulation + surgical swelling + less movement of the leg = increased potential to have a blood clot in the leg.
“This process usually takes a few days, but occasionally, it happens sooner. Some patients are more susceptible to developing blood clots, so it can happen within 24 hours.”
Trouble Breathing, Chest Pain Soon After Discharge
The patient continues to recover from joint replacement surgery at home. They then develop these two symptoms.
“This is an emergency, and under no circumstance should it be ignored,” says Dr. Bergin. “Call your surgeon, or better yet…call 9-1-1.”
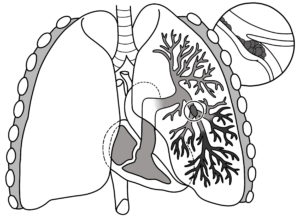
Deadly Saddle
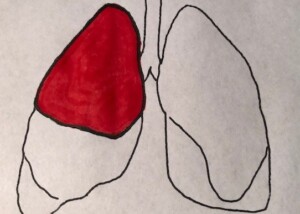
The type of pulmonary embolus that can kill in a minute is called “saddle,” because it blocks blood flow to both lungs at the same time — sealing off the entrance to any inhaled oxygen.
However, the saddle P.E. is not likely to strike a healthy person, even if they’re over 80.
It’s more likely with someone who has a pre-existing clotting disorder or very poor health.
The type of pulmonary embolus that usually develops in joint replacement patients are smaller clots that occupy only one lobe of the lungs (a pair of lungs has five lobes total).
A patient could have trouble breathing because a clot is in one lobe, but still be able to breathe with the four other lobes and have plenty of time for a CT scan and diagnosis.
Can shortness of breath + chest pain after a joint replacement have a less serious cause?
Dr. Bergin explains, “Occasionally chest pain and shortness of breath can be due to stomach acidity.
“But don’t assume that,” EVEN IF the patient has recently been diagnosed with a bad case of acid reflux.
“Chest pain and shortness of breath after surgery on the lower extremities means heart attack or pulmonary embolism until proven otherwise. You’re off to the ER in short order” if this occurs after the patient returns home.
As for my father, I was always on high alert, periodically asking him if he felt short of breath or had chest pain. He had no complications and fully recovered.

Dr. Bergin is a general orthopedist, surgically and conservatively treating all manner of bone and joint conditions. She enjoys educating patients so they can emerge stronger than they were before their orthopedic injury or surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ESB Professional
Sources:
mayoclinic.org/diseases-conditions/pulmonary-embolism/basics/symptoms/con-20022849
mayoclinic.com/health/pulmonary-embolism/DS00429/DSECTION=risk-factors
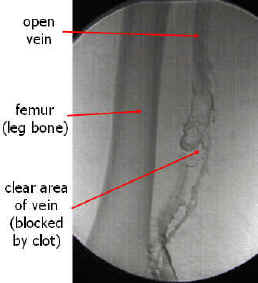
Knee Replacement DVT: Patients at Highest Risk?

Certain kinds of patients have the highest risk of a DVT following joint replacement surgery.
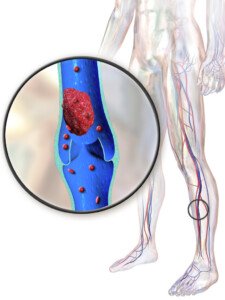
A DVT is a deep vein thrombosis which could break off and travel to the lungs and be life threatening.
When it comes to knee replacement surgery, few patients just do not have a choice, and along with this extremely common procedure is the risk of DVT: deep vein thrombosis.
DVT has gotten a lot of attention lately within the context of extended air travel, but the king of DVT production is surgery, especially joint replacement.
A deep vein thrombosis is a blood clot. Part or all of it may break away and migrate into the lungs: a pulmonary embolus.
Tiny pulmonary emboli are not life-threatening, but massive or “saddle” pulmonary emboli can drop you in seconds — permanently.
This is why DVT prevention is critical.
Anyone can develop a pulmonary embolus if the perfect storm is in place, such as extended air travel while keeping the legs in the same cramped position; lack of hydration; being on birth control pills; excessive bed rest from a foot injury; and so many other circumstances.
Joint replacement patients are given DVT prevention treatment, namely blood thinners.
But certain joint replacement patients still have a relatively high risk of deep vein thrombosis.
