Can a Low Thyroid Cause Missed Periods?

If you’ve been missing some periods lately but are too young to suspect perimenopause, have you considered low thyroid as a possible cause?
But keep in mind that even a woman of perimenopausal or premenopausal age can still develop underactive thyroid disease. (more…)
Can Two Periods in One Month Mean the Start of Menopause?

There are a few causes of two periods in one month and many women believe that menopause is one of them.
However, what seems to be two periods in one month may be something more sinister… (more…)
Is Pasta Really As Bad As Its Reputation for Fat Gain?

Looks like all the backlash against pasta over the years as a weight gain food has been undeserved.
Now research shows that pasta, which has a low glycemic index, isn’t bad at all for people trying to lose fat.
Foods with a low glycemic index cause a slower rise in blood sugar than do foods that are rated high.
Research from St. Michael’s Hospital
Researchers identified 30 randomized control trials that involved nearly 2,500 pasta eaters — people who did not regularly consume other forms of carbohydrates — as part of a low glycemic diet.
“The study found that pasta didn’t contribute to weight gain or increase in body fat,” says the lead author, Dr. John Sievenpiper, in the paper, which appears in the April 2018 British Medical Journal Open.
“In fact analysis actually showed a small weight loss,” continues the paper. “So contrary to concerns, perhaps pasta can be part of a healthy diet such as a low GI diet.”
Better Type of Pasta
Ideally you’ll want the pasta to be fresh-made at home rather than in a microwavable frozen box or tub that’s full of additives — including added sugars!
The Study
The study subjects averaged 3.3 pasta servings per week instead of other carb foods, wherein one serving = about half a cup of cooked pasta.
The subjects lost about half a kilogram of weight over an average follow-up of 12 weeks.
Context Must Be Considered
The report points out that the results apply to pasta eaten with other low glycemic foods as a part of a low glycemic diet – rather than heaps and heaps of pasta eaten along with lots of high glycemic carbs or other kinds of diets.
“As a rule of thumb, everything should be eaten in moderation,” says Shana Spence, MS, RDN, CDN, a registered dietitian nutritionist based in New York, who was not involved in the study.
Moderation for pasta would mean a cup or two, depending on the circumstances.
For instance if you killed it at the gym with an intense and heavy weight workout, two cups of pasta (with protein!) would be appropriate.
For a late evening snack, one cup is better.
“There are also so many different types of healthier pasta options available now, it really should not be counted as something negative anymore,” continues Spence.
“There is whole wheat pasta that has more fiber than its white version. There are also protein versions now made with legumes such as chickpeas.
“There is also nothing wrong with eating the original white pasta.
“Just be mindful of portions especially when you’re eating out at restaurants since they tend to provide double and triple the size.”
 Shana Spence of The Nutrition Tea is committed to providing trending information and nutrition facts covering a wide range including nutrition for heart disease and diabetes, pediatric nutrition and healthful lifestyles.
Shana Spence of The Nutrition Tea is committed to providing trending information and nutrition facts covering a wide range including nutrition for heart disease and diabetes, pediatric nutrition and healthful lifestyles.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Source: sciencedaily.com/releases/2018/04/180403085034.htm
Lily’s Stevia Chocolate Bars’ Added Inulin Causes Farting

Lily’s Stevia sweetened chocolate bars may as well be called “fart bars” because their excessive amount of inulin causes flatulence.
One bar contains 22 to 24 grams of fiber. (more…)
8 Exercises Fat People Can Do As Well As Thin People

If you think you’re too fat to work out at the gym, you’re so wrong, as there are 8 REAL exercises that very big people can do as well as thin people. (more…)
Relief of Osteoarthritis Knee Pain without Drugs, Surgery

A breakthrough shows an effective treatment that relieves the pain of osteoarthritis in the knee without drugs or surgery.
The treatment doesn’t even require any hospital stay, recovery time or rehab exercises.
Osteoarthritis is a degenerative condition that involves a progressive wearing down or thinning of the cartilage in the knee joint.
For some patients the result is eventually a bone-on-bone contact, causing a lot of pain just from walking.

