What Causes Red Itching Bumps on the Fingers?
Itchy red bumps on the fingers can have several causes.
Regardless of cause, the No. 1 rule is that you should avoid scratching, as this can make the condition worse — regardless of the cause.
One possible cause, believe it or not, is warts.
Warts are “a viral condition you pick up from the environment,” says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
The viral infection is located in the top layer of the skin. The viruses are of the HPV type and can get into the skin via a little scratch.
The cells grow rapidly, forming a wart – which can itch.
But warts typically will not grow in clusters all over your fingers. Other conditions can.
Dr. Goldernberg continues, “Papular (bumpy) eczema can also cause red bumps on the hands and is usually treated with topical creams.”
Eczema will itch worse than a few warts. The last thing you’ll want to do is get into a scratching frenzy.

The pinkish red bumps of eczema. Maslesha,CC BY-SA
Scratching at eczema can cause the area to crust and even ooze.
When you scratch, you irritate the already inflamed skin, which can exacerbate the itching and lead to more severe flare-ups.
This creates a cycle of itching and scratching that makes the eczema symptoms worse and more difficult to control.
Plus, scratching increases the risk of infection. As you scratch, you break the skin, which can allow bacteria, viruses or fungi to enter and cause infections.
These infections can complicate the eczema and make the condition more challenging to treat, often requiring additional medical intervention.
Scratching also delays the skin’s healing process. Continuous irritation from scratching can prevent the skin from recovering properly, extending the duration of the eczema flare-up and making it harder to manage over time.
The damage caused by scratching can lead to further complications, including thickened and rough patches of skin known as lichenification.
Frequent scratching can lead to long-term skin damage. The repetitive trauma can cause permanent changes in the skin, such as scarring or thickening, which may be difficult to reverse.
Your dermatologist will prescribe the right medication to treat eczema, which is common and which can also occur on the elbows and make them itch like mad.
If the itching is driving you batty, you can gently wrap gauze around your fingers overnight or while you’re watching TV or any activity during which you are not using your fingers too much.
Dr. Goldenberg continues, “Bites can occur on the hands, and can be caused by mosquitos or bed bugs – see your dermatologist for tests to rule this one out.”
Bottom line: You certainly do not have to worry about a serious disease causing red bumps to be scattered all over your fingers or hands, no matter how badly they itch.
But remember: Avoid scratching and instead see a dermatologist for proper treatment.

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Image Point Fr
Skin Peeling Like Crazy On Your Hands: Doctor Explains

A dermatologist says there can be two common conditions that cause a lot of skin peeling on your hands.
These conditions are very common, says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
The conditions are psoriasis or eczema.
Dr. Goldenberg explains, “Psoriasis is a genetic condition in which the skin forms scaly patches and plaques, anywhere on the body, including hands.
“This condition may also be associated with arthritis and internal disease, such as heart disease, stroke and diabetes.”
Psoriasis is an autoimmune disease, and sometimes, patients experience the joint problems before they experience any skin problems such as peeling on the hands.
“The treatment of psoriasis depends on the severity of disease, including topical creams, certain oral medications (pills) and biologic injections.”
Eczema
Dr. Goldenberg says, “Eczema is a very common condition that is genetic in nature. Hand eczema is the most common manifestation of this disease in adults.
“It usually presents with scaly patches and may be related to other allergies. Treatment is usually with topical creams.”

