Malabsorption Syndrome: Cancer, Other Causes, Symptoms Q & A
Are malabsorption syndrome and cancer necessarily in the same sentence?
- Do you fear you’re suffering from a malabsorption malady?
- Is there a way you can tell at home if you have this gastrointestinal ailment?
If you’ve been having these symptoms, you might think it’s malabsorption syndrome; you may then think, “Thank goodness it’s not cancer.”
However, what might be the cause of the syndrome in the first place?
Cancer is a possible cause, but not a likely cause.
There are numerous causes for malabsorption syndrome other than cancer.
These include bacterial overgrowth in the small intestine; chronic pancreatitis; celiac disease; surgical procedures; parasitic infections; and viral/bacterial infections.
Is a hallmark sign of this ailment oil droplets in the toilet water?
“Oil slicks and droplets are characteristic of patients with very significant and gross fat malabsorption,” says Ned Snyder, MD, Chief of Gastroenterology, Kelsey-Seybold Clinic, Houston, Texas.

“In some types of malabsorption, the primary substance that is not absorbed may not always be fat.”
“For instance, if one has disease of the terminal ileum or a previous surgical resection of this area, then B12 and bile salts will be malabsorbed, and the stool can be normal or liquid after meals, and the patient will be anemic.
“In celiac disease, the fat malabsorption may be modest and the primary presenting problems could be anemia from iron malabsorption or bad bones because of poor absorption of calcium and vitamin D.”
Do stools here have a typical, characteristic appearance?
“It really depends again upon what is malabsorbed,” says Dr. Snyder.
“There are many manifestations of malabsorption, and only a minority of cases have the classic features (stools that are greasy, oily, bulky, foul-smelling).

“In classic fat malabsorption in chronic pancreatitis (or pancreatic cancer), the stools will be light colored, voluminous, float, and be oily.”
“However, all stools that float do not represent malabsorption.
“Also, one can have mild fat malabsorption, and have normal stools.
“If the malabsorption is for carbohydrates or bile salts, the stools can be watery. Protein malabsorption is primarily manifested by muscle wasting, weakness, etc.”
Just how much undigested food will a person typically see in their stools with this condition?
“Undigested food is primarily seen in only the most gross cases of fat malabsorption,” says Dr. Snyder.
Are stools with this condition always loose and diarrhea-like, or can stools be solidly formed?
“If the malabsorption is selective for B12 or iron, the stool can be normal,” says Dr. Snyder.
“However, when fat or bile salts are malabsorbed, the stools will be loose.”
What percentage, if known, of malabsorption syndrome is the result of cancer?
Dr. Snyder explains, “Cancer is a rare cause, except in the elderly when cancer of the pancreas is the etiology of a small percentage of cases.”
(The pancreas is the organ most commonly associated with malabsorption.)
How uncommon is pancreatic cancer in people under 50?
“I can’t provide an exact figure, but pancreatic cancer is highly unusual under the age of 50.
“I suspect approximately 5-8 percent of patients are 50 years of age or younger.
“The mean age is 72, and the incidence of the disease begins to go up sharply in a linear fashion after age 50.”
What is the most common cause of the syndrome in young adults? In middle aged people?
In children? Dr. Snyder says, “Young adults: celiac disease; middle age: celiac disease and chronic pancreatitis; children: cystic fibrosis and celiac disease.”
Celiac disease: The body thinks gluten is an invader and thus mounts an immune response, which over time damages the intestinal lining.
Do the stools float all the time, or can they sometimes sink, with this condition?
“They can sink.” If a person suspects they have this, what should they tell their doctor? “Give a good history including a description of the diarrhea and weight loss, if any,” says Dr. Snyder.
“Gastroenterologists often go straight to colonoscopy with a history of diarrhea.
“Colon diseases can cause diarrhea but not malabsorption, so a colonoscopy will not turn out to be helpful sometimes.
“Patients should ask for evaluations of their small bowel and pancreas.”