A report in the Journal of Bone and Joint Surgery (2011) states that blood clot formation, including the pulmonary embolism, is a serious complication from knee replacement surgery.
The paper also says: “Prophylactic measures, such as the use of blood thinners around the time of surgery, are used to reduce the occurrence of clots, but their effectiveness in routine clinical practice following surgery is more uncertain.”
How the Study Was Done
- The study tracked over 37,000 knee replacement patients between 1997 and 2007.
- For 90 days after surgery is when pulmonary embolism risk is highest.
- There were 441 patients (1.2 percent) who had to be hospitalized for blood clots during this time window. The following risk factors were associated with clot formation:
– Over age 80
– History of previous clot
– History of cardiovascular disease
– Increased comorbidities (additional medical conditions like diabetes)
The study noted that knee replacement surgery is generally a safe procedure, but that people need to be very DVT-aware.
During the surgical consultation, patients should discuss blood clots and not leave the consultation without knowing precisely what the prevention measures will be.
Some surgeons will prescribe blood thinners for only the hospitalization duration.
“Despite the use of blood thinners, patients undergoing knee arthroplasty continue to remain susceptible to clot formation for several weeks following surgery,” says the paper.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sasirin pamai
Source: sciencedaily.com/releases/2011/07/110727121658.htm
Retrievable (Temporary) IVC Filters vs. Permanent: Pros & Cons
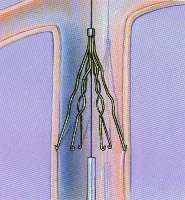
Wondering about the pros and cons of retrievable IVC filters vs. permanent ones?
Since you’re here you probably know what an IVC filter’s job is: prevent pulmonary embolism.
The largest study on following people with retrievable IVC filters supports the guidelines generated by the SIR: Society of Interventional Radiology.
An IVC filter can be placed temporarily or permanently.
IVC stands for inferior vena cava (a large vein involved in circulation).
A blood clot in a deep vein is called a deep vein thrombosis (DVT). If the clot breaks loose and travels to the lung, it becomes a pulmonary embolus, which can choke off a person’s oxygen supply in seconds.
Most people with DVT are treated with a blood thinner drug, which usually prevents pulmonary embolus.
An IVC filter will block a migrating DVT from getting into the lungs. Some people are not suitable candidates for blood thinners, such as trauma patients.
There’s also people who, despite being treated with blood thinners, develop DVT anyways.
In 2007, 167,000 IVC filters were placed. In 2012, at least a quarter of a million were placed.
Most of these filters were meant to be permanent. A type called “retrievable” can be later removed by a doctor.
However, some retrievable IVC filters can fracture or even migrate to other portions of the bloodstream.
The FDA has recommended that doctors who implant these devices routinely consider the risk/benefit ratio for every patient.
Removal should be considered for patients no longer at risk for PE.
Some Big Considerations
“In 2019, if a filter is deemed necessary, it probably should be a retrievable one, but plans need to be made for removal at the time of placement,” says Steve Elias, MD, FACS, a vein specialist with Englewood Health in NJ.
“The biggest problem with retrievable filters is that they are not retrieved,” continues Dr. Elias. “They work well. If one is 100% sure it never needs removal, then a permanent filter should be placed.”
A retrievable filter may need to be taken out within four to six weeks of placement. Waiting too long for removal would give the filter a chance to become too firmly attached to the inferior vena cava to be removable.
One of the reasons a retrievable filter may end up in the patient’s body too long is that the patient loses touch with their doctor during the crucial follow-up period.
Hence, selection of which patients should receive a retrievable IVC is very important.
Patients with retrievable IVCs or who are being considered for one should have very close communication with their doctor.
Those with the filters should talk to their interventional radiologist, plus other physicians, about any concerns.
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: sciencedaily.com/releases/2011/11/111128121545.htm
How Often Does Someone in the U.S. Die from a DVT ?

The rate at which a deep vein thrombosis kills an American will floor you.
Every year in the United States, a significant number of people die from VTE: venous thrombus embolism.
“DVT kills more people than accidents, cancer and AIDS combined,” says Steve Elias, MD, FACS, a vein specialist with Englewood Health in NJ.
“It is common all over the world — but perhaps not recognized as often in developing countries.”
How often does an American die from DVT?
Every five minutes, reports the Vascular Disease Foundation.