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Monster e
Why Your Eyelid is Itchy & Swollen: Doctor Explains
A doctor explains the most common cause of a swollen, itching eyelid.
And the most common cause of this is contact dermatitis, says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
He further explains, “This is more common in female patients than men. Common allergens include nail polish, hair care products, makeup and gold jewelry.
“Investigative work may be needed here to find out the exact cause of the allergy.
“Your dermatologist may suggest patch testing – a test to see what it is you are allergic to.”
Patch Testing
Patch testing for dermatitis is a diagnostic procedure used to identify specific allergens or irritants that might be causing allergic contact dermatitis.
During the test, small amounts of various potential allergens are applied to the skin, using adhesive patches.
These patches remain in place for about 48 hours, after which they are removed and the skin is evaluated for reactions.
The test helps determine which substances trigger dermatitis by monitoring the skin for signs of an allergic reaction, such as redness, itching or swelling.
The results guide treatment and management by identifying which substances to avoid.
Patch testing is typically conducted by a dermatologist and is particularly useful for patients with chronic, unexplained dermatitis or those who have not responded to standard treatments.
What can you do about an itching, swollen eyelid?
Dr. Goldenberg explains, “Treatment can be a bit frustrating, since sometimes even if you remove the allergen, the condition may persist.
“Topical creams may be helpful. Caution should be exercised with using topical steroids on the eyelids.”
Make sure you follow the instructions.
More About Contact Dermatitis and the Eyelid
You’d be surprised at what can come in contact with your eyelid every day or several days a week — enough to cause itching and swelling.
In some cases the contact is unintentional such as with hand cream and tweezers.
Do any of these apply to you?
- Moisturizer
- Hand cream
- Tweezers
- Allergens even in eye drops and contact lens solutions
- Dust mites. Yes, they live on the eyelid.
- Pet dander
- Perfume
Keep a daily journal about what just possibly — even if it seems silly — could be making unintentional contact anywhere around your eye.
This includes from housecleaning agents that get onto your fingertips, and then before you wash your hands, one of those fingertips rubs a tired eye — transferring the chemical allergen to the lid.
Other causes of an itchy swollen eyelid you’d never think of.
- Very cold or hot temperatures
- Very dry or humid air
- Dust in the air
- The new carpet, memory foam pillow or mattress. Their “off-gassing” could be sending chemical allergens straight to your eyelid.

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Missing Child in a Store? Where to Look First!
If your child goes missing in a store, the first place you should look is probably not where you’d think.
Where was the first place Adam Walsh’s parents searched when the 6-year-old child went missing at a mall Sears store on July 27, 1981?
They spent two hours searching inside the store for their missing boy, and then they called the police, say reports such as from nbcnew.com.
Reve Walsh wasn’t looking away from Adam for long by the time she returned to the toy section to retrieve him and saw that he was missing.
This scenario is actually common:
Parent “looks away for just a few minutes,” and then the child goes missing. If it turns out the child was abducted (lured away by a predator), it’s very fair to speculate that a mother dramatically increases her chances of catching the predator in the act — if she dashes towards the store’s nearest exit, which is likely where the predator is heading — victim in tow.
Or maybe the parent will spot the predator and her child outside walking towards his car, which again, puts her in a position to thwart the abduction.
Parents who worry about their child going missing in a store or mall should know the location of the nearest exit at any given time.
I asked Robert Siciliano, a personal safety and security expert, where is the first place a parent should look in a store if that’s where a child goes missing.
“As a parent, I’d go directly to the front of the store, near the entrance, so I can watch the door,” explains Siciliano, CEO of Safr.Me.com.
“Customer service is usually near the front as well. Bring it to the attention of customer service and they will bring it to security. Usually a code goes out on a PA alerting employees to be on the lookout.”
In the Walsh case, the PA system summoned him by name. Preceding that, however, while his mother was frantically calling out for him in the toy section and asking nearby shoppers if they’d seen him, those crucial minutes were apparently being used by the predator to whisk Adam outside to his vehicle.
What person, who abducts a child, lingers inside the store with the victim?
They usually have it all planned out. The moment they have gained the child’s trust, they lead him or her towards the nearest door to the parking lot.
Once the child is out there, while the frantic parents are searching inside the store, it’s a done deal.
Siciliano says that, if his own child went missing in a store, after alerting the security there, he’d give his mobile number to the store manager and look outside.
When children go missing in stores and then later turn up murdered or never found, one has to wonder if the abduction process could have been intercepted in at least half these cases, had the parent immediately bolted out the nearest exit.
It’s inconceivable that a perpetrator, once he has the child’s hand, would continue hanging out inside the store or mall, knowing full well that a search is in progress.
“And there’s nothing wrong with causing a little scene to get other parents to be on the lookout too,” says Siciliano. “I’ve done it myself.”
This can be done while the parent rushes towards the exit — hollering out that someone possibly kidnapped their child.
Usually, when a child goes “missing” inside a store, they’re located safe and sound inside the building, having innocently wandered off.
But no parent spends the rest of their lives regretting that years ago, they had created a scene “for nothing” inside a store, bolted outside and searched the parking lot for a stranger with their child.
 Robert Siciliano is a private investigator fiercely committed to informing, educating and empowering people to protect themselves and their loved-ones from violence and crime — both in their physical and virtual interactions.
Robert Siciliano is a private investigator fiercely committed to informing, educating and empowering people to protect themselves and their loved-ones from violence and crime — both in their physical and virtual interactions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sources:
nbcnews.com/id/28257294/#.UmoSrnCor20
trutv.com/library/crime/criminal_mind/psychology/child_abduction/9.html
http://www.nbcnews.com/id/28257294/#.UmoSrnCor20http://www.nbcnews.com/id/28257294/#.UmoSrnCor20
Crohn’s Disease: Early vs. Long-Term Symptoms

