Do Hardbodies Really Stare at Fat People in the Gym?

Is it reality or myth that in a gym, the hardbodies stare and gawk at fat people?
You’d think a gym would be crowded with very overweight people, but just the opposite is true.
Many overweight people believe that they’d be stared at, even snickered at, by the buff bodied patrons at a health club.
It’s true that the overweight jogger is bound to get heckled outdoors by motorists. But I’m talking about GYMS.
A gym, actually, is a sanctuary for overweight people, even the obese. The truly fat man or woman just doesn’t realize what a sanctuary a gym could be.
If you are obese and experience rudeness in public, the gym is one place where this will be nearly nonexistent.
Do not stereotype the “hardbodies” as being the rude type who’d snicker and stare.

Shutterstock/RomarioIen
I’ve watched TV shows, talk shows and news shows in which overweight people are explaining their fear of being openly stared at or ridiculed at a gym.
I’ve also read such points of view by overweight people in print media.
Now I’m not saying there aren’t isolated cases in which an overweight person was treated poorly by gym personnel, or treated rudely by another patron.
But these are isolated situations. Even a buff person can be treated like crap by a jerk. That’s life: Some people are just plain jerks.
I have witnessed very obese women and men walking towards the locker room in a crowded gym.
Actually, my eyes were more on nearby gym goers to see if, indeed, there was any truth to this idea that very big people at a gym get gawked at.
I have YET to witness just ONE person staring bug-eyed at an obese man or woman. I’m sure it’s happened, but behind the person’s back, I’m sure.
In fact, it’s expected that a nearby person’s eyes will nonchalantly follow a 300 pound person as they head towards the locker room.
If a 250-pounder in shorts is on the treadmill in the row of cardio equipment ahead of you, you’re certainly bound to stare a little.
And guess what: The anorexic-looking women get stared at, too.
In fact, there’s always lots of staring at a gym.
- The woman whose arms are completely covered in tattoos gets a lot of staring.
- The 5-2 woman who’s built like a bar bouncer as she trains for her bodybuilding competition also gets her share of gawking, stares and whispers.
- So does the man who grunts loud enough during weightlifting for the whole gym to hear
- And so does the woman whose spinal column is jutting out because she weighs 79 pounds.
But I have never, ever, ever caught wind of any ridicule or snickering directed towards fat people. Why would someone ridicule you for working out?
If you’ve been ridiculed at Dairy Queen as you walk out with an ice cream cone, this doesn’t mean you’d be made fun of at the gym.
If you’ve been heckled by a car load of teens at the grocery store parking lot, this doesn’t mean that you’d get taunted at the gym.
The gym is your escape from a mean world.
Everyone at a gym is so caught up with their OWN bodies, they’ll hardly notice yours.
Do not avoid the gym before you go there and see what it’s really like.
I swear, people on the cardio equipment are either in a trance, or, their eyes are glued to the TV screens, or, they’re yakking to each other on side-by-side machines or into their cell phones. They won’t even notice you.
As for the weightlifting equipment, again, have a seat on some exercise equipment.
Any hardbodies nearby will be too busy cranking out their routine, or too busy recovering from it, or too busy checking out their own bodies, to take interest in yours.
It’s a myth that hardbodies stare at “fat” people at the gym.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Lebedev Roman Olegovich
Speed Up Fat Loss with Anaerobic Cycling: Lose Belly & Leg Fat

Never underestimate the power of stationary bike workouts for melting off excess fat in your stomach, thighs or anywhere else — as long as you do it anaerobically.
Because pedaling a stationary bike is so easy, requiring no impact and no balance, you may think that it’s impossible to perform a wickedly punishing routine on this simple piece of exercise equipment.
Don’t let the simplicity of the stationary bike fool you; this tool is a potent weapon in the war on stubborn body fat.
Pedaling the bike in the “aerobic zone” has its limitations; namely, you won’t burn as much fat as you will if pedaling in the anaerobic zone (also referred to as the “cardio” or “athletic training” zone on some machines’ consoles).
Traditionally, the stationary bike has proven very useful for a comfortable, inviting warm-up for a grueling weight workout, or a hard-paced run on the treadmill. It’s also popular for warm-downs.
But don’t stop there. Include the stationary bike as a tool for igniting fat loss.