This translates to 100,000 to 180,000 Americans every year succumbing to deep vein thrombosis.
Though most VTE isn’t fatal, there’s no way to tell, in any given patient with a DVT, whether or not the clot will break off and travel to the lungs, how big the breakage will be and/or exactly where the broken fragment will lodge.
Keep in mind that many lives are saved because the symptoms of a deep vein thrombosis are difficult to ignore, prompting people to seek medical attention, leading to diagnosis and treatment.
Some estimates are higher, such as 300,000 Americans a year (Journal of Vascular and Interventional Radiology, Oct. 30, 2009).
The Vascular Disease Foundation says that just about anyone can develop a deep vein thrombosis under the right circumstances, and the more risk factors present, the more likely you’ll develop the condition.
The VDF names the following risk factors: smoking, obesity, sitting for more than six hours when traveling, prolonged bed rest, family history, cancer and cancer treatment, increasing age, recent major surgery (particularly orthopedic), and hospitalization for illness.
DVT symptoms may consist of pain, tenderness or aching in one or both legs; change in skin color (usually red or purple); skin hot to the touch; and swelling. Be especially suspicious if these symptoms occur in one leg.

Scientific Animations, Creative Commons/BY-SA/Attribution-ShareAlike 4.0 International
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Ocskay Bence
Sources:
sciencedaily.com/releases/2011/03/110305105233.htm
sciencedaily.com/releases/2009/10/091027132430.htm
Can a DVT Go Away on Its Own?
A deep vein thrombosis (DVT) can be deadly, but does this mean it can’t go away on its own?
If you suspect a DVT, get to the emergency room, because a deep vein thrombosis can travel to the lungs and cut off your air supply, killing you.
My mother was diagnosed with a “big DVT” in her jugular vein soon after coronary bypass surgery, but, believe it or not, it went away on its own.
Just when the DVT formed is not known; it may have formed during surgery or in ICU recovery.
It fattened her arm and I insisted on an ultrasound. However, nothing was done for this blood clot because the infusion of a clot-busting drug, said the doctor, would have put her at risk for lethal internal bleeding.
She was already on the blood thinner Coumadin as a regular post-bypass therapy, and thus, administration of a clot-busting drug was contraindicated.
So I asked the doctor, “What about this DVT in her neck? Can’t anything be done to break it up?”
He said that there was a “slim” chance that it would dislodge (travel to lungs).
I was told that her body would “reabsorb” the DVT, that it would “resolve on its own.”
How true is this?
“DVT, when it resolves, usually does “resolve’ on its own,” says Steve Elias, MD, FACS, a vein specialist with Englewood Health in NJ.
“Even when patients are using blood thinners for DVT treatment, the blood thinners’ role is to prevent further DVT from developing,” continues Dr. Elias.
“Blood thinners do not dissolve DVT. The patient’s own body’s enzymes do.
“So yes, in theory, a patient not on blood thinners can resolve their DVT.”
Sit and Wait
So over the next several days after her surgery, I knew that this big DVT was just sitting in my mother’s neck.
I knew that there was nothing to stop a piece of it, or the whole thing, from becoming renegade and getting into her lungs and becoming a pulmonary embolism.
I watched her arm like a hawk over the next several days to see if it was getting even bigger.
However, I noticed that the alarming swelling was gradually going down. Ultimately, the swelling disappeared.
At some point along the way a second ultrasound showed that the DVT had gone away.
Nevertheless, if you suspect a DVT, don’t think it will always “reabsorb” or “resolve on its own.”
Even if you’re young or an athlete. DVT means ER.
At the time of my mother’s deep vein thrombosis, I didn’t know about special filters that can be inserted in the patient’s vein to trap blood clots that have migrated from their origin and are heading towards the lungs.
However, filter insertion is usually for patients who cannot take Coumadin or other anticoagulant drugs, or when these drugs are not effective.
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: BruceBlaus/CreativeCommons
DVT Prevention with a Treadmill Desk
A treadmill desk will go a very long way at helping prevent DVT: deep vein thrombosis.
Perhaps you’ve heard that prolonged sitting during air travel or road travel is a risk factor for developing a deep vein thrombosis (DVT).
Likewise, sitting for long periods in general can put a person at risk for a DVT, and this was first reported in the January 1954 New England Journal of Medicine.