What conditions can mimic this ailment?
Dr. Snyder explains, “Common diseases that can present like malabsorption but not usually associated with it include microscopic colitis, Crohn’s disease, ulcerative colitis, infection with giardia, and irritable bowel syndrome.
“Lactose intolerance is common and sort of a malabsorption problem due to a deficiency of the enzyme lactase and should be mentioned as well.”
 Dr. Snyder is a member of the American Gastroenterological Association and the American Society for Gastrointestinal Endoscopy.
Dr. Snyder is a member of the American Gastroenterological Association and the American Society for Gastrointestinal Endoscopy.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Robert Kneschke
Acid Reflux Symptoms Compared to Sinusitis
You think you have acid reflux but you may have sinusitis; or, you’re convinced you have sinusitis but it just might be GERD!
The symptoms of GERD or acid reflux and sinusitis, do indeed overlap, and one condition is often mistaken for the other by sufferers as well as physicians.
“GERD is technically the wrong term; it actually is laryngopharyngeal reflux (LPR),” says Jamie A. Koufman, MD, Director of the Voice Institute of New York and a leading authority on reflux disease.
“GERD refers to reflux into the esophagus, but not all forms of acid reflux disease.
“When the air passages are involved, medical specialists usually call it LPR, also often called silent reflux.”
So if you want to know how to tell GERD symptoms from sinusitis, the better question is:
How do laryngopharyngeal reflux symptoms compare to those of sinusitis?
Dr. Koufman explains, “Reflux can cause post-nasal drip and too much throat mucus, as can sinusitis; but more importantly, reflux can actually be the cause of sinusitis.
“LPR is called ‘silent reflux’ because the reflux can occur during the night; and when this occurs, the stomach contents (enzymes and acid) actually make it all the way up into the back of the nose, where they can cause problems with the sinuses.”

Shutterstock/Elen Bushe
Can a person have LPR and sinusitis, but with both conditions independent of each other, rather than one causing the other?
Dr. Koufman explains, “A person can have both conditions.
“However, reflux is more likely to cause sinus disease than sinus disease to cause reflux.
“As doctors become more aware that reflux can cause disease anywhere in the airway, including the sinuses, more people will receive treatment, which can prevent sinusitis.
“In other words, many reflux patients on long-tern anti-reflux treatment report that their sinus troubles vanish, too.”
How often is GERD misdiagnosed as sinusitis?
“LPR/GERD is often misdiagnosed as sinusitis, simply because of the post-nasal drip,” says Dr. Koufman.
“Too much throat mucus is one of the most common symptoms of LPR.”
What is the function of mucus? It creates a protective barrier for the nasal membranes, as well as the membranes that line the throat.
“When irritation is present from reflux, generally more mucus is produced, almost as if the body was trying to better protect itself,” says Dr. Koufman.
About half of Dr. Koufman’s patients, who have been diagnosed with sinus disease by other doctors, don’t have sinusitis.
She adds, “Unfortunately, sometimes I see such patients after they’ve had unsuccessful and ineffective sinus surgery.”
Why is GERD so often misdiagnosed as sinusitis?
“Reflux is misdiagnosed as sinusitis, even when special X-rays are obtained,” says Dr. Koufman.
“Thick lining inside the sinuses is actually not ‘sinusitis,’ but can be associated with reflux or even allergies.
“True sinusitis will show complete opacification of the sinus or even an air-fluid level.” Opacification means non-transparency.
The truth is, continues Dr. Koufman, that “many physicians assume that nasal/sinus symptoms are due to sinusitis simply because they are still unaware of silent reflux.
“After all, if a person doesn’t have heartburn or indigestion, it’s easy (easier) to overlook the diagnosis of LPR.”
So how is a diagnosis of LPR made?
One must make an appointment with an ENT (ear, nose and throat) doctor for a complete throat and nose exam.
Dr. Koufman adds that there is now a special test called pharyngeal pH-monitoring that detects acid in the upper area of the throat.