©Lorra Garrick
Take a break from the treadmill, elliptical or outdoor running. Shock your body with something different for a change.
A shocked body will use up more stored fat to deal with the shock—the shock of something entirely new that it is not acquainted with.
The anaerobic threshold varies from one person to the next. This is that point at which your body’s energy system shifts gears: from aerobic to anaerobic.
The more fit you are, the higher will be your anaerobic threshold. You must find out where yours is with cycling.
This is done as follows: Picture a number scale: 1 is how you feel when lying on a hammock, and 10 is how you’d feel if you just tried to outrun a train.
For ultimate fat loss, you want an exertion output that makes you feel at level 9-10. Because this is very near or at maximal intensity, it cannot be sustained for very long.
In other words, how hard must you pedal a stationary bike before you’re ready to fall off of it after only 20 or 30 seconds?
It’s easy to think you’re ready to fall off the bike if you’ve been pedaling with gusto for 20 minutes nonstop.
But when I say “ready to fall off,” I mean it: You’re so spent that you cannot pedal one revolution past 20-30 seconds.
Your thighs are wasted. You can’t talk.
The settings to achieve this kind of exertion, depending on your cardio fitness level, might be a level 12 on a bike that goes up to 12 “levels,” which indicate resistance of pedal crank.
This is a sturdy pedal resistance, but it must be combined with high RPMs to completely tax you in under half a minute. The RPMs in this case might be 100—sustained for an entire 30 seconds.
Try it. If you can go beyond 30 seconds, then after two minutes of easy pedaling at very light resistance (level 1-3), see if you can sustain an RPM of 130 at level 12.
Keep searching for that RPM speed that, if carried out at level 12, leaves you with no energy to go beyond half a minute.
Now, some bikes have up to 20 levels. In that case, a level 12 on these bikes is easier than a level 12 on a bike that has only 12 levels. There are many makes and models of stationary bikes out there.
For many people, it will be impossible to pedal 100 RPMs at level 18 on some models.
Don’t get confused by all these numbers here; focus more on the concept:
At at least 100 RPMs, figure out the pedal resistance (“level,” which is usually indicated by an “L” on the bike’s console), that turns you to toast within 30 seconds.
If you’re pedaling longer than 30 seconds, you begin going into a pacing mode.
This workout’s brief bursts of high-powered pedaling are supposed to be “sprints,” to maximize fat-burning.
They alternate with two minutes of lenient, gentle pedaling (70 RPMs at very light pedal resistance).
- Warm up for 10 minutes with easy pedaling progressing to moderate pedaling.
- Then begin this high intensity interval training by introducing your first 30-second interval—but make it a perceived exertion of 7 or 8 on that 1-10 scale mentioned prior.
- The next interval can be an 8.
- Make the next a 9.
- After that, you are warmed up for all-out sprints on the stationary bike.
Don’t get caught up with counting how many sprint intervals you do. Instead, when the time lapse hits 40-45 minutes, start winding down by pedaling at medium intensity for several minutes, and then light pedaling for a few more minutes.
50 Minutes Tops
The entire time you’re on the bike, including warm-up and warm-down, should not exceed 50 minutes.
This kind of anaerobic cycling can be done twice per week when you are trying to cut up or really thin out your body fat layer, while hanging onto mass.
A third cardio session per week should be done at low intensity and for long duration.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
Broad Shoulders in Women: Solutions?

Are you a woman who hates her broad shoulders?
Perhaps you’ve been wondering if there are ways to shrink the size of your broad shoulders.
If you hate your broad shoulders because you’re a woman, then there’s only one thing that I, as a personal trainer, can think of as a solution, and it’s a solution that can actually work:
Embrace your broad shoulders.
That’s all a woman who hates her broad shoulders can do, and here’s why.
I once read a thread in a fitness forum started by a woman who despised her broad shoulders.
She sounded like she was in serious trouble, because although her initial post seemed to be no more than asking fitness enthusiasts if there were exercises to reduce her shoulder size, she made more posts that were increasingly disturbing.
In summary, this woman’s life was bleak and bitter, and she blamed this on her broad shoulders. Does this sound like body dysmorphia to you?
In the thread, none of the fitness enthusiasts, who included personal trainers, offered any exercises that could lessen the dimensions — because none exist.
But there was a recurring theme coming from the men who responded: Broad shoulders on a woman are sexy.

Shutterstock/RomarioIen
One guy pointed out that it’s a mystery where women get their ideas of what a man would find attractive or not attractive, that they probably get their ideas from other women.
He continued that they should not pay attention to what other women find physically appealing in each other.
Instead, he pointed out that they should pay attention to what MEN find appealing in women.
The one man also posted that it would be ridiculous for him to worry what other MEN thought was appealing on a man’s body, since he was attracted only to the opposite gender.
Likewise, if you’re a woman worried that men might be intimidated or turned off by your broad shoulders, where is this idea coming from — men, or your own gender ??

