How Much Caffeinated Coffee Is Safe a Day?

What does a doctor have to say about how much caffeinated coffee is safe on a daily basis?
“According to multiple studies, for people in generally good health, up to about 200 mg of caffeine a day is acceptable for most people,” says Marc I. Leavey, MD, a primary care physician with 40-plus years of experience.
Dr. Leavey continues, “With a standard six ounce cup of brewed coffee containing about 100 mg, this would be about two coffee cups daily.
“Remember that coffee cups are six ounces, not eight, so that 12 ounce mug holds two cups.”
Caffeine isn’t the only ingredient in coffee to be aware about.
“Along with the caffeine, there are other substances in coffee which are physiologically active,” says Dr. Leavey.
“Indeed, coffee made with a French Press may have substances which influence serum lipids; filtered coffee removes those substances in the brewing.
“Instant coffee is also lacking those chemicals, and likely is lower in caffeine (for regular instant) than brewed coffee.
“Some studies have suggested there may be toxins in instant coffee, but these are likely at very low levels, ft at all, and may or may not be of clinical significance in typical coffee drinkers.”

Dr. Leavey was formerly with Mercy Medical Center in Baltimore, MD, where his focus was primary care and internal medicine. He has a blog, STRING OF MEDICAL PEARLS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/NOBUHIRO ASADA
Can You RUB Off a Melanoma?

This article is about rubbing off a melanoma, not scraping, picking or cutting.
Ever wonder if melanoma can be literally rubbed off? For instance, with a fingertip, rag or piece of clothing?
“It is not possible to remove a melanoma completely by simply rubbing it with clothing, a rag or a finger,” says Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30+ years’ experience.
But this doesn’t mean you can’t remove some of the melanoma with a rubbing action, especially if it’s big and has raised portions.
It just depends on how hard you rub, the length of time spent doing this (vs. just one swipe with a fingertip or wash cloth) and what the rubbing instrument is (finger vs. sandpaper).
Dr. Prystowsky says that it’s “possible with effort to purposely rub the visible signs of a melanoma off of the skin.
“It would require rubbing that leads to superficial bleeding, however, like a skinned knee from rubbing the rough cement on a sidewalk.”
In short, intense rubbing—with something rough rather than smooth, such as a loofah brush or emery board, as opposed to the smooth surface of your palm or a cotton swab. And it would require repeated swipes.
“Even with this extreme rubbing, it would not mean the melanoma is completely gone, however, because microscopic melanoma cells would remain behind in deeper layers of the skin,” says Dr. Prystowsky.

Melanoma
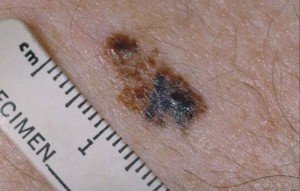
Melanoma

Melanoma. CDC, Carl Washington, MD, Emory Univ. School of Medicine, Mona Saraiya, MD, MPH
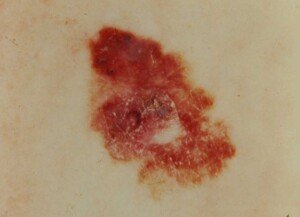
Melanoma. Laurence Meyer, MD/ cancer.gov
There can be micro-metastases, meaning, microscopic branches of the malignant cells extending underneath the visible spot, penetrating into the dermis, which is the second layer of skin.
“Someone rubbing the melanoma would have the mistaken belief that because they cannot see the spot on their skin any longer, that they do not have to worry about it –this is not the case,” explains Dr. Prystowsky.
If you leave even just one tumor cell behind (in theory), that one cell would likely proliferate unseen beneath the visible part of the skin.
“It is worth noting that skin cancer tissue bleeds more readily than normal skin typically, so minor trauma from tight clothing may trigger enough rubbing to disrupt the surface of a skin cancer and cause bleeding.
“This is because cancer cells more readily break away from each other and have a more generous blood supply than normal skin.
“After the bleeding stops, you would expect to see at least some of the skin cancer, e.g., melanoma, remaining under this less traumatic, accidental rubbing situation.”

