Can a Drooping Eyelid Be Caused by TMJ Disorder?

An eyelid that’s suddenly drooping can be frightening to anyone who knows that a brain aneurysm can cause this, but can TMJ disorder also cause this unnerving symptom? (more…)
Can Acute Liver Damage from Heart Failure Cause Ascites?

Ascites has many potential causes, but liver disease is notorious for causing this abdominal fluid buildup.
What if heart failure is behind the liver disease? (more…)
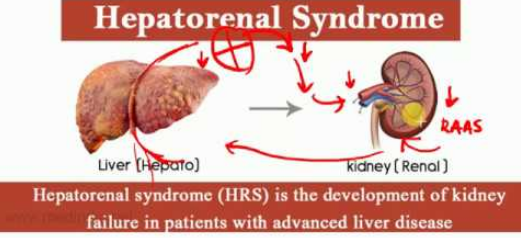
Can Ischemic Hypoxic Liver Cause Hepatorenal Syndrome 1 ?
Ischemic or hypoxic liver (lack of oxygen) can be caused by heart failure, and it’s logical to wonder if this can lead to hepatorenal syndrome type 1 – which has a very dismal prognosis. (more…)
Why Dark Chocolate Is a Health Food: Certain Kinds, That Is

It’s old news that dark chocolate has health-giving phytonutrients, but research shows that certain kinds of dark chocolate are especially good for the body.
And in a way that you’re probably not assuming. (more…)
How Many Elderly Have Undiagnosed Sleep Apnea?

Sleep apnea is one of the most under- and misdiagnosed conditions in the elderly; the estimated number who have it is alarmingly high, and this includes non-overweight as well as female older people.
Symptoms of sleep apnea in the elderly can easily mimic signs of other conditions such as “old age” and “age-related” fatigue, loss of energy, issues with concentration and falling asleep in front of the TV or while doing something else passive such as reading or crocheting.
“Sleep apnea is very common in the elderly, and some studies have shown a prevalence between 20 and 40%, and this prevalence steadily increases with advancing age,” says Daniel Rifkin, MD, a sleep medicine expert at the Sleep Medicine Centers of Western New York.
“This is almost double the prevalence in the younger adult populations!
“Because untreated obstructive sleep apnea is associated with heart disease and strokes, among many other medical conditions, and worsens quality of life, we should focus our efforts on treating our older patients.
“Instead of laughing at grandma falling asleep at the kitchen table during lunch or dinner, we should take it seriously and urge her to get her sleep evaluated.”
Excessive Daytime Sleepiness Is NOT Normal in the Elderly
It’s likely due to obstructive sleep apnea.
This is what University of Michigan researchers have found.
According to their study, 56% of people over 65 have a high risk of obstructive sleep apnea.
How was the study done?
1,052 Medicare recipients completed a sleep questionnaire plus other surveys as part of the National Health and Aging Trends Study.
The study found that 94% of those at risk turned out to actually have OSA.
Though OSA is common, it’s one of the most misdiagnosed conditions.
One reason is that its symptoms mimic what seems to be the inevitable signs of advancing age.
Falling asleep in the middle of the day, during supper or having difficulty concentrating are signs that wouldn’t be as alarming in an elderly person as they would be in a 45-year-old. Thus, a diagnostic workup wouldn’t as likely be pursued.
The second reason is that it can’t be diagnosed with a simple blood test, biopsy sample or X-ray.
Rather, it requires a sleep study, and many people just do not want to get hooked up to wires overnight.
A third reason for the massive under-diagnosis of OSA in the elderly (and younger) is because many people anticipate being told they’ll need to “sleep with a mask” if they’re diagnosed. So they deny they might have OSA.
The study appears in the April 2018 Journal of the American Geriatrics Society.
 Dr. Rifkin is board certified in both neurology and sleep medicine. He also treats insomnia, RLS and narcolepsy.
Dr. Rifkin is board certified in both neurology and sleep medicine. He also treats insomnia, RLS and narcolepsy.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: newswise.com/articles/view/694298/?sc=mwhn
Exercise or Take It Easy After a Heart Attack?