Freepik.com, Racool_studio
Your perspective should be based more on what men find inviting, not from what members of your own gender find attractive. Many men simply do not go for the small, petite, “weak” look.
Remember the shoulder pad craze of the ‘80’s?
There was a reason for that. Watch TV shows filmed in the ‘80’s and note how many actresses have shoulder pads.
You might even spot shoulder pads being worn by movie starlets in 1940’s films.
There are no solutions for you if you’re a woman who hates having broad shoulders, other than to accept them — because you cannot change them if they’re natural.
All I can suggest is that you exercise your entire body to make it as fit and strong as possible, to distract you from obsessing about something that you cannot change.
And before you dismiss me as someone who cannot possibly understand your predicament, I’d like to point out that I proudly sport broad shoulders.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
Cause of Child’s Skin Picking: OCD or Bad Parenting?

Here’s an answer to if the cause of a child’s skin picking is OCD or bad parenting.
What mother would ever blame herself for her child’s skin picking?
Does your child pick at his or her skin? Is OCD (obsessive compulsive disorder) or bad parenting the cause?
- Coming up with a conclusive answer could be challenging.
- However, is it logical to exclude parenting style from the equation?
When I saw my niece for the first time when she was 15, I inquired about what appeared to be cigarette burns up and down her arms. She said she picked her skin.
Her mother, a doctor whose practice at that time focused on treating people with ADHD and OCD, thought that the girl picked her skin as a result of some genetic wiring flaw in the brain.
Her mother is my sister. Just to give a little context: My sister does not have a medical board certification, and never did, in a specialty related to ADHD or OCD.
In fact, she’s never been board certified in any medical specialty.
Her residency, though, was in pediatrics, and after giving up on passing any Boards, she opened a private pediatric practice.
Eventually she turned to focusing on ADHD, OCD and even addiction, having taken certification courses in these areas, as well as acquiring certification in social work.
With all that said, it’s easier to imagine a child skin picking as a result of being henpecked day and night by a bullying mother, as opposed to being caused by a genetic disorder.
This girl’s parents also had begun divorce proceedings when she was 13, and it was ugly.
I want to interject here that in 2022 I was diagnosed with autism, and since then, have learned that skin picking is more common among autistic people than in neurotypical people.
However, this doesn’t mean that we should look at autism as a possible cause of my niece’s skin picking.
When I look back at her overall behavior, I realize that absolutely there were no signs that were suspicious for autism.
I also don’t see any point in considering the possibility that she concealed any autism via “masking.” But even if she had — this in no way dilutes the hardcore fact that her mother was emotionally abusive.
Furthermore, “more common in autism than in neurotypicals” does NOT translate to “common in autism.”
Neurodivergence aside, let’s imagine hearing from your mother, from the moment you get up in the morning, till it’s time for bed, everything you did wrong that day. Day after day.
That was my niece’s world when she was growing up.
Her mother continuously took slings at her. It was no wonder the girl became a skin picker.
Skin picking, like an eating disorder, is a response to feeling out of control and full of shortcomings, according to skinpick.com.
My niece had been on the receiving end of frequent denigrating remarks from her mother for years – confirmed by my cousin who’d had regular contact with them over the years.
When my sister and her kids were visiting my parents, an hour couldn’t go by without my sister harping on her oldest daughter for no good reason.
An example was when her mother went on a tirade because Emma was searching wastebaskets for a coupon that she believed she had accidentally thrown out.
Like, what is so abnormal and deserving of insults about searching for a coupon in a waste can? What level-headed adult has never done this?
“Emma takes long at everything,” her mother snidely declared, after the girl innocently commented to me that she eats slowly.
The girl had a brooding and glum, rather than neurodivergent, presentation.
Emma was on three drugs (prescribed by her mother) including Risperdal, whose main label use is for schizophrenia, says Risperdal.com.
However, my niece was not schizophrenic or psychotic. She took this drug for OCD: obsessive compulsive disorder.
A child would have to be superhuman not to exhibit maladaptive behaviors as as result of being raised by a bully.
Though my sister didn’t believe in corporal punishment, she definitely hurled words like rocks.
And sometimes, it wasn’t about words, but about behavior.
During their visit, I, my sister, her three kids and my brother went on an easy hike.
My niece complained of a headache at some point. It was very hot, and though she had a trim figure, she was out of shape because she didn’t exercise or play sports.
Her mother suggested she shake water from her water bottle onto her arms to cool off. So far, this sounds like a reasonable suggestion. But — there’s more to it.
Since it was hot out, the water in the bottle was warm; not very pleasant to drink.
Emma casually declined the suggestion to sprinkle it on her arms.
You’d think it would have ended there. But for about 10 minutes, my sister kept demanding that the teen sprinkle water on her arms to “cool off.”
I do not know how sprinkling warm water on one’s arms will cool someone off. Do you?
My sister wouldn’t let this go and turned it into a full-blown power struggle.
Finally, she grabbed her daughter’s bottle and began shaking it at her, droplets flying everywhere, and the distressed girl kept dodging the droplets, literally being chased by her mother.
This was no silly game of tag. Nobody was even grinning. This was clearly a bullying scenario. No wonder the girl picked at her skin.
Skinpick.com even says that a prominent reason a child begins skin picking is in response to being bullied by a parent!
I don’t have a PhD in child psychology, but I have eyes and ears.
This girl was a good kid in that she got good grades and was quite skilled with her favorite musical instrument. Her goal was to either be an English teacher or crime scene investigator.
She grew up to get a college degree in English and work at a bank. I’ve had no contact with her other than when she was 15, and then again at 18.
As of 2023 she’s 28. I have no idea if she ever ceased picking at her skin. However, she has many tattoos.
Skinpick.com explains that the definitive cause of skin picking is the subject of research, but a leading explanation is that a child feels she has no control in her world – except that which is very much within reach: her skin.
So she picked her skin, creating some order in a chaotic world by controlling this one feature. Skin picking symbolizes an active control.
The markings were obvious and plentiful. I’m not talking about just two or three on one arm.
I just cannot believe for a second that this child would have developed skin picking regardless of what kind of parent-child dynamics were going on.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: skinpick.com/skin-picking-causes
Top image: ©Lorra Garrick
Have Plus Size People Really Tried Everything to Lose Weight?