If you have symptoms that seem to be GERD or sinusitis, don’t try to self-diagnose; make an appointment with an ENT physician.
 Dr. Koufman has lectured nationally and internationally and is one of the world’s leading authorities on reflux. For 25+ years her pioneering research has focused upon acid reflux as it affects the voice and airway.
Dr. Koufman has lectured nationally and internationally and is one of the world’s leading authorities on reflux. For 25+ years her pioneering research has focused upon acid reflux as it affects the voice and airway.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
Source: refluxcookbook.com/authors
IBS (Irritable Bowel Syndrome) Stools vs. Malabsorption BM’s

Malabsorption that results in odd-looking stools can have a variety of causes, and IBS (irritable bowel syndrome) can also cause stools to appear less-than-normal.
You may be wondering if there was a way to distinguish between IBS and malabsorption stools.
“I do not think there is any good way to tell apart the stools of someone who just has IBS from other malabsorption conditions like celiac disease, cystic fibrosis, or even inflammatory bowel disease,” explains Pejman Katiraei, DO, FAAP, an integrative physician whose many areas of specialty include adult and pediatric IBS.
Cystic fibrosis is an inherited genetic disorder that primarily affects the lungs.
Other causes of malabsorption include lactose intolerance, soy milk intolerance, bacterial overgrowth, microscopic colitis, Crohn’s disease, surgical procedures, infections, medications and pancreatic cancer.
If you’re experiencing malabsorption, chances are that your stools will be extremely foul-smelling.
However, very foul-smelling stools don’t mean you have malabsorption, and the absence of a foul odor doesn’t automatically rule out malabsorption, either.
Dr. Katiraei continues, “Any of these conditions can show up in all kinds of different ways. As such, in my opinion it is never a good idea to make a diagnosis based on how stools look.
“You have to look at the whole picture (Is the person having fevers? Are they losing weight?).”
Malabsorption often causes weight loss and other symptoms such as cramping, bloating, gas and muscle-wasting.
However, the absence of these other symptoms does not rule out malabsorption.
Dr. Katiraei continues, “Once this information is combined with lab testing and even an endoscopy by a gastroenterologist, then you can safely say that it is IBS or not.
“In my opinion, it is dangerous for any person to make a guess as to what condition they have based on the appearance of their stool.”
What you can do, however, is get familiar with the caliber of your stools.
Most people will not look at, much less closely examine, their stools, as they think this is “gross.”
Rest assured, you can actually get used to viewing what plops into the toilet bowl water.
I certainly did after I developed microscopic colitis.
My stools took on all sorts of funny shapes and textures, including bulky, oily looking, foul smelling, with lots of undigested food intertwined in them.
Sometimes my poops floated, and they had lost their normal milk-chocolate color and were a spectrum of tans, often with a greenish tinge.
Sometimes they’d promptly disperse in the water if I poked them with a cotton swab, and they were never fully formed, meaning, they were what I called semi-diarrhea.
Nevertheless, it turned out that I did not have malabsorption, in that the gastroenterologist who performed my colonoscopy looked at the stool samples in a jar that I brought into the exam room, and he said I did not have malabsorption.
He drew that conclusion by looking at my BMs, but there are fecal-sample lab tests that can determine if you have malabsorption.
If you’re familiar with what your stools should look like when everything is in balance within your body, then you will definitely know when something doesn’t look right.
If you have IBS, get to know how IBS affects the appearance of your stools.
You can’t diagnose by looking inside the toilet bowl, but what you see inside the toilet bowl is enough information to determine whether or not to see a gastroenterologist.
Dr. Katiraei created Wholistic Kids and Families for people interested in learning how to raise a healthy child (and future adult) in a world that’s becoming increasingly polluted with toxins (chemical and emotional).
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Sofi photo
Sources: Merckmanuals.com; .nlm.nih.gov/medlineplus/ency/article/000299.htm
Does IBS Usually Cause Thin Narrow Poops?