The old school of thought among doctors was to take it easy for the rest of your life after a heart attack rather than increase exercise. (more…)
Reasons to Eat Nutmeg: Liver Health and Many More Benefits
The spice nutmeg has been found to be healthy for the liver.
“Nutmeg contains the compound myrislignan, which was found to help protect the liver,” says Shana Spence, MS, RDN, CDN, a registered dietitian nutritionist based in New York.
“This is probably due to the anti-inflammatory properties in the compound, but more research still needs to be done to pinpoint the exact reasoning behind this.”
Researchers have discovered that nutmeg can aid in liver toxicity (and also heart tissue damage).
The findings are published in the Journal of Proteome Research (2018).
The Study
A mouse model of liver toxicity was used to test the mechanism behind the spice’s protective effects.
It’s believed that nutmeg helps fight liver damage by restoring more desirable levels of a variety of blood fats and acylcarnitines.
It was the myrislignan that was found to have a strong protective impact on damage to the liver.
“In addition to myrislignan, nutmeg also contains fiber, manganese, thiamin, vitamin B6, folate, magnesium and copper, which all contribute to health,” says Spence.
“Other health benefits include pain relief from inflammatory diseases, treatment of insomnia, antibacterial benefits that help prevent tooth decay and other anti-cariogenic [resistant to tooth decay] properties.
“However, nutmeg is one spice that is used sparingly in dishes because of its strong flavor — so nutmeg oil is another alternative.”
Nutmeg and Blood Sugar
Nutmeg may help combat high blood sugar and excess fat in the blood due to its bioactive compounds.
Nutmeg contains antioxidants that can help reduce oxidative stress and inflammation, which are associated with diabetes and cardiovascular diseases.
Also, some studies suggest that nutmeg can influence glucose metabolism and improve insulin sensitivity, potentially aiding in blood sugar control (Journal of Diabetes Research, 2015).
This spice also contains compounds that might help lower cholesterol levels and reduce fat accumulation in the blood (European Journal of Clinical Nutrition, 2018).
What if You Don’t Like Nutmeg?
If you’re not too fond of the distinct flavor of this healthful spice, you can sneak it into a protein drink.
For myself, nutmeg and my palate don’t quite get along, so I put it in something that I already don’t like the taste of: my post-workout protein drink.
The one level-teaspoon of the powder form of nutmeg that I add with the four ounces of pomegranate juice, water, vanilla protein powder, ground flax and chia seeds plus cinnamon, actually gets noticed in the flavor of this concoction.
But it’s tolerable to my palate. And if I can tolerate it mixed into my protein drink, chances are, others who find the spice too strong will as well.
 Shana Spence of The Nutrition Tea is committed to providing trending information and nutrition facts covering a wide range including nutrition for heart disease and diabetes, pediatric nutrition and healthful lifestyles.
Shana Spence of The Nutrition Tea is committed to providing trending information and nutrition facts covering a wide range including nutrition for heart disease and diabetes, pediatric nutrition and healthful lifestyles.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
Source: sciencedaily.com/releases/2018/05/180509104934.htm
Bone & Muscle Health in Older Women: Mediterranean Diet

If you’re past menopause and want stronger bones and muscles, consider the Mediterranean diet, says a study.
Postmenopausal women who were on the Mediterranean diet were found to have higher bone and muscle mass than those who were not.
“After menopause, a decrease in estrogen can cause a loss in muscle and bone mass in older women,” says Sara Artigues, a registered dietician and certified personal trainer out of New Orleans.
“The Mediterranean diet consists of eating a high intake of fruits, vegetables, grains, olive oil, nuts and seeds, and a moderately high fish intake.”
Mediterranean Diet Food Pyramid
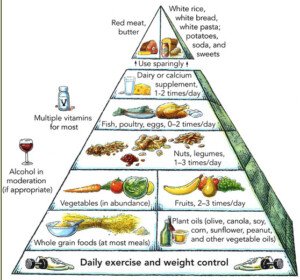
Muscle mass can be added to postmenopausal women who strength train. But what they eat is crucial for optimal progress with their strength training.
The 2018 Study
• 103 healthy women from Brazil
• Average age of 55 and all postmenopausal
• All underwent bone scans to measure bone mineral density, total body fat and lean muscle mass.
• The participants completed a food questionnaire of what they had eaten in the prior month.
The questionnaire determined a Mediterranean diet score. A higher score meant a higher adherence to the diet.
And a higher score was greatly associated with a higher bone mineral density at the lumbar spine, plus with greater muscle mass.
Something to Consider
You might be thinking that women who strength train are more likely to eat Mediterranean style, and thus, they would have stronger bones and muscles.
Though whether or not the subjects did any strength training was not factored into the analysis, what WAS adjusted for was the number of steps they took for six days, as recorded by a pedometer.
Also adjusted for was hormone replacement therapy and smoking, which impact bone density.
“This diet has been linked to lowering the risk of heart disease, cancer and diabetes,” adds Artigues.
“Being a largely plant based diet means that polyphenols are present in greater numbers in the body.
“These polyphenols fight cancer and inflammation which both contribute to poor muscle and bone health.
“The Mediterranean diet, full of healthy fats, can help you maintain a healthy weight which is important to both bone health and muscle mass.
“Following a diet high in vegetables and lean proteins and other healthy heart nutrients can help older women maintain muscle strength and weight.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
 Sara’s training services include fitness/body composition assessments, nutrition planning, customized programs and spin class instruction for a variety of clients.
Sara’s training services include fitness/body composition assessments, nutrition planning, customized programs and spin class instruction for a variety of clients.
.
Top image: Freepik.com
Source: sciencedaily.com/releases/2018/03/180318144826.htm
Choking Feeling from TMJ Disorder: Causes & Solutions

A choking sensation can be caused by a TMJ disorder, but TMJ problems are not among the most common causes of a choking feeling.
It’s scary as hell to suddenly feel that you’re choking or have to gasp for air. (more…)
Serious Diseases that Can Mimic TMJ Disorder

It’s happens: Someone is diagnosed with TMJ disorder but later learns it’s a misdiagnosis of a very serious disease, like a brain tumor or heart problem.
The symptoms of temporomandibular joint disorder are very similar to the symptoms of more serious medical conditions. (more…)