This article explains why “I’ve tried everything to lose weight” is a myth, and what obese or overweight people CAN do for permanent fat loss without surgery.
“‘I’ve tried everything, but nothing works,’ is a common statement that I hear, over and over again in my clinic,” says Richard Kelley, MD, a practicing physician in Texas for 20+ years, and author of “The Fitness Response,” “The Three-Hour Appetite” and the ebook, “The Fitness Response ‘Diet’ for Women.”
Dr. Kelley adds, “For almost all of these clients and patients, nothing could be further from the truth.”
This article was inspired by the countless times that I have seen obese people on talk shows telling the hosts, “I’ve tried everything to lose weight.”
And certainly, physicians of many different specialties have heard these very words as well, numerous times.
Dr. Kelley continues, “Robert Kiyosaki is fond of saying, ‘Excuses are just lies that we tell ourselves.’ In reality, most people know deep-down, that they have not tried everything.”
Look around at your health club. Not only are few patrons actually obese, but you’ll notice other things:
1) It’s quite uncommon to see obese to moderately heavy men and women in the gym’s free weight section
2) And if they are, you won’t see them performing the killer calorie burn routines, and
3) Though many of a club’s overweight patrons are mostly on cardio machines, they’re all doing steady state rather than HIIT.
HIIT is the rocket fuel of cardio.
“In reality, in almost any circumstance and for almost every problem, there are alternative solutions to consider, even when we believe we’ve run out of options,” says Dr. Kelley.
He adds that the majority of his patients who DO exercise, confine it only to aerobics.
Aerobics-only exercise does not equate to significant weight loss.
“Researchers will point to the fact that there is not a strong tie between exercise and weight loss, but again, their data is based by and large, on aerobic-only activity and research that tends to test in the realm of aerobic-only data,” explains Dr. Kelley.
“This is a bias which may not even be recognized by many researchers and investigators, who may believe that ‘exercise is exercise,’ and it must all be equal in its ability to burn calories.”
Magic Bullet for Weight Loss for the Obese
Research showing the power that strength training yields for weight loss is relatively new.

Shutterstock/Travelerpix
But this power is no secret to physique athletes and bodybuilders. A “bodybuilder” is anybody who seeks to build muscle, and these enthusiasts do not necessarily bulge with veiny muscle. Bodybuilding or physique development is on a continuum.
“I encourage almost every patient I see, who can do so safely, to consider beginning a resistance training program, to help them bridge the gap between the limited number of calories that most of us can burn through aerobic-only exercise, and to help them transition to a physiology capable of burning calories more consistently, 24/7.”
What Dr. Kelley means is that a serious strength training regimen will create a substantial increase in resting metabolism, something that Zumba, dance aerobics, and steady state sessions on cardio equipment will never produce.
This is why men and women who seriously train with weights, and eat sensibly, have such small, tight waistlines.
If you’re obese and think you’ve tried everything to lose weight, ask yourself if you’ve tried heavy weightlifting for six months.
If you’re obese and believe you’ve tried everything to lose weight, have you tried deadlifts, leg presses and bench presses?
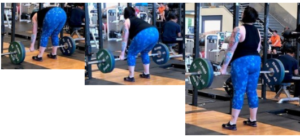
Deadlift Sequence

