Twitching Tongue: Bulbar ALS or Normal?

If your twitching tongue is driving you mad with anxiety and fear of bulbar onset ALS, then you need to know how to rule out bulbar onset ALS, which is diagnosed in only about 600 people every year in the U.S.
However, for some panicky individuals, this number is no reassurance if their tongue is twitching, and especially if they’ve been perceiving accompanying symptoms such as a heavy-feeling tongue, or a lopsided tongue.
Other Perceived Symptoms
Others that can cause alarm over bulbar onset ALS in some hyper-alert individuals include difficulty swallowing, and the inability to rapidly speak a particular selection of words without mispronouncing one.
Fear can play abominable tricks on the vulnerable mind.
People with bulbar onset fear are very capable of spending huge amounts of time every day examining their tongue in a mirror for all sorts of nuances, ranging from comparing one side to the other, to counting the number of indents in the tongue.
Other tongue tests for bulbar that can consume a fearful person’s time include rapidly moving the tongue from side to side; pressing it as hard as possible to the roof of the mouth or to the side; sticking it out to see if it twitches; rapid chewing; and chewing tough foods.
No matter how many tests such an individual subjects himself to, there’s never enough reassurance that they do not have bulbar onset ALS.
But is this endless menagerie of testing necessary?
“If a person is really worried about having bulbar onset ALS, inspecting the tongue is not the exam to perform,” says Kristina Lafaye, MD, a board certified neurologist specializing in clinical neurophysiology and neuromuscular medicine with Tulane Doctors Neurosciences.
“If they do not have any problems with swallowing, chewing, or controlling their secretions, then they do not need to bother looking at their tongues.”
Nevertheless, visual inspections of the tongue is a common, time-sinking occurrence amongst individuals suffering from bulbar onset hypochondria.
Dr. Lafaye emphasizes, “Looking at the tongue is irrelevant.”
She adds, “Bulbar onset is marked by problems swallowing, chewing, and controlling secretions.
“There is coughing and a perception of food (liquids) ‘going down the wrong way.'”
As for swallowing, chewing and controlling secretions, keep in mind that if you fixate on these elements, you’ll be prone to imagining or perceiving difficulties with these.
The more you focus on every tiny detail of your eating experience, the more you’ll imagine something’s wrong.
The time to review your chewing, swallowing and secretion control is when you weren’t thinking about it.
Look back and ask yourself how things went during that dinner with friends when you actually didn’t think about bulbar onset ALS or your tongue. Went pretty smoothly, didn’t it?
Dr. Lafaye says about the bulbar onset progression, “This is subtle and does not occur overnight.
People with ALS have a very distinct speech which is impossible to describe, but it is a combination of spasticity and weakness.
“These individuals need swallowing studies and other diagnostic studies.
“They must have electrodiagnostic studies to assess for denervation in other parts of their body, because they do not have ALS if symptoms are limited to the bulbar muscles.”