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/KamranAydinov
Occasional Tender Spot on Head; No Injury
That occasional tender spot on your head can have different causes other than trauma or injury.
“It’s happened to most of us,” begins Marc I. Leavey, MD, a primary care physician with 40-plus years of experience.
“You are brushing your hair or having a shampoo or rest your head back on a chair, and that spot hurts.
“You have someone look at it and they see nothing, but it hurts.
“Could it be a brain tumor? Could it be a stroke? Could it be where the alien probe was? Probably not any of those.”
So what, then, causes a tender spot on your head to come and go if you haven’t been hitting your head?
Dr. Leavey explains, “Lacking a direct cause for a tender spot, such as being hit over the noggin with an object or suffering a fall, the vast majority of these pains are located in the relatively thin layer of skin and muscle that covers the skull.
“Unlike most other areas of your body such as the limbs or your trunk, pressing on the skin of the head directly compresses the tissue into the underlying, unyielding bone of the skull.
“That means that any disruption of the integrity of the skin of the head, no matter how minor, can be magnified in its effect due to this compression.
“Trauma could be so slight as to be unnoticeable to all but detailed inspection, and could be from an insect bite, a scratch from a brush or comb, an inflamed hair follicle, a pimple, or even a reaction to a hair product.
“I have had patients who rested their heads on hard surfaces for a period of time, reading or sleeping; and each awoke with a micro-bruise of the area, a tender spot without any apparent reason.
“Certainly, if you have an area of pain or discomfort, especially one without an apparent cause, you should seek medical attention to be sure that nothing more ominous is causing the problem.
“But be reassured that in the vast majority of such cases, the etiology is minor, the process is self-limiting and the discomfort normally clears in a short while.”
The tender spot on your head, don’t be surprised, feels like the same kind of tenderness you might feel in a specific spot on your shin, where that same pressure phenomenon can occur, since there’s not much “meat” between the skin and the shin bone.

Dr. Leavey was formerly with Mercy Medical Center in Baltimore, MD, where his focus was primary care and internal medicine. He has a blog, STRING OF MEDICAL PEARLS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Safe to Lift Weights through Pain of Tetanus Shot?

Here is what a nurse told me after I asked if lifting weights through tetanus shot pain was safe.
The day after a tetanus shot, my upper arm felt as though someone had slugged me there.
I could not lift it to horizontal — as though doing a side lift with a dumbbell — without pain.
On this day, it did not interfere with my deadlifts, farmer walks or reverse rows.
But I could tell it would be a beast to attempt pushing movements—which I was scheduled to do four days later.
The next day, no change. Rather than see what laypeople are guessing at about this on sites like Yahoo Answers, and not finding this specific information on sites like webmd, I decided to call my medical carrier’s nurse advice line.
“Is it okay to lift weights through the pain of a tetanus shot?”
I left my message with the medical assistant. Shortly after I got a call from the nurse.
She started, “I got your complaint and I laughed. You are so right!” She obviously has received many complaints about pain in the arm from a tetanus shot.
She continued, “It hurts SO bad. I’ve had the same shot myself. It DOES hurt. It’s the medicine working in the arm. The more you move it, the more you’ll work out the medicine.”
The pain is from the vaccine drug working around in there. “It hurts really really bad,” she continued.
But she assured me that movement is the best thing for it, and this includes strength training.
I even said, “So I can go ahead and pick up my dumbbells?” And she gave me the green light.

Shutterstock/Syda Productions
Medical Doctor’s Answer
I then asked a doctor, for the purpose of this article, what her take was on lifting weights despite pain from a tetanus shot.
“Absolutely. In fact, keeping the muscles moving will help the pain,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
However, the green light comes with a precaution. Your arm, due to the tetanus shot, may be weaker, even if you can mentally bully your way through the pain during a weightlifting set.
So start out with lighter weights, particularly with the dumbbell overhead press and dumbbell press.
Gradually work your way up to your working sets with the bench press; so if you normally perform warmups with four different weights, insert a few additional intermediary loads in there.
For best results, don’t do pushing movements or shoulder work within two days of a tetanus shot, as the pain may distract you and result in a sub-par weightlifting session.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/thodonal88
White Flakes In Your Beard: Cancer May Be Cause

If you’ve been seeing white flakes in your beard, cancer must be ruled out.
A dermatologist explains the causes (including cancer) and solutions to white flakes in your beard.
“White flakes in a beard can reflect a dermatitis such as seborrhea (dandruff) or atopic dermatitis (eczema or psoriasis),” begins Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30+ years’ experience.
“These are nuisance conditions that can be readily managed with topical steroids and anti-dandruff shampoos.
“Sometimes prescription strength formulations are required depending upon the severity.
“Most people with an itchy, flaky beard have some form of dandruff, eczema or psoriasis.
“If over the counter anti-dandruff shampoos don’t help, and if topical steroids don’t seem to help either, it may be time to see your dermatologist.”
Infections As Cause of Flakes in One’s Beard
Dr. Prystowsky explains, “Infections of the beard hair follicles can cause white flaking and are more serious.
“If suspected, the skin and beard hair should be cultured to determine whether fungus (dermatophytes) or gram positive bacteria (e.g., staph, strep) or gram negative bacteria (e.g., pseudomonas) may be present.
“Infections of the beard usually are best treated in my experience with oral prescription medication targeted for the particular infectious agent.
“Oral drugs work better than topical agents in the beard because the follicles containing the infection are deep, requiring blood delivery of the drug to clear up the infection.”
Cancer As a Cause of White Flecks in Your Beard
“Finally, precancerous and cancerous growths may produce white flakes, and a biopsy may be required to determine definitive treatment,” says Dr. Prystowsky.
These growths would be originating from the skin: skin cancer.
But who’d ever think that cancer might cause what appears to be dandruff in one’s beard?
But cancer is possible, though not the most likely cause.
“White flaking in the beard that does not respond readily to over the counter remedies should be evaluated by a dermatologist,” says Dr. Prystowsky.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: George Rudy
White Patches on Big Toenail: Causes, Solutions