And a report titled “eThrombosis” appears in the Feb. 2003 European Respiratory Journal, which describes venous thromboembolism that’s associated with immobility.
Unfortunately, the commercial invention of the treadmill desk didn’t occur until years later.
More and more office and home workers are using treadmill desks, the only way to eliminate all their excessive sitting.
The risk of DVT from excessive sitting is no secret, as more and more studies pile up pointing this out, such as the 2010 report in the Journal of the Royal Society of Medicine titled “Prolonged work and computer-related seated immobility and risk of venous thromboembolism.”
Venous thromboembolism is the term that incorporates both DVT and PE — pulmonary embolism — which can result when the blood clot partially or in whole dislodges and travels to the lungs, causing a potentially fatal outcome.
Long stretches of sitting does slow the blood flow in the legs; it doesn’t matter if you’re on an airplane, watching TV or at a computer.

Shutterstock/fizkes
A report in a 2007 Journal of Thrombosis and Haemostasis says that after 90 minutes of sitting (without intermittent relief exercise), blood flow to the vein behind the knee drops by 40 percent.
Treadmill Desk Solution to DVT from Prolonged Sitting
You needn’t walk fast on a treadmill desk to make it work against DVT development. Even a one-half-a-mile per hour walk will keep the blood flowing in your legs.
The Centers for Disease Control recommends that desk workers raise and lower their heels while keeping their toes on the floor, and repeating this but with the heels on the floor, and then tightening and releasing the leg muscles.
As a former personal trainer, I recommend simply exiting the chair and doing high knee marches, going up and down on the toes, leaning the hands on the desk and extending the legs, or walking about the room.
However, this requires keeping track of time, and for a busy desk worker, 90 minutes can fly by while they sit immobile without them realizing it.
A treadmill desk will solve this problem, keeping you in constant motion. I myself have a treadmill desk, and once you get absorbed in your work, you can easily forget that you’re walking.
Don’t take a chance; consider investing in a treadmill desk to help prevent DVT.
You need not spend ALL of your computer time walking at the desk.
You can move your laptop back and forth between a sit-down and a treadmill desk.
Or, a more convenient option is to get two computers: one that’s always at the treadmill desk and one that’s always at your sit-down station.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Source: patientblog.clotconnect.org/2012/10/22/behind-the-headlines-does-eating-lunch-at-your-desk-increase-blood-clot-risk/#more-1757
DVT Detection with Urine More Accurate than D-Dimer

A urine test may soon replace the D-dimer to screen for DVT (deep vein thrombosis) blood clots.
Imagine being in the ER with a suspected DVT (deep vein thrombosis), and instead of getting your blood drawn for the D-dimer test, you’re asked to give a urine sample because the nurse says, “We can see if you might have a blood clot by analyzing your urine.”
This scenario may soon be standard in ERs, thanks to a study led by Timothy Fernandes, MD.
The study report was published in 2014, but detecting a deep vein thrombosis with the patient’s urine is still not a standard procedure in emergency rooms.
But imagine the possibilities:
Detection of a DVT through urine would make it simple and easy to do in a regular medical clinic.
My mother has had her D-dimer level evaluated at least three times when she presented to the ER with symptoms that a DVT can cause.
Each time, the D-dimer was positive, and because of that, a CT scan of her chest was ordered to see if there was blood clot in her lungs (pulmonary embolism).
The CT scans were negative all those times. A positive D-dimer doesn’t always mean a blood clot. However, this tests helps guide physicians in what to do next.
“Physicians, especially in the emergency room, are often faced with patients with symptoms and risk factors concerning for DVT/PE,” says Dr. Paramjit (Romi) Chopra, MD, founder of the Midwest Institute for Minimally Invasive Therapies (MIMIT), an interventional radiology and endovascular therapy practice.
“Like most screening exams, D-dimer is a blood test with a high sensitivity and low specificity for diagnosing PE.
“However, some studies have shown that fibrinopeptide levels in the urine may have higher diagnostic accuracy than D-dimer.
“Ultimately, the key to diagnosing DVT/PE is a thorough history and physical exam by an experienced physician.”
What is fibrinopeptide?
FPB is a compound that’s released when a blood clot forms, and gets excreted through urine.
Dr. Fernandez says in the report that the urine test is more accurate than the D-dimer.