Dr. Lafaye is triple board certified: neurology, clinical neurophysiology and neuromuscular medicine from the American Board of Psychiatry and Neurology. Her expertise and leadership continue to make a significant impact on patient outcomes.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/oneinchpunch
Twitching Tongue: When to Worry About ALS
Is your twitching tongue keeping you up all night worrying you might have bulbar onset ALS?
Relax, relax. Don’t let a twitching tongue ruin your life.
Do you realize how exceedingly rare bulbar onset ALS is?
Even if your tongue is twitching all over the place, don’t forget that your tongue is a muscle.
Muscles twitch. That is a fact of nature.
Only about 600 people annually are diagnosed with bulbar onset ALS.
So the odds of your twitching tongue being a symptom of bulbar onset are over 60 times LESS than dying in a car accident!
Thus, examining your twitching tongue for every little distinction, every little groove, indent and twitching, in the name of “could this be bulbar onset ALS?” will prove nothing, really.
And don’t stick your tongue out to inspect for twitching, because the mere act of sticking out the tongue can cause this muscle to twitch!
And forget the side comparisons for size and shape.
“The tongue is a muscle, so like any other muscle one side could be a little larger,” says Kristina Lafaye, MD, a board certified neurologist specializing in clinical neurophysiology and neuromuscular medicine with Tulane Doctors Neurosciences.
Yes, one side could be bigger. Just like one calf or one foot or one bicep can be bigger than the other.
Focus on what your tongue can do, not what it looks like or whether or not it twitches.
Dr. Lafaye explains, “Basically, if the tongue moves normally as characterized by the person speaking, eating, swallowing, and breathing normally, then those are the important points.”
You need to learn how to distinguish between perceived difficulties chewing, swallowing and talking, and actual (or clinical) difficulties performing these functions.
Bulbar onset prevents carrying out these functions without true, actual difficulty.
The “rule of tongue” is this …
If you must concentrate and really focus your mind upon what you are testing for, then there’s no need to think bulbar onset ALS.
On the other hand, if you have bulbar onset ALS, you will not have to scrutinize and hunt for any noticeable problems, because they will be quite obvious.
Deliberately selecting tough-to-chew-and-swallow foods won’t prove anything.
Dr. Lafaye also says, “There can be atrophy of the tongue caused by other conditions (e.g., tumors compressing the hypoglossal nerve), but there would be other signs and symptoms as well.”
And that’s key: other signs and symptoms, and REAL signs and symptoms, not ones that you have to invent through carefully calculated examinations in order to keep your fear alive.

Dr. Lafaye is triple board certified: neurology, clinical neurophysiology and neuromuscular medicine from the American Board of Psychiatry and Neurology. Her expertise and leadership continue to make a significant impact on patient outcomes.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Twitching Calf Muscle: Should You Worry?
Top image: Shutterstock/ANN PATCHANAN
Carpal Tunnel Syndrome Symptoms vs. Impinged Neck Nerve
Did you know that the symptoms of an impinged neck nerve can masquerade as carpal tunnel syndrome?
A doctor might get fooled by this. This happened to my mother.
The doctor who misdiagnosed my mother’s carpal tunnel syndrome for nerve entrapment or impingement in the neck, was an ER doctor whose work badge said “toxicology” on it.
The doctor asked my mother to describe her symptoms, then touched her in various places along the hand and arm, asking what she felt, if she felt it, etc.
The doctor felt around her neck and discovered an extra sensitive spot.
My mother told him she had difficulty turning her head leftward.
After gathering information from her as far as numbness, tingling, pain, etc., the doctor said he suspected a pinched or impinged nerve in the neck.
However, only an MRI would supposedly confirm that, so he ordered an MRI.
A few hours later the doctor returned with the MRI report and said, “It was what I suspected; you have nerve impingement in the neck.”
Interestingly, the doctor said he himself had the same problem.
The doctor appeared to be around 40 and explained he, too, had neck nerve impingement, and described his symptoms, which were identical to my mother’s, but not as extensive as hers, which were as follows:
1) Awakening in middle of the night with arm pain
2) Experiencing numbness in the second and third fingers, and
3) Shoulder pain.
My mother’s symptoms were more pronounced, but the doctor’s symptoms could “fit” inside my mother’s easily.
So when he said she had neck nerve impingement, we didn’t question this diagnosis, even though we were well aware of the idea of carpal tunnel syndrome.
I might add that my mother’s carpal tunnel syndrome was in both hands simultaneously.
The doctor said that a neck nerve impingement could explain why her symptoms were in both hands/arms.
The MRI report revealed narrowing of the spinal canal through which the spinal cord extends; a few bulging disks; degeneration due to age; and some arthritis.
The doctor said the next step was to make an appointment with a neurosurgeon and take it from there.
He said this didn’t necessarily mean she needed surgery; other treatment options were possible, and he himself had seen a neurosurgeon three times and had never been “cut into.”
My mother got an appointment for the following week, but in the meantime, was able to get a sooner appointment with a neurologist to have an EMG test done.
The EMG neurologist immediately suspected pronator teres syndrome after examining her.
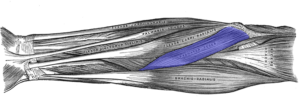
The pronator teres muscle joins the upper arm bone with the two forearm bones.
His secondary diagnosis was carpal tunnel, and he said that her symptoms were not consistent with those of neck nerve impingement!
He said the EMG test would be the only way to tell for sure if the problem was pronator teres syndrome or carpal tunnel syndrome.
Next day was the EMG test: “It’s carpal tunnel,” said the neurologist early into the testing.