Find out if cancer is one of the many causes of a white patch on your big toenail.
You may be quite scared that the white patch or multiple white lesions on your big toenail might be some kind of cancer such as melanoma.
There are multiple possible conditions that can cause a white patch to appear on the nail of your big toe.
And here’s some reassurance: Melanoma and other skin cancer are not among those conditions.
Possible Causes
“White patches on the big toenail usually represent a superficial fungus that can be treated with over the counter topical agents such as Lotrimin or Lamisil,” says Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30+ years’ experience.
“Sometimes it can indicate no infection at all and may be nail plate dryness from removing nail polish with solvents,” she continues. “Moisturizing the nail plate with Aquaphor may help.
“Deeper fungal infections may also look like white patches, and a culture is necessary to verify this.
“Finally, trauma to the nail from ill-fitting shoes, or exercise that causes the end of the nail to jam repeatedly against the inside of a sneaker or ski boot can cause the nail to separate from the nail bed and make it appear whitish.”

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Andrey_Popov
Small Circles of Peeling Skin On Fingertips: Doctor Explains
There are three causes, says a dermatologist, of small circles of peeling skin on the fingertips.
That’s a pretty odd-looking symptom, but here is what Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30+ years’ experience, explains:
“Small patches of peeling skin on the fingertips is typically psoriasis; a contact reaction to a substance that you may be allergic or sensitive to; or may reflect recovery from a systemic viral illness.”
So to treat this symptom, you must find out what the cause is. A doctor can determine if the cause is psoriasis.
If it’s determined that this autoimmune disease is not responsible for circular peeling areas of skin on your fingertips, then you’ll need to evaluate whether or not you’ve been touching things or getting substances on your fingertips that might be triggering an allergic reaction.
Of course, if you’ve recently had a systemic (body-wide) viral illness, you will have felt sick enough to know this — or at least, that some kind of “bug” was in your body.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Half of Mole Suddenly Falls Off, Bleeds

Has half or part of one of your moles suddenly fallen off and has bled?
Are you afraid this is melanoma?
“When half of a ‘mole’ suddenly falls off and bleeds, it usually is not a mole but a benign seborrheic keratosis that has caught on some undergarments,” says Dr. Janet Prystowsky, a board certified dermatologist in New York, NY, with 30+ years of experience.
A seborrheic keratosis is a skin barnacle and it is benign.
These skin growths typically begin appearing after age 40 and will NOT turn into melanoma.
However, keep in mind that these harmless barnacles may look very much like a mole — especially if it’s in a difficult-to-inspect location such as your butt or back, not enabling you to get a close view.

Seborrheic keratoses mixed with moles. Shutterstock/NICKY1841
They may even resemble melanoma and can suddenly change in their appearance.
For example, they may get noticeably lighter in a matter of only days.
This is harmless as long as what you see changing is only the seborrheic keratosis.
However, if you notice that a diagnosed seborrheic keratosis is changing in appearance or especially bleeding, have it checked by a dermatologist because, by sheer coincidence, it is possible for a melanoma to start up on the same skin surface area as this harmless barnacle.
Keep in mind that a seborrheic keratosis does NOT cause or trigger the melanoma that by chance just happened to arise within it.
The presence of these skin barnacles does not prevent melanoma from taking over the space.
Another situation that may appear as part or half of a mole tearing off and then some bleeding, is that of the common skin tag.
“Sometimes a benign skin tag will twist on its stalk and may completely or partially fall off,” says Dr. Prystowsky.
“However, if a true mole (nevus) begins bleeding (whether or not part of it falls off), it could represent a melanoma — a serious and potentially fatal type of skin cancer.
“Other forms of skin cancer, such as a pigmented basal cell carcinoma, may bleed and resemble the appearance of melanoma.
“A professional opinion from a dermatologist should be sought for any growth that starts bleeding, especially if you have no recollection of it being traumatized.”
Areas to Check for Moles
Moles can turn up anywhere where there is skin.
When conducting self-exams of your skin, be sure to check the following areas: behind your ears, the earlobes, inside your ears, the eyelids, the lips, your belly button, between your fingers and toes, and the soles of your feet.
The skin of the genital area should also be checked.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE certified personal trainer.
Top image credit: Shutterstock/IanRedding
Muscle Twitching vs. Spasms: the Difference?