Bone-on-bone contact of osteoarthritis. Scuba-limp/Commonswiki
Pain Relief from Knee Osteoarthrits: No Drugs, No Joint Replacement
The simple and painless procedure is called geniculate artery embolization (GAE).
This image-guided treatment blocks arteries in the knee, resulting in less inflammation and therefore less pain.
“Geniculate artery embolization is a relatively new procedure [as of 2022] for treating arthritis pain in the knee,” says Marc F. Matarazzo, MD, a board certified orthopedic surgeon with Total MD Family Medicine & Urgent Care.
“There are several randomized controlled trials currently being conducted.
“This procedure uses a minimally invasive technique to disrupt the blood flow at the site of pain.
“It is thought that this inhibits neovascularization [growth of new blood vessels], leading to the breakdown of tissue and feeding of inflammation and knee osteoarthritis.
“There are some promising initial data regarding its efficacy.
“This should not be confused with geniculate nerve radiofrequency ablation, which is also a minimally invasive treatment for pain related to osteoarthritis of the knee.
“This procedure has a more established track record and has been shown in one study to be superior to NSAIDs and an intra-articular cortisone injection.”
How is GAE done?
• An interventional radiologist inserts a catheter through an incision the size of a pinhole.
• This blocks the very small arteries within the knee’s lining, reducing inflammation caused by the osteoarthritis.
• GAE is an outpatient treatment.
• It takes 45 to 90 minutes.
In a small study by Bagla et al, there were no adverse side effects of the procedure.
After one month, patients continued to report pain relief.
If you’re suffering from the pain of osteoarthritis in your knee, you may want to ask your orthopedic surgeon about geniculate artery embolization.
But keep in mind that GAE is not a cure for the degenerative process of osteoarthritis.
 Dr. Matarazzo specializes in sports medicine and related injuries. He performs minimally invasive and complex reconstructions, and joint replacements, of the shoulder and knee. Dr. Matarazzo is certified in the MAKO robotic-assisted knee replacement system and has 20+ years of orthopedic experience. He has a special interest in cartilage restoration and preservation.
Dr. Matarazzo specializes in sports medicine and related injuries. He performs minimally invasive and complex reconstructions, and joint replacements, of the shoulder and knee. Dr. Matarazzo is certified in the MAKO robotic-assisted knee replacement system and has 20+ years of orthopedic experience. He has a special interest in cartilage restoration and preservation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Depositphotos.com
Alzheimer’s Breakthrough: Prevent Disease with Common Painkiller?
A breakthrough in the prevention of Alzheimer’s disease may be on the horizon, thanks to researchers who believe a common painkiller may prevent this killer from striking. (more…)
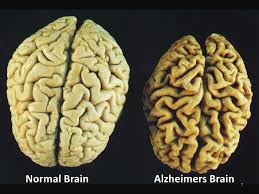
Does Slow Walking Actually Damage the Brain (Dementia)?
A study links slow walking with dementia, but what exactly does this mean?
Does slow walking damage brain cells?
The study concludes that slow walking in older adults means a higher risk of dementia, and this includes the ability to think and make sound decisions. (more…)
Sitting too Much Is Linked to Problems Peeing
The “sitting disease” is back in the news: Excessive sitting is linked to issues with voiding: lower urinary tract symptoms.
Problems with peeing in the case of extended sitting time refer to issues with urinating and/or storing urine.
The association between peeing problems and prolonged sitting (as well as overall sedentary lifestyle) is a finding that’s reported in the BJU International (March 2018). The study involved 69,795 Korean men of middle age.
Lower urinary tract problems were 39 per 1,000 person-years, says the study.
A person-year refers to the number of years of follow-up multiplied by number of people in a study.
Problems Peeing May Be Related to Excess Sitting Time
“The results support the importance of both reducing sitting time and promoting physical activity for preventing lower urinary tract symptoms [LUTS],” explains lead author Dr. Heung Jae Park in the BJU paper.
“Further studies are still needed to examine the influence of sedentary behaviors on LUTS and its determinants,” says senior author Dr. Seungho Ryu in the same paper.
Nevertheless, this study is an eye opener and brings more awareness to the sitting disease – which has been called the “new smoking,” because excess time with your butt in a seat is associated with the same severity and type of cardiovascular health problems as is smoking.
In addition to problems with peeing, excessive sitting is also linked (and very strongly at that) to coronary artery disease, chronic heart failure, high blood pressure, type 2 diabetes, deep vein thromboses and spinal problems.
Rid the Sitting Disease
Two ways to break free of the sitting disease are to walk about the room or pace forward and backward while watching TV, and to get in the habit of using a treadmill desk for computer work.
You may also want to wear a high quality pedometer to track the number of steps you get in daily. Aim for at least 6,000 and ideally 10,000.
This will be an incentive to reduce your sitting time throughout the day.
If you regularly do stretching exercises for your legs, do them while standing.
For example, hamstring stretches can easily be done while standing by propping a foot on a height and gently leaning your chest towards your knee.
Additionally, see if you can replace some seated strength training exercises with a standing version.
For example, replace a seated dumbbell curl with standing, and seated overhead dumbbell press with standing.
Little changes like this will go a long way in cutting back on the amount of time you spend in a chair.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.









