Do narrow stools have you fearful of colon cancer, even though you’ve been diagnosed with irritable bowel syndrome (IBS)?
If narrow or thin stools are common with IBS, then this may certainly provide more peace of mind in the person already diagnosed with this aggravating condition.
“Narrow stools can be common with IBS, and they may be very difficult to differentiate from colon cancer,” says Pejman Katiraei, DO, FAAP, an integrative physician whose many areas of specialty include adult and pediatric IBS.
“Depending on what is happening to a person’s gastrointestinal tract, a person suffering from IBS can have everything from severe constipation to watery diarrhea.
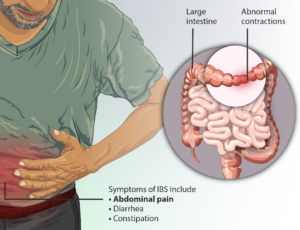
Irritable Bowel Syndrome. Source: myupchar.comen
“As such, there is no specific type of stool that would allow a person to know they have IBS over deadly conditions like the early stages of inflammatory bowel disease or even colon cancer.”
If you’ve already been diagnosed with irritable bowel syndrome (and the diagnosis should have been made after an entire battery of tests ruled out other possible causes of your GI distress such as colon cancer), then you can conclude that the presence of narrow or skinny stools is most likely a part of having irritable bowel syndrome.
However, Dr. Katiraei adds, “I would strongly encourage people suffering from gastrointestinal problems to be evaluated by a medical professional.
“Simple blood and stool testing can give important information that can be life-saving.”
So assuming, then, you’ve already been cleared of colon cancer, and have been diagnosed with irritable bowel syndrome, there is one critical element you must never forget:
Just because you’ve been diagnosed with irritable bowel syndrome, doesn’t mean that you’ll never get colon cancer!
A person with irritable bowel syndrome can still develop colon cancer, so get to know your IBS presentations very carefully and meticulously.
After all, the symptoms of irritable bowel syndrome and colon cancer strongly overlap and are virtually identical.
Have your apparent IBS symptoms changed lately?
Have you always had narrow stools, or are narrow stools only a recent occurrence after having irritable bowel syndrome for years?
Is there suddenly blood in your stools?
Have you had IBS for years, and are now suddenly losing weight for no reason?
Unexplained weight loss can also mean diabetes or overactive thyroid; get a thorough medical exam.
Do you have any other new symptoms that don’t seem to fit the bill for irritable bowel syndrome?
If you’re in doubt, then get another evaluation by your doctor.
Don’t assume you can’t have colon cancer because you have IBS.
Irritable bowel syndrome cannot morph into colon cancer, but a benign and malignant disease of the GI tract can exist simultaneously in the same person.
Dr. Katiraei created Wholistic Kids and Families for people interested in learning how to raise a healthy child (and future adult) in a world that’s becoming increasingly polluted with toxins (chemical and emotional).
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Causes & Treatments for Irritable Bowel Back Pain

Irritable bowel syndrome (IBS) can cause back pain.
If you have back pain that has not responded to massage or other typical treatments, you may actually have IBS.
First of all, how does IBS even cause back pain in the first place?
Dr. Pejman Katiraei explains that he had a female patient in her 50s who suffered from back pain, along with other symptoms including chronic fatigue, allergies and migraines.
“Since other treatments were not working, she decided to go on a specialized water fast for three days,” says Dr. Katiraei, DO, FAAP, an integrative physician whose many areas of specialty include adult and pediatric IBS.
“Within two days, her back pain, muscle pain, allergies, and even hot flashes were gone.”
Was there a connection between the absence of food and the disappearance of the pain and other symptoms?
“To understand why this patient got better, we need to understand her IBS was tied to her back pain and all her other symptoms.
“I believe there is now ample evidence to show that people with IBS have inflammation or increased immune activity in their intestines. This inflammation is the reason for pain, diarrhea and most other symptoms.”