The nerves affected by CTS. Source: scientificanimations.com/CreativeCommons
Not only did the EMG test confirm carpal tunnel syndrome, but the EMG test ruled out any pinched nerve in the neck, since the neurologist attached recording electrodes to my mother’s neck.
“Carpal tunnel syndrome and an impinged nerve in the neck can have similar symptoms, which can make it difficult to distinguish between the two conditions,” says Christopher R. Sforzo, MD, head surgeon and founder, Sforzo Dillingham Stewart Orthopedics + Sports Medicine.
“However, one key difference between the two conditions is the location of the symptoms.
“Carpal tunnel syndrome affects the hand and wrist, while an impinged nerve in the neck may affect the neck, shoulders, arms and hands.
“Additionally, carpal tunnel syndrome symptoms are usually more pronounced in the thumb, index and middle fingers, while an impinged nerve in the neck may affect a broader area of the arm.
“A healthcare professional can perform a physical exam, nerve conduction studies and imaging tests to help diagnose the underlying cause of symptoms and develop an appropriate treatment plan.”
If you’re having troubling symptoms (numbness, tingling, weakness, pain) in your fingers, hands, arms and even shoulder, and you’re diagnosed with nerve impingement or pinching at the neck WITHOUT an EMG test to confirm this, you should have an EMG test done.
An EMG exam may reveal that you have carpal tunnel syndrome or even pronator teres syndrome.
And here my mother was … thinking that she might need neck surgery!
 Christopher R. Sforzo, MD, is a board certified orthopedic surgeon, providing treatment of problems involving the shoulder, arm, elbow, forearm, wrist and hand. He performs many procedures using minimally invasive techniques including endoscopic carpal tunnel release, arthroscopic rotator cuff repair, and arthroscopic wrist and elbow procedures.
Christopher R. Sforzo, MD, is a board certified orthopedic surgeon, providing treatment of problems involving the shoulder, arm, elbow, forearm, wrist and hand. He performs many procedures using minimally invasive techniques including endoscopic carpal tunnel release, arthroscopic rotator cuff repair, and arthroscopic wrist and elbow procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sbko
Bulbar Onset ALS vs. Normal Tongue Twitching
Does a twitching tongue have you fearing you might have bulbar onset ALS?
When a person initially becomes aware of tongue twitching, he or she normally has no idea what bulbar onset ALS even is.
The problem arises when the person does an Internet search on tongue twitching, and links to ALS sites come up in the search results.
The individual immediately sees, upon scanning the search results, that a twitching tongue can be a sign of bulbar onset ALS.
Another way this is discovered is when the individual is already aware of muscle twitching being a symptom of ALS, due to having done an Internet search on twitching muscles one day — and seeing ALS links come up in the search results.
They fixate on possibly having this neurological disease, learning about bulbar onset along the way.
Then one day they notice a twitch in their tongue, and so begins a fixation on the bulbar onset version.
If you’ve clicked on this article, then you already know that this motor neuron disease is an incurable, fatal affliction in which muscle twitching is a symptom.
The tongue is a muscle, and, like any other muscle in the body, it can be prone to twitching for benign reasons.
Bulbar onset ALS is an extremely rare condition, afflicting about 10 percent of ALS victims, and this motor neuron disease overall is a rare disease, with about 5,600 cases diagnosed yearly in the U.S. What’s 10 percent of that?
Only about 600 people per year in America are diagnosed with bulbar onset.
If you’ve noticed a twitching tongue lately, it would be quite irrational to jump to the conclusion you might have bulbar onset ALS.
Remember, the tongue is a muscle, and muscles, by nature, are prone to twitching for benign reasons such as fatigue, stress, dehydration and mineral imbalance.
There is far more to bulbar onset ALS than the twitching tongue.
“ALS with bulbar onset is unusual but presents with subtle speech changes and difficulty controlling chewing/swallowing of various consistencies of food,” says Kristina Lafaye, MD, a board certified neurologist specializing in clinical neurophysiology and neuromuscular medicine with Tulane Doctors Neurosciences.
Dr. Lafaye continues, “This is also a gradual process. There is coughing which may prompt consideration of a respiratory condition such as asthma or COPD.
“Unless an individual is having the aforementioned symptoms, then they do not have bulbar onset ALS.”
In short, if you’ve developed the habit of persistently examining your tongue in a mirror, you are wasting valuable time if your only symptom is twitching.
You may be perceiving difficulties chewing and swallowing food, but there is a huge difference between perception and performance.
If the food is getting chewed in a reasonable amount of time, and swallowed without gagging and choking, then you do not have bulbar onset ALS.