A neurologist explains the difference between twitching muscles and a spasm.
These two terms are often used interchangeably among laypeople either posting their concerns in forums, or journalists who indiscriminately toss around these two terms.
To get the distinction between muscle twitching and a spasm (of skeletal muscle), I asked Bonnie Gerecke, MD, director of the Neurology Center at Mercy in Baltimore.
“Muscle twitching refers to a small muscle contraction in the body,” says Dr. Gerecke.
“This usually entails twitching of some muscle fibers of a muscle and not necessarily the entire large muscle itself.” The entire large muscle itself is called the belly.
An example of a twitching muscle is that which commonly occurs in the eyelid. Another common area is the hamstring group.
You’ll feel the fluttering or “creepy crawlie” under the skin in a very localized spot.
If the twitch occurs in a very small muscle, such as the eyelid or pinky toe, you’ll see the jerking or jumping of the involved muscle fibers.
But that’s because the affected fibers are part of such a tiny muscle to begin with.
“Muscle spasm refers to a spontaneous abnormal contraction of a whole muscle,” continues Dr. Gerecke.
An example is when a leg jerks as you’re falling asleep (myoclonus). This is a perfectly normal phenomenon.
“A twitch is a brief phenomenon that affects a small portion of a muscle, whereas a spasm may be more prolonged and affects a large muscle group.
“A twitch does not tend to be painful, but a spasm can be quite painful.”
Myoclonus is painless, but the other kind of spasm that Dr. Gerecke refers to is, indeed, intensely painful.
For instance, you’re just awakening from a night’s sleep and without really thinking, you stretch your body, straightening and tensing up your legs — when suddenly, your calf muscle goes into a spasm.
The pain is agonizing. To relax the muscle, bend the foot upward. Massage will also help.
You may also notice sudden pain in your neck and jaw area upon doing a big yawn.
The involved muscles are going into a spasm, and it hurts quite a bit, but subsides very soon.
Even smaller muscles can go into a benign spasm, such as those in your big toe. It hurts, but quickly subsides.
Non-skeletal muscle can also spasm, such as the uterus (menstrual cramps) and the esophagus (which can make someone think they’re having a heart attack).
You now know the difference between a muscle twitch and a spasm.

Dr. Gerecke has a special interest in ALS, myasthenia gravis, myopathy/muscular dystrophy, peripheral neuropathy and radiculopathy. She is board certified in general neurology and neuromuscular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Joyseulay
Is Tongue Twitching Normal if You Stick It Out to Inspect?

A neurologist explains if it’s normal for a tongue to twitch when you hold it out to examine it due to bulbar ALS fear.
People with a fear of bulbar onset ALS will stick their tongue out and hold it in one spot to see if it twitches.
It’s difficult to hold the tongue perfectly still, so invariably, it moves, and you may incorrectly interpret these movements as fasciculations with a pathological cause.
“It is not necessarily pathological for one to experience twitching in the tongue when protruding it,” says Bonnie Gerecke, MD, director of the Neurology Center at Mercy in Baltimore.
“Twitching can be due to a variety of conditions such as anxiety, hyperthyroidism, hypoglycemia (low blood sugar) and even in normal individuals,” explains Dr. Gerecke.
“Fasciculations, which are different than just twitching of the tongue, is often more pathological, but is rare and is often not seen in isolation in patients with ALS.
“That is to say that if there are fasciculations in the tongue of a patient with ALS, he or she also will likely have dysarthria (slurred speech) and perhaps trouble chewing or swallowing.”
Stop sticking out your tongue to inspect it for twitching.
Give this a rest. Enjoy your food and talking. If there’s difficulty swallowing, chewing or speaking as a result of bulbar ALS, even early ALS, you will know this without having to consciously try to detect it.
Think about that for a moment: Difficulty swallowing, chewing or speaking without slurring are symptoms that are impossible to miss!
You do not need to constantly be inspecting your tongue, subjecting this muscle to the tiring act of holding one position.
For additional reassurance, ask all of your friends to stick out their tongue and try to hold it still without it “twitching.”

Freepik.com/asierromero
If you’re reluctant to make this request of adults, ask children; disguise the request as a game.
Have a stopwatch and ask the child to see if they could stick out their tongue and hold it there for 20 seconds without it moving.
You will see the same “twitching” in this experiment as you do with your own tongue.

Dr. Gerecke has a special interest in ALS, myasthenia gravis, myopathy/muscular dystrophy, peripheral neuropathy and radiculopathy. She is board certified in general neurology and neuromuscular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.