Ischemic or hypoxic liver (lack of oxygen) can be caused by heart failure, and it’s logical to wonder if this can lead to hepatorenal syndrome type 1 – which has a very dismal prognosis.
Hepatorenal Syndrome Type 1
• Survival means a liver transplant.
• Without a new liver, the patient may live days to about 10 weeks.
• Type 2 hepatorenal syndrome has a much better prognosis and can usually be treated without a liver transplant.
An ischemic or hypoxic liver can occur in the setting of longstanding heart failure with depressed ejection fraction: The heart has been pumping very weakly for a long time.
When the liver suddenly crashes (acutely fails), the kidneys will be in this path.
But acute kidney failure in the presence of a rapidly deteriorating liver doesn’t always mean hepatorenal syndrome type 1.
“Theoretically, any form of severe acute liver injury causing fulminant [sudden onset] hepatic failure or acute liver failure can lead to HRS,” explains Daniel Motola, MD, a top board certified gastroenterologist and hepatologist providing same-day and next-day services in NYC with Gotham Medical Associates.
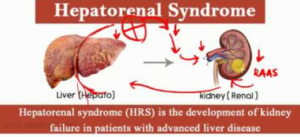
“Severe hepatic dysfunction resulting in portal hypertension, splanchnic vasodilation and upregulation of the renin-angiotensin system leads to HRS,” continues Dr. Motola.
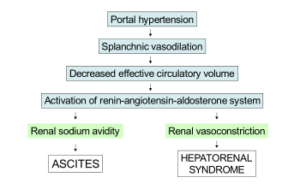
What is portal hypertension?
Blood to the liver mostly comes via the portal vein in this organ. High blood pressure in this vein will cause a backup or congestion, restricting blood supply.
This dire situation can occur due to a local cause (problem within the liver) or an extra-hepatic cause (weak blood output from a sick heart).
“Cirrhosis is not a requirement for hepatorenal syndrome,” says Dr. Motola. “Take for example patients with acute liver injury from alcoholic hepatitis [hepatitis means inflamed liver, not viral infection].”
“HRS in cardiac disease-induced acute liver failure is complicated, as there is likely to be low flow state to the kidneys as well as the liver, thus resulting in hypoxic injury to multiple organs.
“Therefore, it may be hard to distinguish HRS in such a patient from acute nephrotoxicity caused by low cardiac output.”
In other words, a patient may suddenly start developing very concerning symptoms.
And in this case, in the ER it’s determined that acute liver failure, or a sudden worsening of this organ, is in progress, manifesting as jaundice and altered mental status.
However, tests also show worsened kidney function, which may not be causing any symptoms other than perhaps infrequent urination, but the blood creatinine test for renal function is very telling.
If this patient has a history of progressive heart failure, and the CT scan and other tests are negative for alcoholic cirrhosis, a viral infection, liver toxicity and local liver pathology (e.g., cancer), then one can deduce that the acute liver and kidney injuries are being driven by very poor cardiac output.
- But is the kidney failure directly “downwind” from the liver failure?
- Or did the kidneys, by sheer coincidence, decide to give up the good fight at the same time that the liver decided to throw in the towel – after years of struggling to stay afloat in the setting of poor cardiac output?
There’s really no way to tell. But it’s certainly possible for the sequence to develop as follows:
1) Chronic heart failure
2) Chronic but subclinical hepato-insufficiency resulting from poor perfusion (blood flow) from heart failure.
3) Fulminant liver failure due to hypoxic threshold (tipping point beyond which the liver, having been chronically shorted of oxygen-containing blood, takes a steep decline).
4) Hepatorenal syndrome type I, as described previously.
If you are interested in a consultation with one of Gotham Medical Associates’ gastroenterologists please call 212-227-3688 or book online. Our staff will be happy to assist you, your family member or friend!
NOTE: Signs of liver failure warrant a trip to the emergency room. They include altered mental status or confusion, difficulty talking, extreme weakness, grogginess, loss of appetite and yellowish skin.

 In addition to his liver transplant expertise,
In addition to his liver transplant expertise, 







