Think of the body as a whole unit, such that everything is connected; inflammation in one area of the body can cause a ripple effect: inflammation in another area … including the spinal area.
Eliminate inflammation in the intestines, and you will also eliminate inflammation in the back, says Dr. Katiraei.
How does the gut have anything to do with the back?
Nerves from the intestines go to the spinal cord.
“These nerves are also indirectly connected to the tissue in parts of our back. The inflammation in the intestines also irritates these nerves, which then causes irritation at the level of the tissue (skin) in the connected areas on the back.”
Massage therapists, chiropractors and osteopaths, who heal patients with their hands, can detect tissue change as a response to inflammation.
“So you may go to your chiropractor for back pain, and they may be astute enough to tell you that the pain is not from your back, but rather from your intestines,” says Dr. Katiraei.
This phenomenon also works in reverse. A problem with one’s back can cause intestinal issues.
“There are nerves that go from the spinal cord into the intestines. Some people who have back pain and some intestinal problems actually have some vertebrae that are out of place and impinging on the nerves, causing the nerves not to work perfectly, which then disrupts the signals to the intestines, causing the intestines to not work perfectly.
“The back pain may be due to these bones being out of place. So, sometimes a good adjustment by a chiropractor or osteopath can relieve a person’s back pain and subsequently the abdominal pain.”
Does this all sound confusing?
Dr. Katiraei confirms that this all, indeed, is complicated, and therein lies the problem … the problem a person with IBS has when it comes to finding a treatment that truly works.
“People are looking for a one-size-fits all solution, and it simply does not exist,” says Dr. Katiraei in reference to irritable bowel syndrome.
“When treatments for IBS are tailored to each person, it becomes very possible to effectively treat and perhaps even cure IBS!”
Dr. Katiraei created Wholistic Kids and Families for people interested in learning how to raise a healthy child (and future adult) in a world that’s becoming increasingly polluted with toxins (chemical and emotional).
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Leg Pain Caused by Irritable Bowel Syndrome

Leg pain can have a ton of causes ranging from so very benign to life threatening–and one of those possible causes is irritable bowel syndrome.
Having pain in your leg and wondering if this is related to your irritable bowel syndrome?
Your one burning question is: “Can IBS cause leg pain?”
“Yes! The underpinnings of IBS are fascinating, and this underpinning helps explain the leg pain,” says Pejman Katiraei, DO, FAAP, an integrative physician whose many areas of specialty include adult and pediatric IBS.
“To start, we must recognize that people with IBS have inflammation in their intestines. Inflammation means that there is increased immune activity in a part of the body.”
An example of this would be the redness that occurs around a cut in your skin, or the swelling of a sprained ankle.
“People with IBS have inflammation in their intestines,” continues Dr. Katiraei.
“This inflammation typically involves a specific type of immune cell called mast cells.”
A doctor may give an endoscopy to a person with IBS, but tell that patient that all is normal … because pathologists are not able to see the mast cells via standard biopsy analysis.
The problem is there, says Dr. Katiraei, but it goes unseen. This is why people with IBS are often told that nothing is wrong.
But Dr. Katiraei continues, “If doctors used very sensitive tools like electron microscopes or very specialized immune stains, they will find these changes in the intestines.
“In the bowel, sitting right next to these mast cells are nerve cells that take information from the intestines to the spinal cord.”
During an inflammatory process, the mast cells release chemicals that can irritate nerve cells.
“The irritated nerve cells then send signals to the spinal cord that there is something very wrong,” says Dr. Katiraei.
“Our brain interprets this signal as pain. It so happens that the nerves from the legs merge in the spinal cord in the same area as the intestines. The signal from the gut and the legs gets mixed up.”
This is called viscerosomatic convergence and it tricks the brain.
“The pain signal from the intestines gets mixed up as a pain signal from the legs.”
So indeed, a person with IBS can definitely experience a perception of pain in the legs. The leg pain here is actually from the intestines.