That’s because the D-dimer protein fragment becomes present in the blood after the DVT begins to break down.
Whereas the FPB is present in the blood before the DVT begins degrading, while the thrombus is still active.
The urine test, though, is still not refined enough to become a replacement for the D-dimer test.
Dr. Chopra combines his Eastern roots and 30+ years’ Western experience to unify the best of both worlds at MIMIT to treat venous disease, peripheral artery disease and musculoskeletal disease.
combines his Eastern roots and 30+ years’ Western experience to unify the best of both worlds at MIMIT to treat venous disease, peripheral artery disease and musculoskeletal disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/New Africa
Source: ciencedaily.com/releases/2014/05/140518164105.htm
Sudden Feeling Shortness of Breath with No Other Symptoms

That’s one of the most frightening symptoms: a sudden feeling of being short of breath even though you’re at rest.
Even if the sensation of being short of oxygen is your only symptom — it’s still scary and should not be ignored.
A sudden feeling of being out of breath or that of not getting enough air isn’t always caused by a heart problem.
You May Have a Pulmonary Embolism
“One of the most common presenting complaints associated with pulmonary embolism is shortness of breath,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
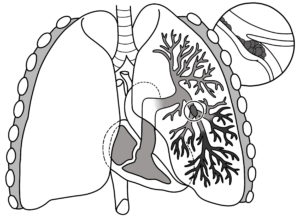
“In a pulmonary embolism, a clot breaks loose from somewhere in the body – typically a leg vein – and lodges in an artery in one or both lungs.
Pulmonary embolism
“The affected areas in the lung lose the ability to transfer oxygen into the bloodstream.
“If a large enough area is affected, the body senses a drop in oxygen, leading to a sensation of shortness of breath.
“Different conditions lead to different types of shortness of breath.
“Many conditions that cause shortness of breath – like asthma – cause the sensation that a patient cannot move enough air in and out.
“A person with a pulmonary embolism does not have trouble moving air in and out, but they still feel like they are not getting enough air.”
To have an idea of what this could feel like, walk on a treadmill at two mph and five percent incline – assuming that your body is not used to incline walking.
- Do NOT hold onto the machine, not anywhere. Hands are free.
- Breathe only through your nose; do not open your mouth to take in air – not even a sliver.
- Keep the mouth sealed.
- You will not have difficulty moving air in and out – no issue with the mechanics. But you will feel shorted of air.
Shortness of Breath May Be the Only Symptom
Research from Saint Vincent’s Medical Center in Bridgeport, Connecticut, revealed in 2012 that out of 334 patients with a confirmed pulmonary embolism, 29 percent had difficulty breathing without any other symptoms.
Three Key Symptoms of a Pulmonary Embolism
- A sensation of difficulty breathing or of being short of breath
- Chest pain
- Cough
This sounds like a heart attack, but you can have a perfectly normal heart while experiencing a pulmonary embolism – which can kill in minutes without emergency medical attention.
Any combination of these symptoms can occur from a pulmonary embolism — including one of them in isolation.
The biggest risk factor for a P.E. is a deep vein thrombosis.
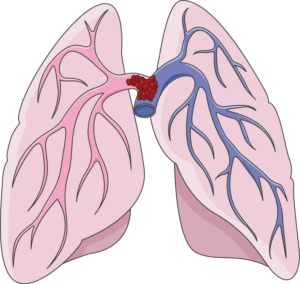
A “saddle” type pulmonary embolism, plugging up the area where the pulmonary artery splits off into each lung. This can cause death in minutes. Laboratoires Servier, CC BY-SA/creativecommons.org/Wikimedia Commons
Risk Factors for a DVT
- Extended air travel or hours driving without a break
- Smoking
- Obesity
- Lack of exercise
- Use of birth control pills
- Pregnancy
- Recent joint replacement or abdominal surgery
- Excessive bed rest
- Old age
- Family history of DVT
- Heart disease
If you suddenly “can’t breathe” or have difficulty breathing, it’s important to know what your very recent history of activities has been, such as having recently gotten off a plane after a long flight or being on birth control while maintaining a smoking habit.
This information will help in the ER, though the symptom complaint of “trouble breathing” or “shortness of breath” will always net a blood test to check for the presence of a blood clot.
 Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, jcomp
Source: sciencedaily.com/releases/2012/10/121022081023.htm
Deep Vein Thrombosis Treatment: Drugs plus Ultrasound

Can DVT treatment be more successful with both ultrasound and drugs, rather than just the clot-busting medications alone?
DVT stands for deep vein thrombosis, a life-threatening blood clot that can result from surgery (especially joint replacement) as well as extended air travel or prolonged home bed rest.
The typical treatment is administration of a clot-busting drug intravenously.
A study from the Emory University School of Medicine shows that ultrasound plus drugs will help break up a DVT.
But more studies are needed — and large-scale ones — to obtain a final verdict.
“It was a small study, and the CHEST guidelines (which is what most physicians follow) does not recommend this method above others,” says Steve Elias, MD, FACS, a vein specialist with Englewood Health in NJ.
Dr. Elias adds, “Small studies give us food for thought but should not change practice patterns completely.”
Most DVTs form in the calves but can form anywhere.
A deep vein thrombosis can break loose from its positioning in the blood vessel and travel into the lungs, where it will then block blood flow.
At this point it’s called a pulmonary embolism. A massive pulmonary embolism can kill in less than a minute.
It severely impairs blood flow from the heart to the lungs, causing a sudden drop in oxygen levels and extreme strain on the right side of the heart.
This can be detected with a stethoscope; the right side pumps de-oxygenated blood to the lungs to be re-oxygenated.
In severe cases, a PE can lead to cardiac arrest and death almost immediately.
DVT Risk Factors
- Older age
- Smoking, even if you’re a younger adult
- Overweight, particularly severely
- Pregnancy
- Birth control pills
- Hormone replacement therapy
- Having a pacemaker
- Family history of DVT
- Extended bed rest, air travel or road travel — even if you’re fit and healthy
- Heart failure (chronically weak pumping action of the heart)
- Cancer treatment
- General anesthesia (especially in combination with morbid obesity)
- Major surgery, particularly hip and knee replacement; and abdominal surgery
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Casa nayafana
Source: sciencedaily.com/releases/2008/11/081123150253.htm
Can Pulmonary Embolism Cause Fainting? Yes, Especially After Flying
There’s a unique circumstance under which a fainting episode may be caused by a pulmonary embolism.
A pulmonary embolism results when a deep vein thrombosis (“DVT” or blood clot) breaks loose and travels to the lungs.
Extended air travel can cause this problem.
A study concludes that if a person faints soon after air travel, this could signal a pulmonary embolism (PE).
However, fainting is generally not a common symptom of a pulmonary embolism.
But Fainting CAN Happen from a Pulmonary Embolism
“A pulmonary embolism cuts off blood flow to a portion of one or both lungs,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
“When a segment of lung loses its blood flow, it becomes unable to transfer the oxygen the body needs to survive.
“If the affected area is large enough, it’s possible that the patient will not be able to oxygenate the blood well enough to remain conscious.
Shutterstock/Artemida-psy
“If an embolism is large, another possible effect is a serious interruption of blood flow.
“A major blockage of a pulmonary artery can cause the amount of blood transiting the heart – the ‘cardiac output’ – to drop dramatically.
“In some cases the output of the heart may drop so low that consciousness cannot be maintained.”
Fainting Is More Suspicious for a Pulmonary Embolism if It Occurs Shortly After Air Travel
Research was presented at CHEST 2012, the annual meeting of the American College of Chest Physicians (ACCP).
Dr. Robert Rifenburg, MD, of Resurrection Medical Center in Chicago, and lead author of a study, said at the meeting, “Fainting may be an atypical symptom of PE, but fainting associated with recent air travel is a dangerous combination.”
PE that’s associated with recent air travel is also more likely to be the saddle type (blocking the pulmonary artery where it splits off into each lung), and this type is bigger and more life-threatening than other pulmonary emboli.
If you ever faint after recent air travel, get to an emergency room ASAP.
Dr. Rifenburg also said that a pulmonary embolism following a fainting episode after being in a plane very likely means that the situation is life-threatening.
The saddle type can cause sudden disruption of blood flow to the brain, which in turn causes fainting.
The study did not examine for an association between length of air travel and likelihood of fainting from a pulmonary embolism.
Nevertheless, Dr. Rifenburg speculates that a longer flight would put a person at a higher risk for a saddle embolism.