The obesity rate in America keeps shooting up; this defies claims that “some people are meant to be big.”
There is now a proposed new definition of obesity that could dramatically change how many Americans are considered obese.
Researchers from Mass General Brigham say that using updated criteria developed earlier in 2025 by the Lancet Diabetes and Endocrinology Commission increases the estimated U.S. obesity rate from about 40 percent to nearly 70 percent.
The research team analyzed health data from more than 300,000 people.
The biggest jump appeared among older adults, but the shift affected nearly every age group.
The study also found that many people who would now fall under the updated definition face higher risks for serious health conditions. The findings were published in JAMA Network Open.
This new definition isn’t as straightforward as what the scale says or even what the BMI number is.
Why BMI Alone Doesn’t Tell the Whole Story
For decades, obesity has mostly been defined using body mass index, or BMI. BMI is calculated using height and weight, which makes it simple and easy to apply on a large scale.
But BMI has a major limitation. It doesn’t show where fat is stored in the body or how much of a person’s weight comes from muscle versus fat.
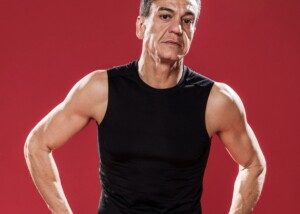
Thus, BMI would seem to be the most inaccurate when applied to muscular athletes, particularly male bodybuilders, leaner football players and other adults whose sports or passions involve building muscle.
On the other hand, a BMI of 50 surely indicates a very substantial amount of surplus body fat, no matter how much muscle that individual has from lifting weights at the local gym.
In short, BMI fails to identify body composition. Two thinner people could have the same low BMI, while one has much more muscle and less body fat (healthier composition) than the other.
Other measurements, such as waist circumference, waist-to-height ratio, and waist-to-hip ratio, offer more detail, more accuracy.
These measurements are especially helpful for identifying abdominal fat, which is strongly linked to heart disease, diabetes and other health risks.
How the New Obesity Framework Works
Under the updated approach, obesity can be identified in two main ways.
- One group includes people with a high BMI plus at least one elevated body-fat measurement. Researchers refer to this as BMI-plus-anthropometric obesity.
- Another group includes people with a normal BMI who still have at least two elevated body-fat measurements.
- An example would be someone who doesn’t look overweight in a suit (BMI of 23), but underneath is excess abdominal fat. This category is called anthropometric-only obesity.
The framework also divides obesity into preclinical and clinical forms. Clinical obesity is defined by physical impairment or organ dysfunction related to excess body fat.
So far, at least 76 organizations have endorsed the new standards, including the American Heart Association and The Obesity Society.
However, this new definition is going to go over very poorly with that segment of the population that denies obesity’s impact on health.
Study Results Show a Much Higher Obesity Rate
The researchers used data from the National Institutes of Health All of Us Research Program, which includes a diverse group of more than 300,000 Americans.
Using the traditional BMI based definition, the team found that 42.9 percent of participants were classified as having obesity.
When the new criteria were applied, that number jumped to 68.6 percent. The entire increase came from people classified as having anthropometric-only obesity.
These individuals would not have been labeled as having obesity under older guidelines.
The guy in the suit, who kind of looks lean, but has the excess fat in his middle, would have a BMI of 23 (normal range).
But a body fat analysis done with a skin-fold caliper at various points on the body would reveal a body fat percentage in what the American Council on Exercise calls the “obese” category: at least 25 percent — regardless of what the person looks like or what the scale says.
Though this numerical value is close to his BMI’s, body fat percentage is nowhere near the same as BMI as an indicator of “how much fat someone has.”
So in this study, obesity rates varied by gender and race, but age had the strongest effect. Nearly 80 percent of adults over age 70 met the new definition.
Health Risks Are Higher in Newly Classified Individuals
The study also showed that people with anthropometric-only obesity had higher rates of diabetes, cardiovascular disease and premature death compared with people without obesity.
About half of all participants who met the new definition were classified as having clinical obesity.
Recall that clinical obesity means that the excess fat impairs the body’s mobility or function, or has a negative impact on an organ.
That almost 50 percent was only slightly lower among those with anthropometric-only obesity compared with those who had both high BMI and elevated body-fat measurements.
“These findings reinforce what we’ve suspected for a long time,” says senior author Steven Grinspoon, MD, Chief of the Metabolism Unit at Mass General Brigham.
He adds: “BMI alone misses people who are clearly at higher health risk.”
More Research Coming
The researchers say more studies are needed to understand why anthropometric-only obesity develops and how best to treat it.
Their team has already developed a therapy aimed at reducing waist circumference and plans to study how different treatments may work for this newly defined group.
“Body composition matters,” says co-first study author Lindsay Fourman, MD, with Mass General Brigham.
She says what personal trainers and others in the fitness industry have known for years:
“Even people with a normal BMI but higher abdominal fat are at increased health risk. It’s not just about the number on the scale.”
It’s not hard to believe why, in the wealthiest country on earth, the obesity rate keeps climbing more than what would be expected with population growth — and this refers to the “old” definition of obesity, too.
With this new definition, the rates can only exponentially increase more than ever.
The U.S. has become the poster child for a sedentary lifestyle coupled with abundant opportunities for overconsuming high calorie foods. None of this has anything to do with genetics or “I’m just meant to have a bigger body.”
![]()