Dr. Lafaye is triple board certified: neurology, clinical neurophysiology and neuromuscular medicine from the American Board of Psychiatry and Neurology. Her expertise and leadership continue to make a significant impact on patient outcomes.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Hit Head? Bleeding in Brain Symptoms Can Occur Six Weeks Later

If you hit your head and don’t have immediate symptoms or even symptoms for a few weeks after, you can still develop symptoms of bleeding in the brain at least six weeks later that are the direct result of hitting your head.
Hit your head but everything is fine and you have no symptoms?
Mark the date you hit your head because you can still develop symptoms weeks later – six weeks later, even, from a very slow bleeding in your brain caused by the blunt trauma to your head.
This is what happened to my mother.
She blacked out (from a blood pressure drop) while standing in the bathroom, and collapsed from the loss of consciousness (which lasted only moments, but long enough to turn her body into dead weight) — hitting her head on the bathtub on the way down.
I heard the awful “THUD!” and rushed into the bathroom to see her lying on the floor (conscious), with her shoulders propped up against the side of the bathtub.
There was no way she could have ended up like that without hitting her head.
I examined her head and discovered a generous-sized matting of blood in her hair.
A few hours later in the ER she had a CAT scan that was normal.
The CAT scan was to see if there was bleeding on her brain (subdural hematoma).
Up to that point my mother reported no symptoms, not even a headache.
There was no nausea, dizziness, unsteadiness, slurred speech, vision problems or change in mental status.
She stayed overnight for observation and next morning, another CAT scan was normal.
I expressed concern about the possibility of a very slow bleeding that might start showing symptoms “a few months out.”
But the ER doctor said the chances of this were very tiny, and that the next-morning CAT scan results were very encouraging, and that there probably wouldn’t be any complications — but to keep a close watch on my mother over the next few days.
Over the next few days I kept a close watch: no symptoms, no headache, gait problems, slurred speech, cognitive changes, nothing.
I then completely forget about the idea that her hit on the head could cause any bleeding in the brain.
Until 6.1 weeks later.
The symptoms came out of the blue. She awakened at 7 am with a headache so bad that she was weeping.
It persisted. I did not connect the dots and think of the fall on her head six weeks prior.
I just thought it was one of her bad headaches (every now and then my mother has always reported a bad headache), and that the weeping was just her being overly-sensitive (she’d had quintuple bypass surgery 12 week prior and the recovery had been very bumpy).
The headache was so bad that my mother was unable to get ready for the day.
But I noticed that she had difficulty walking across the room; very weak. Then she upchucked.
Then I noticed her left leg had a slight drag to it.
It still did not occur to me that these symptoms were the result of a slow, delayed brain bleed from hitting her head six weeks ago. Instead, I thought it was a mild stroke.
So did the ER doctor. A CAT scan was ordered and the surprised ER doctor informed us that there was bleeding in the brain.
“Did you hit your head recently?” She asked my mother.
I said she fell about six weeks ago and hit her head on a hard surface.
The diagnosis was a chronic subdural hematoma.
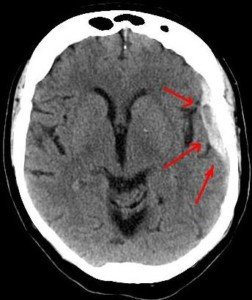
Arrows show the bleeding in a patient with head trauma. Source: Lucien Monfils
And ultimately, the medical reports from two ER visits (this one and another one when the brain bleed recurred after the fluid was drained) named the fall in the bathroom as the cause of the chronic subdural hematoma.
Between the time my mother had hit her head, and the night before she awakened at 7 am with an excruciating headache, she had shown absolutely no symptoms characteristic of bleeding in the brain or head injury!
“Yes, everyone who hits their head traumatically should be evaluated by a physician,” says Danielle DonDiego, DO, a family physician with SteadyMD, an online program where patients can call, text or video chat with their doctor anytime.