Leg Press
If you’re obese and believe you’ve tried everything for weight loss, ask yourself if you’ve tried HIIT: high intensity interval training.
If you’re obese and think you’ve tried everything but also believe you’re too large to do HIIT or intense strength training, you are mistaken. HIIT can be done by the obese.
Obese people are on an even playing field with thin people when it comes to strength training.
Next time you open your mouth to say, “I’ve tried everything to lose weight,” first ask yourself, “Am I sure?”
Chances are extremely high that you have never employed high intensity interval training — a proven way to crush fat.
 Richard Kelley, MD, is an author, speaker, fitness expert and transformation coach.
Richard Kelley, MD, is an author, speaker, fitness expert and transformation coach.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dmitri Ma
Do’s and Don’ts if Your Child Is the Youngest in the Grade

If your child is the youngest in the class and especially entire grade, you’ll want to make sure that you don’t make the following mistakes.
I started first grade at age five, and I have some great advice for you.
Do’s and Don’t’s for Parents Whose Child Is Younger than Everyone Else in the Class
If he or she complains that classmates are reaching various milestones sooner, explain that the milestones will come to your child at the same rate whether he’s with kids his age or a year older.
Don’t ever make a big deal about the age difference, but if the issue surfaces, open up the lines of communication and listen.
Never, ever tell your child that she’s “emotionally behind” or “not as mature” as her classmates.
When I was in seventh grade (age 11), I was the only girl who remained sitting calmly at my desk in homeroom when a bee flew into the room.
All the girls (12 years old, maybe a few 13’ers) fled the room shrieking. The boys stayed behind.
I went to a new high school for grades 11 and 12. It was small and had only one restroom (with several stalls). Between class changes it was always filled with girls – older than me – smoking.
Stinking up the restroom with smoke, knowing full-well it was against school rules to smoke in the building, is a sign of immaturity and blatant disregard for nonsmokers who’d like to use the facility without gagging on the stench of ashes (the restroom wasn’t regularly cleaned).
I never smoked or drank. Older kids did. I never got into trouble. Older kids did. I never stuck gum under desks. And I’d witness older kids cry over things that didn’t phase me.
Was I perfect? No. Once I threw a paper airplane and it hit the teacher in her eye, knocking out her contact lens.
I had no idea the plane would veer that way. I looked away and played innocent, and the teacher never found out where the plane had come from.
Yes, I had my occasional moments, but overall, I was a very low-maintenance, chilled-out kid who began babysitting at age 11.
But believe it or not, I heard more than once from family members that I was “emotionally behind” my classmates because I was younger!
If you don’t want a resentful kid, never tell them they’re less mature than their classmates just because they’re the youngest.
And don’t tell other people that your child is less mature than their classmates, either.

Maturity Level Doesn’t Always Correspond to Being the Youngest in the Class
The most disruptive kids in any class I’d ever been in were not the younger ones.
How Do You Define “Maturity”?
An 11-year-old girl may still be drawn to “The American Doll” or scampering around with her seven- and eight-year-old neighbors, while her 12- and 13-year-old female classmates are more interested in fashion, boys and babysitting jobs.
But this doesn’t mean she’s less mature than they are.
Who’s to say that in a school bus accident, this 11-year-old wouldn’t be the first to go around seeing if anyone was hurt, while the older girls were hysterical and immobile, despite having no injuries?
When I was 13 and a freshman at an all-girls Catholic high school, some older boys from an all-boys Catholic high school entered the building between classes and released a decapitated chicken.
The bird crazily ran all over the place (neurological reflex), dripping blood everywhere.
When the bell rang for the next period and girls filled the hall, they screamed and chaotically dispersed in all directions—girls who were older than me.
I remained calm and simply made sure that the bird didn’t come near me.
Another incident at this school, when I was 13, involved the nun who was in charge of directing school musicals.
The cast performed poorly for the first evening’s production, and we were ordered to sit in the gym’s bleachers afterward.
The nun stood across the gym and began hollering at us, spouting ugly things.
She was so aggressive that the principal had to stand behind her, hands on her upper arms to restrain her.
After her tirade we were released to the dressing room. A 12th grade girl who towered over me was very shaken up and sobbing, exclaiming to me (because I was the nearest to her), “Did you hear what she said?! Did you hear what she said?!”
This girl, prior to all of this, had always come across as thick-skinned, rough around the edges, the kind who wouldn’t take any guff from another classmate.
Yet here she was, unraveled and in tears. And me? I wasn’t the least bit shaken up by the crazed nun’s temper tantrum. Instead, I hated the nun even more.
If your child is one of the youngest in his or her grade, don’t sweat it and never use it as an excuse for anything.
When Your Child Is the Youngest in the Class in Elementary School