“Crohn’s is the inflammation of the intestine, from mouth to anus, usually in the small or large bowel – or both,” says gastroenterologist Sander R. Binderow, MD.
“Some patients have anal Crohn’s or Crohn’s of the stomach; however, that is very rare,” adds Dr. Binderow, who’s with Atlanta Colon & Rectal Surgery.
This disorder is an inflammatory bowel disease that is actually associated with an increased risk for colon cancer.
Microscopic colitis is also an inflammatory bowel disease, but is not associated with an increased risk of any kind of cancer. Microscopic colitis is often misdiagnosed as irritable bowel syndrome.
“Crohn’s presents as a diarrheal-type illness, where the large intestine lining is inflamed, and with Crohn’s, there is not as much blood,” says Dr. Binderow.
“Patients tend to be ill, where they lose a significant amount of weight, do not eat and have a loss of appetite.”
If you think these symptoms sound like those of colon cancer, you are correct.
Long-term Symptoms of Crohn’s Disease
“Long-term symptoms can include a stricture, which causes abdominal pain, nausea and vomiting, narrowing of the colon and fistulas,” says Dr. Binderow.

If you’ve been diagnosed with Crohn’s disease, you should be vigilant about colon cancer screening.
You can begin this with Cologuard, a non-invasive way to screen for colon cancer.
It’s a test that you take at home. Using the latest in DNA technology, Cologuard identifies precancerous cells.
If your test result comes out positive for this, your next step should be a colonoscopy.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Zetar Infinity
Constant Need to Burp: Most Likely Cause

A GI doctor explains what the most likely cause is if you constantly need to burp.
The important thing to note here is if frequent burping is your only symptom, rather than it’s also accompanied by (not necessarily at the exact time that you burp) concerning symptoms such as abdominal pain, blood in the stools, unexplained weight loss and undue fatigue.
So let’s say that lately, you just seem to be burping a lot, but otherwise feel as healthy as ever.
“Most people talk while they eat, which leads to burps and farting,” explains gastroenterologist Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
“There is a possibility of a small bowel obstruction if a person is burping, but in that case the patient would be more concerned about the pain they are experiencing and would go to the doctor for that obvious symptom rather than burping alone.
“It is possible a patient could be burping more often if they suffer from reflux; however, most times if the symptom of burping is the only one that the patient is experiencing, they are likely talking more while they eat.”
Have you been going out to dinner more frequently, and hence, talking more while you eat? Try not to gulp air as you take in food or drink beverages.
What if you don’t talk when you eat, yet you’re still frequently burping?

Shutterstock/Aaron Amat
It’s entirely possible that you’re still swallowing excessive air as you eat and drink — especially if you’re a fast eater.
But what about the question, Can excessive burping actually be a symptom of cancer?
Yes, it can. In this article, Dr. Maxwell Chait explains what kinds of cancer can cause this seemingly innocuous symptom.
What about colon cancer? If you’ve been experiencing a lot of burping lately, chances are extremely unlikely that this is being caused by cancer of the colon.
However, other GI symptoms can be caused by this disease, such as abdominal pain, constipation, blood in the stools (which may appear dark, not necessarily red), unexplained fatigue and unintentional weight loss.
By the time symptoms of colon cancer begin presenting, the disease has spread beyond local confines. That’s why it’s so important to be screened for it.
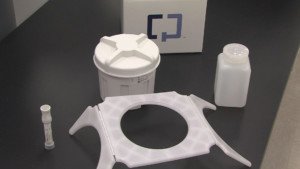
Cologuard
You can start with Cologuard, a non-invasive home test that utilizes state-of-the-art DNA technology to identify abnormal cells.
If you have abnormal cells, the next step is a colonoscopy.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/elbud
Bits of Foam in Diarrhea Explained by Doctor