“If there is any loss of consciousness, ‘worst headache of their life,’ confusion, feeling faint or vision changes — these are all major signs to go to the ER immediately.
“Even if someone loses consciousness and regains consciousness quickly, they could still have a head bleed that can be deadly. It’s always best to be evaluated,” especially if the individual is elderly, even if initially they don’t seem to have any symptoms and insist “I’m fine.”
Dr. DonDiego continues, “If a CT head is negative initially, especially in the elderly or someone taking blood thinners, and a slow worsening headache persists for days to weeks, it is possible there is a slow bleed, and a re-evaluation is necessary.
“Our veins weaken as we age, so they are likely to be higher risk for hemorrhages.”
If someone hits his or her head, they should record the date.
Any peculiar symptoms that occur even weeks later should be documented.
This includes nausea, vomiting or lingering dizziness.
A normal CAT scan 24 hours after getting hit in the head doesn’t mean that bleeding in the brain won’t eventually occur.
 Dr. DonDiego, who’s also a certified personal trainer, focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
Dr. DonDiego, who’s also a certified personal trainer, focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik
Muscle Twitching Help; Foot Drop Strength Tests & ALS
If you have muscle twitching and have googled twitching muscles, you’ve most likely stumbled upon some links for the deadly disease ALS.
You now might think you have ALS, since muscle twitching is a symptom of the incurable ALS.
But if you read more about ALS, you’ll come upon information that indicates that muscle twitching comes after muscle weakness.
However, you may now suddenly be experiencing what you believe to be weakness in your muscles.
In ALS, one of the first muscles to go is often that which controls foot movement, particularly up and down movement: clinical muscle weakness.
The muscles that control the joint action of dorsiflexion no longer work, and thus, the foot becomes limp.
A person suffering from fear he or she has ALS might start thinking they have this foot drop.
If he stumbles upon bunched-up carpet, right away he’ll think foot drop.
They’ll perform endless strength tests for these muscles to check for the drop, and no matter how well they do these muscle strength tests, they’ll never be assured that they don’t have ALS.
Strength Tests for Foot Drop Obsession and ALS Fear
“If a patient has a foot drop, they would not be able to perform any active exercise, meaning any exercise that can be performed unassisted or that would require resistance such a standing on one’s toes or utilizing a resistance band to stretch out the calf,” explains Dr. Alan L. Bass, DPM, Medical Director of NEMO Capital Partners, LLC.
Using the Foot Pedal While Driving
Yes, as simple as this is, a person with ALS foot drop will not be able to do this efficiently.
This action requires continuous dorsiflexion, the very muscles that, when healthy, prevent foot drop.
Though these muscles don’t work hard to operate the car’s pedal, the continuous use of these muscles is significant.
This test applies only if the person already normally uses the foot on the pedal (depending on driving habits).
Stair Jumping
Stand at bottom of staircase. With both feet at the same time, jump to next step. Land with both feet at the same time. Repeat to the next step. Go all the way to the top.

Shutterstock/G-Stock Studio
This isn’t a fitness test. It’s a “Can I even do this?” test. If you’re clumsy (and you WILL be, due to anxiety of passing this test), this doesn’t matter, because MOST people cannot do this without a little (or even a lot) of clumsiness.
As a fitness trainer I’ve had only a few clients who were able to smoothly hop up a flight of stairs: boing boing boing boing boing.
Other clients were sloppy and uncoordinated. A person with ALS foot drop will NOT be able to what the women in the image above are doing.
Standing on One Foot
Muscles required to do this are the same that prevent foot drop.
If you can stand on one foot, it’s time to stop obsessing about ALS. If you stand on one foot, you’ll feel these muscles at work.