“In my experience this is really only an issue in elementary school when a year can make a huge difference in developmental and emotional maturity,” says Dr. Tia Kern-Butler, a licensed psychologist for over 20 years who treats a broad range of issues including relationship problems and behavioral issues of children and adolescents.
“Yes, a parent should never tell a child that they’re emotionally behind, nor should they really compare the child in any negative way to their peers.
“If a child is struggling with this issue there must be a particular reason why they’re feeling out of place (perhaps they can’t do something the other children can, or another child is calling them a baby, etc.).
“A parent should try to talk to their child about what is going on and how they feel about it first, before jumping to conclusions or giving any opinion on it themselves.
“Often a child’s perspective on a situation is much different, and the parent can get a better idea of how to respond when they know how the child is perceiving it.
“If a child feels out of place because of skill differences, the parent should focus on the fact that all people are different and have different strengths.”
The parent should also remind the child that he or she will grow into the skill-set that older classmates have.
Maybe you can also say, “No matter what your age, you will always be a year younger than someone, and someone will always be a year younger than you.”
Dr. Kern-Butler also advises that the parent help develop their son or daughter’s unique strengths.
“They can also discuss that skills are learned and can be improved with practice and identify some ways to help their child do this,” says Dr. Kern-Butler.
 Currently in private practice Dr. Kern-Butler spent 10 years as the lead child and adolescent psychologist with Winter Haven Hospital and served as the mental health liaison for the Children’s Advocacy Center for 14 years.
Currently in private practice Dr. Kern-Butler spent 10 years as the lead child and adolescent psychologist with Winter Haven Hospital and served as the mental health liaison for the Children’s Advocacy Center for 14 years.
Professionalpsychologyofpinellas.com/about-me
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, peoplecreations
Dropping Weights at the Gym & Getting Injured

Dropping weights at the gym is almost always done intentionally, and it’s no surprise that sooner or later, the men who do this get injured.
The whole idea of dropping weights at the gym needs to be changed.
After all, if you’re strong enough to do sets with a particular weight, you should be strong enough to set the weight down without forcefully dropping or “throwing” it.
The exceptions would be a one-rep max deadlift and farmer walks with the heaviest dumbbells possible, but almost always, the dropping appears to be done electively rather than from the inability to handle the weight.
Injuries from Dropped Weights at the Gym
Dropped weights at the gym cause far more injuries than you think, says a new study carried out by the Center for Injury Research and Policy of The Research Institute at Nationwide Children’s Hospital.
The study tracked weight training injuries between 1990 and 2007: over 970,000 overall ER cases in the U.S. during that time.
The most common way that injury occurred in the gym was from weights dropping on someone: 65 percent of the reported injuries.
Overall, 90 percent of the injuries occurred with free weights (which explains why so many injuries were from dropped weights).
I see men carelessly dropping dumbbells and plates to the floor all the time – but a lot of times, it’s the plates that are being dropped — sometimes tossed to the floor or carelessly dropped vertically into slots.
And when men do this, occasionally they miss. But I’ve never witnessed an accident.
As for dropping or “throwing” dumbbells to the floor after chest presses, the user isn’t at risk for a dropped-weight injury; someone nearby is — their feet.
However, I do not know if this specific mechanism of insult was reported in the study. “Dropped weights” can mean different scenarios.
It can mean a dropped barbell on someone’s chest. It can mean a dropped dumbbell on someone’s foot after he doesn’t quite place it in the rack.
Plates can slide off crooked barbells and easily land on someone’s foot.
The age bracket in which the highest proportion of injuries from dropped weights occurred, was12 years and younger. Kids are dropping weights left and right, apparently.
What about mishaps from resistance machines?
What age group had the most injuries from machines? People 55 and over. This isn’t surprising because these machines attract the older crowd more than the younger crowd.
Also, whenever I see someone incorrectly using a machine, it’s almost always an older man – particularly the preacher curl machine. What is it with men 50-plus and the preacher curl machine?
Ever see an old-timer use this machine? Cheat City, USA – which translates to injury risk.
The lat pull-down is another machine that older men improperly use, putting themselves at risk for back and rotator cuff injury.
“Before beginning a weight training program, it is important that people of all ages consult with a health professional, such as a doctor or athletic trainer, to create a safe training program based on their age and capabilities,” explains study author Dawn Comstock, PhD.
This report may make it sound as though pumping iron is a dangerous pursuit, but lifting actually ranks relatively low as far as injuries, when compared to other physical activities.
Weights being dropped is something that’s within people’s control, far more preventable than, say, a sprained ankle while playing basketball.
Also keep in mind that the report included children.
Kids should not handle strength training equipment without supervision, and I wonder how many of these injured kids were not supervised.
So with all of that said, it would be a smart move to work on limiting how often you let the weights drop during your gym workouts.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2010/03/100330115925.htm
Why It’s Insulting to Say “Don’t Worry About It”

