
If the MRI is so sensitive to picking up cancer in very dense breasts, why shouldn’t women with non-dense or fatty breasts ALSO benefit from annual MRIs?
After all, MRIs can pick up a lot of things that mammograms (and ultrasounds) can’t.
A study from Germany says that MRI screening makes early diagnosis more possible in women with average breast tissue – women at average risk – and this means non-dense breasts.
Traditionally, the MRI has been recommended only for women at high risk for breast cancer.
This imaging tool has never been the one of choice for women with average risk of breast cancer, even though mammograms have a 20% “miss” rate for women with average risk of disease.
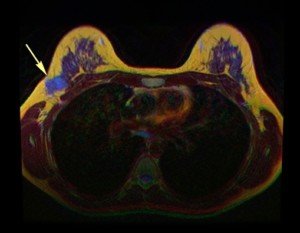
The arrow in this breast MRI points to cancer. © Nevit Dilmen/CreativeCommons
MRI Study: Intriguing Results
Christiane Kuhl, MD, decided to pursue the efficacy of MRI for detecting breast cancer in “regular” breasts.
- The impact of MRI on 2,120 women, 40-70, was studied.
- The women had been determined to have a less than 15 percent lifetime risk of disease.
- The women’s mammograms were normal.
- Women with dense breasts also underwent ultrasound with normal results.
Disturbing Discoveries
- MRI of the subjects detected 60 cancers.
- This translates to a detection rate of 15.5 per 1,000 women.
- The study, which appears in the Feb. 2017 Radiology, also revealed MRI’s superiority over ultrasound.
With about 240,000 women in the U.S. every year getting diagnosed with breast cancer, why isn’t MRI as standard as the mammogram – even if a woman is willing to pay out of pocket and doesn’t mind lying inside the equipment?
Dr. Kuhl’s paper points out that MRI finds malignant tumors that mammography would eventually find – but that MRI detects them sooner.
The report also notes that if the MRI had not been done, those additionally-caught masses would have progressed to interval cancers.
Interval masses refer to those that the patient or doctor discover with the fingers in between imaging procedures.
The earlier that breast cancer is caught, the more curable it is. So why then, aren’t MRI’s routine for non-dense breasts?
“This study was evaluating average-risk women, meaning, those with background lifetime risk (12%, 1/8 over the course of their lifetime), with non-dense breasts and history of normal imaging,” begins Anjali Malik, MD, a board certified diagnostic radiologist with Washington Radiology in Washington, DC., who was not involved in the study. She interprets mammograms, breast MRIs and ultrasounds, and performs biopsies.
“Screening examinations are meant to be accessible, easy, quick, cheap tests with good sensitivity and specificity to detect a disease that, when caught early, is curable.
“This study clearly demonstrates the excellent specificity and sensitivity of contrasted breast MRI.
“However, the cost, limited accessibility (less centers, magnets and techs for MRI, length of time, even if abbreviated, due to IV placement, checking renal status), and risk (gadolinium contrast is not without risk) make MRI a poor screening examination for those with average risk.”
Issues with MRI
- If a woman with non-dense breasts and no other high risk factors doesn’t mind lying in the “tube” and paying out of pocket, she can still pursue a breast screening MRI for her peace of mind. But she also needs to know that MRI has a much higher false-positive rate than do mammograms.
- All people who undergo a contrast MRI must be injected with the gadolinium dye.
- If the patient has compromised kidney function, they will be refused the procedure because the chemical dye is toxic to the kidneys.
- Furthermore, in very rare cases, the patient has a life-threatening allergic reaction to the dye.
- So overall, it’s not efficacious for MRI to be a routine screening procedure for women with non-dense breasts and average risk.
“Thus, it is reserved for those women with increased lifetime risk for the development of breast cancer, where MRI certainly has a place as part of a high risk breast cancer screening protocol,” says Dr. Malik.
For example, a woman with non-dense breasts but who’s positive for a BRCA mutation would be a candidate.
A woman with heterogeneously dense breasts whose sister was diagnosed with the disease would also be a candidate for MRI screening.

 Dr. Malik
Dr. Malik
