ShutterstockJacob Lund
Expect to lose balance quickly the first several attempts, because anxiety will loom. But keep at it and sooner or later you’ll find yourself balancing nicely.
A person with ALS foot drop will NOT be able to balance and improve, no matter how many times they attempt it.
Stair Running
Run up the stairs as fast as possible, then down. If the muscles that control dorsiflexion are dead, you won’t be able to do this…at all.

Shutterstock/Vadim Martynenko
Seated Ankle Flexion
Have a seat on the floor as shown below. If your “weak” foot can’t flex to match your “good” foot, then there IS a drop problem — but it can have many causes.

Pagemaker787/CreativeCommons
If you can perform all of these routines (regardless of clumsiness or number of attempts required), then you can free yourself of ALS panic, assume your twitching muscles are healthy, and that the foot drop is all in your imagination.
Dr. Bass is with Central Jersey Foot & Ankle Care, and is a Fellow of the American College of Foot and Ankle Orthopedics and Medicine.
basspodiatry.com/our-foot-doctor
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Multiple Sclerosis vs. Sjogren’s Syndrome Symptom Comparison
Sjogren’s syndrome can be misdiagnosed as multiple sclerosis; symptoms are similar.
Sjogren’s syndrome can actually cause symptoms similar to multiple sclerosis (MS).
Sjogren’s syndrome is an autoimmune disease that is commonly associated with dry mouth due to decreased salivary gland secretion, and dry eyes due to decreased lacrimal gland secretion.
However, SS (like multiple sclerosis) can become systemic, affecting many areas of the body, including the nervous system.
As a result, symptoms similar to multiple sclerosis can result from Sjogren’s syndrome.
“Neurological manifestations of Sjogren’s syndrome are protean (considerably variable). Parkinson’s-like is unusual, but MS-like is not uncommon,” explains Ali D. Askari, MD, Professor of Medicine – Case Western Reserve University; Chief, Division of Rheumatology – University Hospitals Case Medical Center; Director, Rheumatology – University Hospitals Case Medical Center. Because SS commonly affects the joints, specialists in this disorder are often rheumatologists.
“In one study 20 percent of patients with what was called primary progressive multiple sclerosis turned out to have Sjogren’s syndrome.”
MRI findings on the brain, says Dr. Askari, can be very similar between Sjogren’s syndrome and multiple sclerosis.
“Other important neurologic manifestations seen in Sjogren’s syndrome include Parkinson’s-like or hemi-Parkinsonism with movement abnormalities including stiffness and tremors.
“Although in Parkinson’s there are not much MRI changes, in Sjogren’s syndrome there are MRI changes of the brain and therefore it could be a very helpful differential diagnosis point.”
And this is because brain lesions are also seen with multiple sclerosis.
“Neurologists are paying careful attention to these possibilities, and in cases of abnormal demyelinating findings on the brain MRI, which looks like cotton balls or smaller, they check the laboratory tests for the presence of antibodies which are commonly seen in lupus or Sjogren’s syndrome.” SS, MS and lupus are all autoimmune diseases.
“We have seen a number of patients with those findings and we have treated most successfully.
“The problem is when the lesions (on the brain) are chronic and they have caused permanent damage to the nervous system and it is difficult to be treated.”
Here is a general symptom comparison between Sjogren’s syndrome and multiple sclerosis.
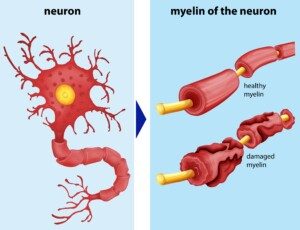
Multiple sclerosis. Freepik/brgfx
Both diseases can present with many more symptoms than in the following list; the list is to show the striking similarities between Sjogren’s syndrome and multiple sclerosis as far as symptoms:
Sjogren’s syndrome symptoms:
Difficulty with chewing, swallowing or talking
Joint pain
Fatigue
Difficulty walking
Tremors
Numbness and tingling
Balance difficulties
Kinesthetic awareness problems (sense of body positioning in space)
Electric shock sensations in the face
Multiple sclerosis symptoms:
Numbness and weakness
Fatigue
Tingling
Pain
Electric shock sensations that arise as a result of particular movements of the head
Unsteady gait
Tremors; difficulty with coordination
Note: Some SS patients do not experience debilitating issues.
For these individuals, the disease is cause for annoyance (e.g., dry eyes and mouth, dental decay), rather than disability.
Update: As of April 2024, Sjogren’s syndrome is now known as Sjogren’s disease.
Dr. Askari’s special interests include diseases of the muscles, fibromyalgia, general rheumatology, lupus and Sjögren’s syndrome.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Lightspring
Sources:
sjogrens.org/home/about-sjogrens-syndrome/symptoms
sjogrensworld.org/sjogrensdefn.htm
mayoclinic.com/health/multiple-sclerosis/DS00188/DSECTION=symptoms
Sudden Onset Dry Mouth Causes & Solutions