Dr. Katiraei adds, “When the inflammation in the intestines calms down, so does the inflammation in the joints, and the pain disappears.”
Dr. Katiraei created Wholistic Kids and Families for people interested in learning how to raise a healthy child (and future adult) in a world that’s becoming increasingly polluted with toxins (chemical and emotional).
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Does Colon Cancer Always Cause Abdominal Pain?

Colon cancer can cause abdominal pain, but does it always?
When I say “pain,” I don’t mean cramps.
There’s a difference between abdominal pain and abdominal cramps. Abdominal pain can result from colon cancer.
But have you wondered, however, if in every case of colon cancer that’s gone untreated long enough to produce symptoms, if abdominal pain is always one of the resulting symptoms?
“Remember, for polyps and early cancers, the hallmark symptom is the absence of symptoms — this is why getting screened at age recommendations while asymptomatic is so important,” explains gastroenterologist Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
A person can “feel fine” yet have colon cancer.
A colonoscopy can detect this disease early, long before it invades surrounding tissue and causes symptoms (such as abdominal pain).

Freepik.com
Dr. Jones explains, “Abdominal pain is one of the many hallmark symptoms and presents usually when there is advanced disease including obstruction, perforation or spread into adjacent organs.
“It can be the initial presenting symptom of large polyps or early cancers.”
Because symptoms of numerous benign conditions can mimic those of colon cancer, it’s important to get colonoscopy screenings beginning at age 45 if you are of average risk for this disease.
To determine if you’re at average risk or increased risk, you need to consult with a physician.
A key risk factor for this disease is having a parent or sibling who had/has the condition.
Pain in the belly is one of the most common ailments of the human body.
Thus, if you’ve been experiencing abdominal pain lately, don’t jangle your nerves by jumping to the conclusion that this must mean colon cancer, even if you are over age 45.
It’s more likely to be from any number of benign conditions.
However, does the abdominal pain from colon cancer feel different from stomach discomfort caused by benign conditions?
Dr. Jones says, “Not really. This is why any unexplained abdominal symptoms should be fully evaluated and if unresolved, colonoscopy should be a consideration once evaluated by a health care professional.
“Symptoms overlap greatly between all of the different GI problems and this includes colon cancer.
“Only a thorough exam can tell the difference and thank goodness, most of the times the cause will not be colon cancer.”
There are literally reams of causes of abdominal pain not related to colon cancer.
However, some non-malignant causes of stomach pain are of a very serious nature, such as appendicitis, a ruptured spleen and a ruptured ovarian cyst — all of which are life-threatening if not promptly treated.
In addition to abdominal pain, Dr. Jones adds the following for colon cancer symptoms:
“Change in bowel habits, rectal bleeding or blood on the tissue (paper), change in stool caliber, fatigue either from anemia or from advanced colon cancer, weight loss, nausea/vomiting from obstructions, anemia, jaundice from metastatic colon cancer to the liver or the bile duct.”
 Dr. Jones’practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
Dr. Jones’practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/George Rudy
Can Diarrhea Be the Only Symptom of Colon Cancer?

Is it possible for diarrhea to be the only symptom of colon cancer?
You may be familiar with colon cancer’s classic signs such as abdominal pain, weakness, weight loss, blood in stools and ribbon-like stools — and diarrhea and/or constipation.
I wondered, however, if colon cancer can cause just the symptom of diarrhea.
I posed this question to gastroenterologist Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
Dr. Jones says: “Yes, diarrhea alone can be a symptom, particularly if this is a new and persistent change in habits.
“Tumors in the lower colon or rectum cause a partial obstruction of the bowel, which compensates by liquefying the stool to get stool past any narrowed portion.”
The tricky thing about this is that diarrhea is a symptom of tons of medical conditions, most of them benign.
This symptom is so common that you can’t watch prime time TV without seeing a diarrhea commercial.
Millions of people have suffered a sudden onset or gradual onset of diarrhea without knowing the cause, at least initially.