Before you tell someone, “Don’t worry about it,” DON’T!
In fact, don’t even say “Don’t worry.” Just these two words alone are a mistake to tell someone, even if they are visibly worrying.
It’s just plain inappropriate to tell someone, “Don’t worry.” If you’re in the habit of doing this, ask yourself the following questions:
“Whenever I tell someone, ‘Don’t worry about it,’ do I have a solution to their problem?”
“Whenever I’ve told a person, ‘Don’t worry,’ did they suddenly brighten up?”
You know the answer is NO to both questions. People don’t want to be told not to worry.
They want solutions to the problem that’s making them upset or concerned.
Invalidating their emotions by telling them don’t worry will not make the problem go away—and they know that. And YOU know that.
Psychology 101 is that the listener makes this lame directive because they don’t know what else to say.
They lack solutions and good advice. Their minds are a blank, so to fill the empty air space, they say “don’t worry.”
And then they have nothing to back up this directive, such as a solution, recommendation or other fix to the problem.
I never tell people not to worry.
Instead, I jump right into offering helpful advice. There is always some way to give help to a fretting person, even if it’s to suggest keywords to google to see what possible information comes up that they can benefit from.
Another peeve is when the individual says, “Don’t worry about it,” in a demeaning or irate tone.
This really puts me on the defensive and makes me feel I must clarify why I’m “worrying” about something.
Another problem with this absurd directive is that many times, it’s an erroneous observation.
I can’t begin to tell you how many times I’ve been told don’t worry when in fact, I wasn’t the least bit vexed.
When this happens, I always call that person out on their wrong assumption, their inability to read someone.
One day I called out my brother on this. I was merely making some comments about the fact that our three-year-old nephew still was not talking.
I was not troubled about this; honestly. At the time, I’d met the nephew only twice in my life and was not in contact with his parents, but my parents were.
So after my casual comment, my brother gruffly stated, “Oh don’t worry about it!”
That set me off. I chastised him for making this wrong assumption. Now you may call me neurotic or overreactive, but I firmly believe that when a person commits a faux pas, they should be called on it.
If my brother, in fact, had been the one to begin commenting about the nephew not talking yet at age three, I would have joined in on the topic and added to it, rather than shutting him down with an irate “Oh don’t worry about it!”
“When someone tells you, ‘Don’t worry about it,’ or, ‘It’s not that bad,’ or anything along the lines of suggesting you are overreacting, that does nothing to change how you feel,” explains Patricia Celan, MD, a senior psychiatry resident at Dalhousie University in Canada.
“Such comments can be seen as dismissive and minimizing,” continues Dr. Celan.
“People would rather feel heard and be told that their feelings are valid, instead of being told to not have those feelings at all – an invalidating response that makes people not want to further confide in the speaker.”
THINK before you tell a person not to worry, even if they’re very visibly upset about something, even if they’re crying.
People want solutions, not invalidation of their emotions.
Even if no solution exists, it’s still highly inappropriate to say those two words. They are overused, patronizing and insulting.
 Dr. Celan is a post-graduate trainee in psychiatry, working in diagnosing and treating patients with psychiatric conditions. She is passionate about psychotherapy, especially in trauma, anxiety and depression.
Dr. Celan is a post-graduate trainee in psychiatry, working in diagnosing and treating patients with psychiatric conditions. She is passionate about psychotherapy, especially in trauma, anxiety and depression.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Do Obese People Only Go Through the Motions with Exercise?

Many obese people insist that they exercise as much as any lean person.
About 80 percent of personal-training clients are overweight women.
But the truth is, the percentage of clinically obese individuals at health clubs or parks (on the walking/jogging/biking/inline skating paths) is drastically lower than the percentage in general areas such as malls, festivals, busy streets, business centers, ball games, concert halls, etc.
Visit any place where people are exercising or getting in physical activity. You will see few people who are significantly overweight.
This isn’t because the very overweight can’t perform the exercise or activity.
I don’t expect to find very heavy people skateboarding, but I’m talking about more practical activities like walking, slow jogging, basketball, tennis. And of course, working out with weights.
An issue of the Journal of Nutrition Education and Behavior (Jan/Feb 2010) delves into the strange paradox:
The solution to obesity and its accompanying hazards is exercise (along with smart eating habits), yet, most obese U.S. people do not have a structured, comprehensive approach to exercise.
First, let’s define exercise.
The shopping you did at Kohl’s or Walmart does not comprise your exercise regimen for the day.
Nor does housework. And leisurely walking your Pomeranian around the block a few times doesn’t count, either.
Exercise that works is that which keeps the heart rate elevated for at least 20 minutes nonstop.