What are the “bits of foam” that someone might see in their diarrhea?
And can this ever be a sign of a disease?
These are questions I asked of gastroenterologist Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
“Foam in diarrhea can occur in the small intestine, when air combines with the bowel movement that is in rapid transit, which is the nature of diarrhea,” explains Dr. Binderow.
“The diarrhea combines with air, creating small foam. This is not a sign of any type of disease when it is observed alone with no other symptoms.”
So next time you see foam or white fuzzy mucus in your diarrhea, remind yourself that it is the product of air combining with your bowel movement.
However, there are other features that you should be concerned about that are not related to bits of foam.
For example, do you see what appears to be blood in your stools?
Or does your diarrhea alternate with going days without any bowel movement?
This is especially concerning if it’s a new phenomenon for you.
These are concerning signs, and though colon cancer can be one of the causes, there are numerous other non-malignant causes for such symptoms.

If you have not yet had a colonoscopy but are concerned — yet are fearful of having a colonoscopy — you may want to consider a preliminary step: Cologuard, a non-invasive screening test that you can give to yourself at home.
Using the latest DNA technology, Cologuard can identify abnormal cells in your stools.
If the test results show this, you would then need to undergo a colonoscopy, which usually takes around 25 to 45 minutes and can be done under sedation.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/sasha2109
Diarrhea vs. Loose Stools Comparison

The line between diarrhea and “loose” stools is very fuzzy; at what point are loose stools actually diarrhea?
Is there a way to test the substance to classify it as one or the other?
“To answer, one must specify that the diarrhea is a medical term and diagnosis, and ‘loose’ stools are a patient observation,” says Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
“A patient could have diarrhea; however, it is also possible that they just have loose stools.
“Diarrhea includes bowel movements more than three times per day with copious amounts, and it can be mixed with mucus.
“If a patient has acute diarrhea, it is often the body’s response to something a person has eaten and needs to get rid of.
“A doctor does not normally recommend treating, and rather, it is best to let the body process the issue.
“If it continues for weeks at a time, it is then necessary to bring to the attention of a physician.”
Colon Cancer Worry
Diarrhea or “loose” stools, in and of themselves, are not common features of colon cancer.
The issue with colon cancer is if diarrhea (or what the patient may perceive as loose stools) alternates with constipation (going days without a bowel movement).
Nevertheless, if loose stools or diarrhea have you worried about colon cancer, it is recommended that you have a non-invasive screening exam for this disease.
Cologuard is non-invasive and can be done in the convenience of your home.

Cologuard uses the latest advances in DNA technology for identifying any abnormal cells in the sample.
If the test results are positive for abnormal cells, you would then be recommended to follow up with a colonoscopy.

Colonoscopy
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
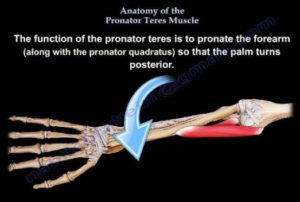
What Is Pronator Syndrome: Causes, Solutions, Prevention