I then asked Dr. Jones if there’s a bowel obstruction, can we assume that once the obstruction starts creating enough blockage to cause diarrhea, that there will be “no going back” to formed stools?
Or can the tumor sometimes shift position and thus result in normal stools?
He responds, “The process, like irritable bowel syndrome, can wax and wane in the short-run (i.e., 1-2 weeks), but in general does not just stop and reverse to normal.
“It will usually be unremitting and eventually leads to obstruction if not diagnosed sooner.”
When having even a routine colonoscopy, if you’ve been enduring diarrhea lately, make sure your physician knows about this.
This way, the endoscopist can collect tissue samples of your colon for microscopic analysis to see if an inflammatory condition is responsible for your symptoms.
For example, ongoing diarrhea for no apparent reason can be caused by microscopic colitis.
Dr. Jones explains, “The time to be screened for colon cancer is while you are asymptomatic. Otherwise, it is not a screening test; it is a diagnostic test.
“When you do have a GI problem (as we all will ), if you had been screened, you are much less likely to have the cause of your issue be colon cancer.”
 Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/daizuoxin
sscpywrt26
IBS vs. Microscopic Colitis: Similarities, Diagnosis

IBS (irritable bowel syndrome) and microscopic colitis produce symptoms that are similar enough to result in misdiagnosis.
So do you have IBS (irritable bowel syndrome) or microscopic colitis?
After all, the symptoms overlap. Furthermore, symptoms of microscopic colitis can vary greatly from patient to patient.
I should know; I had a bout with microscopic colitis, yet compared to the symptom descriptions of people posting on a microscopic colitis forum, my symptoms were quite mild.
“Microscopic colitis generates diarrhea which is for the most part continuous,” says Matthew M. Eves, MD, F.A.C.G., a gastroenterologist in Alabama.
“It is not necessarily associated with abdominal pain. Irritable bowel syndrome by the Rome criteria is defined as abdominal pain associated with a change in bowel habits.
“The diarrhea with IBS does not have the volume microscopic colitis does.
“Unfortunately, many physicians do not adhere to the strict definitions of irritable bowel syndrome and because of that, microscopic colitis has a tendency to be misdiagnosed as IBS.”
Microscopic colitis is more likely to be misdiagnosed as irritable bowel syndrome, than the other way around, and this mix-up is actually rare.
Microscopic colitis can only be properly diagnosed (and definitively at that) with random large-colon tissue biopsies via colonoscopy, which are then examined under a microscope.
“There are, however, several primary care physicians who will listen to the clinical symptoms and diagnose IBS based on that,” says Dr. Eves.
“Because many physicians see IBS as a diagnosis of exclusion, if the workup is not complete, the door is left open for missing microscopic colitis.”
Rome criteria are used to definitively diagnose irritable bowel syndrome.
“Basically you have to have a change in bowel pattern associated with abdominal pain.
“Some would argue that a diagnosis of IBS could be made if these criteria are rigidly applied.
“This is done to establish IBS as a more legitimate diagnosis even though there is no test to confirm its presence.”
Dr. Eves continues: “IBS that meets the Rome criteria is but a small part of a larger spectrum of disorders.
“So by using the criteria you would improve diagnostic accuracy of the single entity of IBS, but miss other disorders of the enteric nervous system commonly called functional disorders.”
Dr. Eves adds that most non-GI physicians view irritable bowel syndrome and functional disorders as one and the same.
And from a practical point, they are indeed synonymous, says Dr. Eves.
“The patient has abdominal pain and usually some bowel symptoms or bloating and wants relief.
“Whether it meets the definition of IBS or not, I still treat with antispasmodics, cathartics, anti-diarrhea agents and antidepressants primarily.
“I keep changing the mix until I get the patient to a point where the impact of the symptoms is minimized.
“It is frustrating because I’m not fixing the problem. In fact, we don’t even really know what the problem is.”
If this sounds like a mess to sift through, it is. To avoid it, the patient must have a colonoscopy to test for microscopic colitis.