If housework keeps your heart rate elevated, this means you’re in poor condition and need to perform structured cardio routines (treadmill, outdoor arm-pumping walking, step class, elliptical machine, staircase machine, cycling).
And a program also of strength training will make housework less fatiguing.
The variable for the obese individual is making time for deliberate, structured, bilateral, neutral-spine-positioned cardio and strength training workouts, regardless of how much “walking” you did at the mall that day, or how much hassling you did carrying around your toddlers that day.
RESEARCH
Researchers at The George Washington University Medical Center analyzed survey results from 1,552 people, of whom 989 were overweight.
Some results: Overweight people believed that exercise enhanced self-image and appearance more so than normal weight subjects.
Overweight participants felt more intimidated and self-conscious about exercise (under most circumstances) than non-overweight people.
And the negative emotions that go with the health club experience may be greater in obese people when it comes to dictating the decision to exercise.
The study authors note that “…it would be wise for exercise professionals and commercial health clubs to help OW people feel more comfortable around those who are different from themselves and to minimize the intimidating aspects of the exercise environment, while promoting the benefits of exercise to personal health and wellbeing.”
It is no secret that many obese and even moderately overweight people won’t exercise at gyms due to self-consciousness.
However, exercise can begin inside the comfort of the house. Fancy, noisy, space-consuming equipment is not necessary.
If you’re obese and not working out, you can start with a used stationary bike for $25, and used treadmills are pretty cheap, if money is an issue.
Or exercise to cable channel fitness programs, or purchase some exercise CDs. You can even follow YouTube workouts.
Though the percentage of obese people who exercise at gyms is way smaller than the percentage of very heavy people in the general population, I’d have to say that enough overweight women and men show up at health clubs to conclude that self-consciousness and intimidation obviously don’t stop these particular individuals from doing what’s right for their body.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ Halfpoint
Source: sciencedaily.com/releases/2009/12/091217133738.htm
Do Obese Women Strength Train Differently than Thin Women?
Obese women indeed strength train differently than thin women, and this is one of the reasons they can’t lose weight.
Obese women strength train a lot differently than their lean counterparts, and while this creates obstacles to fat loss, it’s important to know that it is not the obesity that causes overweight individuals to work out differently than thinner ones.
In my years in the fitness industry, as well as being a “gym rat,” I have observed a very intriguing phenomenon in the way that women of different sizes work out.
First of all, in general, most women, regardless of amount of body fat, tend to use light weights when doing resistance exercise.
There is a range within this range, so that some women use very light weights, while others use heavier than average weights, and only a very small percentage use a “Wow!” amount of resistance.
Most women do not want a muscular look. The muscular look, however, results from very low levels of body fat in combination with a very-well-strength-trained body. Low levels of body fat make the musculature visible.
Obese women almost always use particularly light resistance, whether it’s with a machine, dumbbells or barbells.

hutterstock/Lisa F. Young
Trust me when I say that this is NOT because their excess size prevents use of heavier resistance. Strength training is not the same as running.
There is nothing about obesity that makes a woman physically weak in the sense of strength training.
A very large person is on an even playing field as a lean person when it comes to weight workouts.
Ask an obese woman who strength trains why she strength trains.
She will probably tell you to lose pounds. However, training with light weights will not get her the desired results.
Overweight women usually fear that if they use heavy or even moderate resistance, or work out in a way that feels intense, that they will get bigger. This is a myth.
Go to any crowded gym and observe how obese women do strength training. The weights are often very, very light.
They are afraid of getting bigger if they use more than a light resistance. I’ve had my obese clients use heavier weights—without any problem as far as performing the exercise. They have the ability, but the myth gets in the way.
This phenomenon is particularly obvious with the lat pull-down, any chest press, bench press, seated row and bent-over dumbbell row.
Now, look at the women who are lean and buff. How much weight are they lifting? Almost always, it’s a lot more than light, and often it’s “a lot for a woman.”

In other words, an obese woman will be using 50 pounds for a lat pull-down, while the lean, tight, buff size 6 counterpart will be pulling down 115 pounds.
The best way for the obese to lose body fat via exercise is to lift heavy, and intensely.
Intense strength training with moderate to heavy resistance ignites a hormonal response in the body that causes an accelerated resting metabolism.
This hormonal response does not occur with light exercise!
An obese woman’s body will shrink, shrink and more shrink only when she begins using moderate weights with high intensity, or heavy weights with medium to high intensity.
The formula for this, in general, is using a load that makes 8-12 repetitions exceedingly difficult. If you can do more than 12 reps, increase the resistance!
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.