Pronator syndrome can cause painful symptoms in the hands and forearms that mimic carpal tunnel syndrome.
Pronator syndrome is when the pronator teres muscle of the forearm presses upon the median nerve, the same nerve that’s involved in carpal tunnel syndrome.
Pronator teres syndrome is a nerve entrapment condition. The median nerve gets compressed by the pronator teres muscle; the median nerve is located beneath the superficial head of this forearm muscle.
“Activities involving repetitive wrist and forearm movements are thought to increase the risk of developing pronator syndrome,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“Pronator syndrome occurs secondary to increased pressure on the median nerve in the forearm.
“These repetitive motions can lead to muscle hypertrophy and/or swelling, increasing the pressure over the nerve as it travels through the forearm.
“This is often in conjunction with a patient’s underlying anatomy which may predispose them to developing this in the first place.”
As a former personal trainer, I’m very familiar with the pronator muscle (reverse arm curls target it).
This muscle is responsible for the wrist joint action of pronation, i.e., turning the forearm over so that the palm faces downward or behind you, depending on where your hands are in space; or, if the hands are elevated, turning the palms facing away from you (as in a pull-up).
Though the compression site is in the upper forearm, the symptoms will not only be felt in this area, but also will affect the hand and fingers.
The median nerve controls movement and sensation in most of the hand.
When you want to move your thumb, for instance, a signal from the motor control region of your brain travels down your neck to the median nerve, which extends from the neck region (spinal cord) and runs the entire length of the arm, with its final distribution to most of the hand, including the thumb.
The electrical nerve impulse signal, that originated from your brain, will zip down the median nerve all the way to the thumb, where the nerve distributes to thumb muscles.
The electrochemical impulse will cause the thumb muscle to contract: You just moved your thumb. These nerve signals travel about 50 meters per second.
If the median nerve is compressed somewhere along the way, some of the nerve signal from your brain will never get past the compression point, and hence, why movement in the fingers can be limited or “stiff.”
Numbness is also a symptom for the same reason in reverse:
Sensory neurons normally send signals up the median nerve to the sensory interpretation center of the brain.
If there is a blockage of these signals at the compression site, all the signals won’t make it to the brain, and hence, numbness, rather than a full sensation of feeling.
In addition to compromised motion and numbness, pronator syndrome also causes pain, including in the hand.
The median nerve distributes to the thumb, index and middle fingers, and the half of the fourth finger that faces the middle finger.
Face your right palm towards you. Imagine a line running down lengthwise the fourth finger, dividing it in half. Continue “drawing” that line all the way to the wrist.
Now, imagine shading the portion of your hand and fingers to the right of this imaginary line. This is the area impacted by pronator syndrome.
In other words, the other longitudinal half of the fourth finger, plus the entire pinky and outer portion of the palm, are not affected.
Nevertheless, these symptoms can also be caused by carpal tunnel syndrome, despite what you might have read or will read. Wrist motions should not aggravate pronator teres syndrome symptoms.
Misdiagnosis
A chiropractor misdiagnosed my mother with pronator teres syndrome based on questioning her and feeling her arm for pain triggers.
Then an ER physician misdiagnosed her; he suspected nerve compression at the neck and ordered an MRI. The MRI showed cervical disc degeneration and he said, “It’s what I suspected: nerve compression of the neck.”
The most definitive test to rule in or out nerve entrapment conditions is the EMG test.
An EMG test ruled out cervical compression and pronator syndrome in my mother, and solidly confirmed carpal tunnel syndrome.
Interestingly, the neurologist who performed the EMG test, prior to the test, was very convinced she had pronator syndrome.
But an EMG test does not lie. It revealed a nerve signal conduction blockage at the wrists of both hands: carpal tunnel syndrome.
Treatment
Treatment for pronator syndrome may consist of simply massage.
A chiropractor might be convinced that chiropractic manipulation can correct the problem over a number of visits.
If conservative treatments aren’t successful, then surgery is a final resort.
Prevention
Dr. Oheb explains, “Ways to reduce the risk of developing pronator syndrome mostly involve proper warm-up and stretching before strenuous activity.
“Also, maintaining good strength and flexibility through regular exercise can be preventative.”
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Photographee.eu
Strength Tests if You Fear ALS for Legs & Upper Body
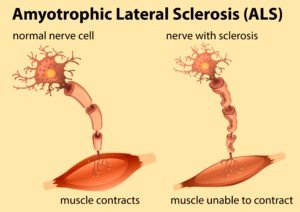
Ever wonder what strength tests for ALS that a healthy person could pass?
Here are strength tests for the lower and upper body: legs, arms, shoulders and hands.
As a fitness expert and former personal trainer, I’ve devised some strength tests that should put your mind at ease about ALS if you’ve been freaking that you might have this disease due to muscle twitching, muscle cramps or perceived weakness.
If you can perform all of these strength tests, then you’ll have much less fear that you have ALS.
If you’ve been spending hours every day doing strength tests for ALS, you can finally stop the obsession, because these strength tests I’m about to describe are official ALS strength tests given by physicians for neurological exams.
You can perform these ALS strength tests with or without a partner.
Before engaging in these strength tests, there’s a few things you should know.
“I think that self-assessment of strength is a tool that can be used to reassure in some cases,” begins Mitzi J. Williams, MD, clinical neurologist with Morehouse School of Medicine and clinical advisor for the Multiple Sclerosis Foundation.
“But it is a bit problematic for a few reasons,” continues Dr. Williams.
“It may be difficult to assess bilateral strength simultaneously for subtle differences (without someone else to assist.
“Strength can be mildly asymmetric if there was a previous injury or pain limiting movement (arthritis).
“With that being said, shoulder flexion and hip movement are definitely doable.
“Biceps resistance can be done manually or using a light weight. Wrist flexion may be a bit harder to assess at home.”
ALS Strength Test 1
Shoulder flexion 1. Raise both arms, keeping them straight, at the same time in front of yourself, palms down.
Partner applies resistance atop your forearms. Both arms should resist with equal strength. Exercise equivalent: shoulder frontal raises with dumbbells.