Out of nowhere I began developing dry mouth.
What can sudden onset dry mouth mean?
Could it mean the beginnings of Sjogren’s syndrome?
One day during the midst of working out at the gym, I began noticing that I was thirsty.
This might sound normal for someone working out, but for me, it was unusual.
I never crave water while lifting weights, but this time, I seemed to be thirsty and drank water.
I was still “thirsty,” and by the end of the workout, realized that this wasn’t actual thirst.
My mouth was dry. I didn’t think much of it until the day progressed and the dry mouth seemed to be getting worse.
There is an autoimmune disorder called Sjogren’s syndrome, and it’s characterized by a persistently dry mouth.
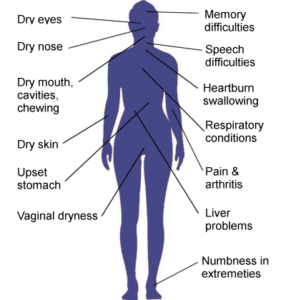
Symptoms that can be caused by Sjogren’s disease.
I wondered if I was developing Sjogren’s, because I already thought I might have a risk factor for it: microscopic colitis.
After being diagnosed with microscopic colitis, I learned that Sjogren’s is associated more with people who have microscopic colitis, though a definite link has not been established.
It’s actually not considered a risk for Sjogren’s, but still, my imagination went a little overboard.
The dry mouth was worse the next day, and the next, especially overnight.
It felt as though there was cotton in my mouth.
Drinking a lot of fluids was not the answer. This was not thirst. It was not dehydration.
Here is how you can tell the difference between dehydration and true dry mouth.
If you’re dehydrated or just plain thirsty, then the thought of a very chilled glass of your favorite thirst-quenching beverage will be extremely enticing.

Freepik.com/Racool_studio
If you have dry mouth, then imagining this tall, cold glass of your favorite drink won’t do anything for you.
I’d envision a tall ice-cold glass of lemonade, orange juice or water … and it did nothing for me; this confirmed (even though I already knew) that I had a mysterious case of really dry, cottony mouth.
My salivary glands weren’t working. I wondered if all four gland stations were being affected, or maybe two or three were.
If I deliberately held off on swallowing, this would allow some saliva to build up, but this didn’t correct the problem.
I also noticed that often, eating made the dry mouth worse, and my lips were also affected. The lips have salivary glands in them.
In Sjogren’s, biopsies of the lip are taken to diagnose for this disease.
On the fourth day I began placing a piece of diced lemon in my mouth to stimulate salivation, and this did a good job of relieving the dryness.