The treatment for microscopic colitis differs from treatment for irritable bowel syndrome.
“If a patient presents with diarrhea for more than four weeks, they ought to have a colonoscopy.
“There is no getting around it. Ulcerative colitis and Crohn’s disease could be missed as well.
“Unfortunately, the physician must recognize the possibility of microscopic colitis.
“If he does not he will lump them in with IBS patients. That is why chronic diarrhea, which is a complex illness, ought to be worked up by a gastroenterologist. Unlike acute diarrhea, it will not go away on its own.”
 With more than 20 years of diverse experience, Dr. Eves cooperates with other doctors and physicians in medical groups including Imc-Gulf Coast Gastroenterology PC.
With more than 20 years of diverse experience, Dr. Eves cooperates with other doctors and physicians in medical groups including Imc-Gulf Coast Gastroenterology PC.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, nikitabuida
Source: perskyfarms.com/phpBB2/index.php
Brain Tumor Headache: What Are False Alarm Symptoms?
Does your very bad headache have you fearing you have a brain tumor? Does the pain make you think it could only be from a brain tumor?
Though the only way to rule out a tumor is with a scan of your brain, this doesn’t mean that a really bad headache is most likely cancer.
There are a number of causes for a really severe headache other than cancer or a ruptured aneurysm.
Sinus headaches have been known to trigger significant head pain.
Anyone with migraine disorder knows that this can bring on a searing headache.
But there’s yet another condition that can cause a really intense headache — plus additional symptoms that can make the sufferer become terrified that it’s a brain tumor.
The condition is called intracranial hypotension syndrome.
Intracranial Hyptension Syndrome
“Intracranial hypotension results from a cerebral spinal fluid (CSF) leak,” says Sumeer Sathi, MD, a neurosurgeon with NYU Langone Health, who treats brain tumors.
“This leak causes a decreased amount of CSF that bathes the brain and spinal cord.
“CSF leaks can be from a leak in the spinal canal (i.e., spinal tap), defects in the spinal tube, and ventricular shunt malfunctions.
“Intracranial hypotension can cause a syndrome that presents in a variety of symptoms.
“The most typical symptom is called a positional headache; the headache tends to worsen in an upright position and improves while lying flat.
“Other symptoms can include nausea, vomiting, vertigo, tinnitus, fatigue and neck pain.
“Onset of symptoms can be abrupt or gradual depending on the cause.”
Digging Deaper into IHS
A study was published in Neurology in which 11 people with incapacitating headaches were found to have enlarged pituitary glands (the gland is in the brain).
Their headache symptoms were those of intracranial hypotension syndrome.
However, intracranial hypotension, at least in the study subjects, had a variety of etiologies, such as unexplained fluid loss, spontaneous occurrence, cervical spine surgery and lumbar puncture via spinal tap.
The headaches were accompanied by nausea, neck pain, visual and hearing problems, and even facial numbness.
As you can see, IHS produces symptoms that very much mimic those of a brain tumor.
Enlarged Pituitary Gland
The researchers believe that the sinuses, that surround the gland, accommodate the low fluid pressure.
They do this by becoming engorged…with blood. This doesn’t make the diagnosis easy.
However, the study results could prevent some people from getting mistakenly thought to have a brain tumor, when they really have intracranial hypotension syndrome.
According to MRI exams, the pituitary glands were 50 percent larger, on average, than normal.
IHS Treatment
“Treatment is aimed at correcting the defect/hole in the dura mater that holds the CSF,” says Dr. Sathi.
When surgery is not required to repair the leak, treatments may consist of bed rest, hydration and corticosteroids.
 Dr. Sathi’s expertise includes spine surgery and treating brain tumors including metastasis, gliomas, meningiomas and acoustic neuromas using gamma knife radiosurgery.
Dr. Sathi’s expertise includes spine surgery and treating brain tumors including metastasis, gliomas, meningiomas and acoustic neuromas using gamma knife radiosurgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.