Shoulder flexion. Shutterstock/ruigsantos
ALS Strength Test 2
Shoulder flexion 2. Raise both arms at same time, palms up, arms straight, as if holding large pizza box. Close eyes and count to 10. Palms should remain up.
This sounds easy, but when ALS affects upper body, at least one arm will “drift” such that palm starts turning downward; forearm starts turning inward; and arm then drops.
Exercise equivalent: shoulder frontal dumbbell raises, holding dumbbells with palms facing ceiling.
ALS Strength Test 3
Biceps resistance. Position arm to 90 degree bend, upper arm vertical or almost vertical. Partner presses down on wrist, his hand atop your arm.
You resist by “curling” or bringing hand up towards shoulder.
Ability to do this should be equal in both arms. Exercise equivalent: Biceps curls with dumbbells or a barbell.

Biceps curl. Shutterstock/AXL
ALS Strength Test 4
Triceps resistance. Position arm as though raising a knife to stab someone; hand is about eye level.
Partner presses against your wrist from below it and you resist, pressing forearm downward. Strength should be equal in both arms.
(Keep in mind that it’s not uncommon for one arm to be a LITTLE stronger than the other.) Exercise equivalent: Triceps push-downs.

Triceps push-down
ALS Strength Test 5
Wrist flexion. Hold arm out straight, palm facing ceiling. Partner places his hand below yours and presses upward to bend your wrist. You resist.
Exercise equivalent: Dumbbell or barbell wrist flexion or “curls.”
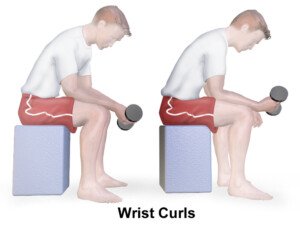
Source: BruceBlaus/CreativeCommona
ALS Strength Test 6
Grip. Partner stands before you. With your arms bent to about 90 degrees, grab partner’s fingers.
But grab only his index and middle fingers; completely grab them.
His arms are bent 90 degrees while you do this. He then tries to removed his fingers from your grip.
He should not be able to do this if you have healthy strength.
However, my own opinion, is that if the partner is strong, he just may be able to remove his fingers. I, personally, don’t believe that it’s a rule that the partner can’t remove his fingers. Exercise equivalent: hand grips.

Hand grip device
ALS Strength Test 7
Hip flexion. Lie on floor, legs straight. Partner presses on one knee while you resist by raising leg.
Partner repeats with other knee. Strength should be equal; you should be able to resist.
Exercise equivalent: ball leg lift, though this requires strength in the core. “Out of shape” people will struggle with this.

Hip flexion. Shutterstock/Motortion Films
ALS Strength Test 8
Hip extension. Lie on floor, legs straight. Partner presses upward against from beneath your thigh (hamstring). Exercise equivalent: Hip extension or “butt” machine; cable.

Hip extension. Shutterstock/vladee
ALS Strength Test 9
Hip adduction. Lie on floor, legs straight. Partner places hands on both inner thighs and tries to spread them out; you resist. Exercise equivalent: hip adduction machine.

Hip adductor or “inner thigh” machine. Shutterstock/The Vine Studios
ALS Strength Test 10
Knee extension. Lie and slightly bend one leg so that partner can support it beneath thigh (hamstring) while placing other hand atop calf.
Extend knee or kick out leg while he resists by pressing down on calf. Exercise equivalent: “leg extension” machine.

Leg/knee extension. Credit: George Stepanek
ALS Strength Test 11
Knee flexion. Same thing except partner places resisting hand beneath calf and tries to keep you from pressing downward. Exercise equivalent: seated leg curl machine.

Leg curl. Credit: George Stepanek
If you do well on these strength tests, you will worry less about ALS.
“It’s fine to do testing at home, but if there is concern, a person should make sure to be seen by a healthcare professional for formal assessment,” says Dr. Williams.