I’d keep the piece in there for a while, and when it was used up, I’d put another one in, and just keep it in there while working at the computer.
Funny thing, while working out at the gym, I noticed that the dry mouth subsided somewhat.
On the fifth day the dry mouth was noticeably suppressed, but I still sucked on a piece of lemon.
By night time there was a noticeable improvement, and on the sixth day, I no longer had dry mouth.
Causes of Sudden Dry Mouth
A sudden development of dry mouth is often caused by “salivary stones,” which are mineral deposits that settle at the salivary gland portal through which saliva is secreted.
But what is the origin?
“Dry mouth occurring in this way is usually the result of a nervous reaction, most commonly with a fit of anxiety,” says Morton Tavel, MD, Clinical Professor Emeritus of Medicine, Indiana University School of Medicine, and author of “Health Tips, Myths, and Tricks: A PHYSICIAN’S ADVICE.”
“I cannot think of any other or serious problems that could account for such a problem,” Dr. Tavel adds.
Often, the crystal-like debris resolves on their own. Other times, dentists must remove them.
One way to force these crystals to get lost is to suck on a piece of lemon.
This stimulates saliva production, and the saliva literally dislodges the crystals and hence, frees up the through-way for saliva, thus resolving the problem of dry mouth.
I took this assessment to my dentist at my next checkup, and she confirmed this process.

Dr. Tavel’s medical research includes over 125 publications, editorials and book reviews in peer-reviewed national medical journals. He was formerly director of the cardiac rehabilitation program at St. Vincent Hospital in Indiana. mortontavel.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/InesBazdar
Could Sudden Dry Mouth Be Sjogren’s Syndrome?

Has your mouth become cottony dry out of the blue, just like that? And is Sjogren’s syndrome constantly on your mind?
Sjogren’s syndrome is an autoimmune disorder that primarily affects the salivary glands and the lacrimal glands (responsible for keeping eyes moist), impairing the glands’ ability to produce fluids.
“Dry manifestations including the eyes and mouth can happen in the absence of Sjogren’s syndrome,” says Ali D. Askari, MD, Professor of Medicine – Case Western Reserve University; Chief, Division of Rheumatology – University Hospitals Case Medical Center ; Director, Rheumatology – University Hospitals Case Medical Center. Sjogren’s syndrome also often causes joint pain.
“There are a variety of other reasons causing dryness of the mouth and enlargement of the parotid glands that includes the stages before the development of Sjogren’s syndrome in total.”
Sjogren’s (pronounced show-grens) syndrome afflicts 2-4 million Americans. Ninety percent of patients are women, for reasons not known.
If you’re wondering if your dry mouth might be Sjogren’s syndrome, first make sure that what you’re experiencing is, indeed, dry mouth.
For first-time sufferers of dry mouth, this sensation can easily be mistaken for thirst or dehydration, especially if it’s mild.
However, an easy way to distinguish dry mouth from thirst (though it’s very possible to coincidentally have both at the same time), is to imagine a tall, chilled glass of your favorite, thirst-quenching beverage.
If this does something for you, you’re probably dehydrated.
If imagining chugging that chilled glass of lemonade, ice tea, soda or iced-up water doesn’t enthrall you, then you likely have dry mouth.
Another hallmark feature of dry mouth, when bad enough, is that it feels like cotton is lining the inner parts of your cheeks.
Plus, drinking large amounts of fluids won’t relieve the dry mouth, but will relieve thirst.
Dr. Askari continues, “In other words, dry mouth could be the first manifestation and one could take it in the context of the presence of other manifestations (of Sjogren’s syndrome) including Raynaud’s phenomenon, arthritis or arthralgia, skin rashes, neurological abnormalities, etc.
“Should all these findings be negative, then dry mouth may be a single problem due to age, dry air, mouth breathing, use of instruments for sleep apnea like what is called CPAP, and history of radiation to the neck and upper chest.”
Hundreds of prescription medications can cause dry mouth, and so can mineral deposits (salivary “stones”) that build up, blocking the secretion portals of the salivary glands. Salivary gland infection is another culprit.
“Furthermore, in somebody with only dry eyes and not Sjogren’s syndrome, the test for antibodies in the blood should be negative.
“These tests include anti-nuclear antibody, rheumatoid factor and specific antibodies of Sjogren’s syndrome including SSA and SSB.”
Update: As of April 2024, Sjogren’s syndrome is now known as Sjogren’s disease.
Dr. Askari’s special interests include diseases of the muscles, fibromyalgia, general rheumatology, lupus and Sjögren’s syndrome.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.








 Dr. Besser
Dr. Besser