Low Thyroid May Be Causing Your Clinical Depression
One cause of depression can be a thyroid problem: more specifically, an underactive thyroid, also known as hypothyroidism.
Yes, you read that right: hypothyroidism can lead to clinical depression.
The disease of hypothyroidism, when the thyroid is underactive, is commonly associated with weight gain or difficulty losing extra weight.
This component of low thyroid gets so much attention that the component of depression gets buried.
But clinical depression is one of numerous possible outcomes of a malfunctioning thyroid.
“When the body doesn’t create enough triiodothyronine (T3) or thyroxin (T4), it causes your thyroid stimulating hormone (TSH) to rise,” says Walter Gaman, MD, FABFM, board certified in family medicine and the author of several award-winning books including “Age to Perfection: How to Thrive to 100, Happy, Healthy, and Wise.”
“The body then experiences symptoms of depression, such as fatigue, loss of ambition, trouble concentrating and generalized feelings of sadness.
“Many doctors may immediately test your thyroid when you complain of these symptoms, while others will assume it is clinical depression without a primary source. This is why some patients do not respond to antidepressants.
“The flipside of this is that people with hypothyroidism may also develop clinical depression that has actually altered the brain chemistry.”
If you have symptoms of depression or know someone who is showing signs of depression, don’t blow off the possibility that an underactive thyroid can be the underlying cause.
A blood test will determine if the thyroid is working properly.
This doesn’t mean that most people with feelings of hopelessness and despair, lethargy, fatigue and loss of appetite have hypothyroidism.
But every person with depression should have a complete physical workup to see if thyroid hormone levels are normal.
Besides depression, classic symptoms of hypothyroidism include:
- Often feeling cold even though the temperature is normal and everyone else in the room feels fine
- Hair loss that doesn’t seem in alignment with male pattern baldness or aging
- Hoarse voice
- Fatigue and lethargy
- Excessive sleepiness and wanting to sleep all the time
- Moderate weight gain (though not all people with hypothyroidism will gain weight, especially if depression is killing their appetite
- Constipation; and tingling in the hands and fingers.
A patient will not necessarily have every symptom listed here, and may only have a few at the time of diagnosis.
It’s interesting to note that sometimes, depression is the first clue that a person’s thyroid is not producing enough hormones.
“The thyroid medication alone may not be enough to reverse the symptoms, and an antidepressant may be necessary in the short run,” says Dr. Gaman.

Dr. Gaman is with Executive Medicine of Texas and is with the Staying Young Radio Show 2.0 podcast.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Steroid Psychosis from Medrol DosePak: Yes, It Happens
Medrol can cause very nasty side effects like psychosis — called steroid psychosis.
And it’s not uncommon for ER physicians to see this.
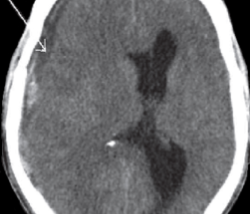
My mother’s neurosurgeon said “one percent,” and then “half of one percent,” while in the surgery prep area where mother was being prepped for evacuation of a chronic subdural hematoma.
This was a recurrence of the chronic subdural hematoma, and the neurosurgeon had prescribed the Medrol Dosepak.
He never mentioned the possibility of mental side effects, though the insert mentioned them. He did mention, however, that constipation could result.
Several hours after taking her first Medrol tablets, my mother became a raving, delirious stranger, highly agitated, and had lost all rational thought processes.
My father asked if this could be a side effect of the steroid, and I said, “No, steroids don’t cause these kinds of side effects.”
I thought that the ranting, bouts of crying, complaints of being unable to breathe, and general delirium, were from a recurrence of the chronic subdural hematoma, with some panic attack mixed in (my mother has a history of panic attacks).
After all, she had already been experiencing two other symptoms that were obviously from a recurrence (and later confirmed via CAT scan) of the chronic subdural hematoma: searing headaches that increased in frequency, and deterioration of fine motor control in her left hand.
So my mind, then, was locked on the conclusion that the rapid-onset madness was yet another symptom of a recurring chronic subdural hematoma.
In the ER, the doctor suspected steroid psychosis from the Medrol, but couldn’t rule out a recurrence of the chronic subdural hematoma until the CAT scan results were in.
The CAT scan showed nothing that could explain such behavior, and the doctor diagnosed her with a bad reaction to the Medrol, known as steroid psychosis.
Steroid psychosis is not the same as “roid rage.”
There are two kinds of steroids: anabolic and catabolic.
Anabolic steroids are what athletes use, to build muscle (anabolism). Corticosteroid drugs, used to control or bring down inflammation, are catabolic (promote muscle breakdown), and often cause fat gain.
The ER doctor said she sees steroid psychosis often, but also said it’s not common.
The neurosurgeon, of course, said that steroid psychosis occurs in one percent, and one-half of a percent, in patients.
Interestingly, my mother tolerates Cymbalta and Effexor beautifully, and antidepressants are notorious for causing a myriad of intolerable side effects, but for my mother, Medrol was a horrible drug.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Can Cymbalta’s Discontinuation Syndrome Be Prevented?
What a shame that the drug companies can’t make an antidepressant like Cymbalta that doesn’t have a discontinuation syndrome, but there’s hope if you want to get off this drug and similar ones.
Antidepressants like Cymbalta, Effexor and Paxil may very well have the worst discontinuation syndromes, even when these drugs are tapered off gradually.
The problem is magnified when people quit Cymbalta and other antidepressants cold turkey, or, they don’t taper off Cymbalta, etc., gradually enough.
I asked an expert if there was a way to prevent discontinuation syndrome from Cymbalta and similar antidepressants: Joe Wegmann, psychopharmacologist and licensed clinical social worker, author of Psychopharmacology: Straight Talk on Mental Health Medications.
“There really is no way to eliminate discontinuation syndrome with Cymbalta,” says Wegmann. “After 4-5 weeks of use, anywhere from 35 to 75 percent of Cymbalta users will experience withdrawal symptoms upon discontinuation.
“The withdrawal symptoms associated with this drug range from mild in some people to moderately severe in others.
“The length of the withdrawal process tends to be dose-dependent – that is, the higher the dose, the longer it takes the discontinuation symptoms to abate.”
A person who’s been on Cymbalta for a while may feel so good, that he or she might then start believing they don’t need the antidepressant any longer.
But the reason they’ve been feeling so normal and motivated is because Cymbalta has been working on their brain chemistry; go off it, and chances are, the symptoms of depression will return.
Depending on a person’s grade of depression, it may be best to keep using Cymbalta or similar antidepressants until an outright, one-dose-pill cure for depression is discovered.
Wegmann continues: “The onset and severity of the discontinuation syndrome with antidepressants is linked to their half-lives – the amount of time, on average that it takes for 50 percent of the antidepressant’s active ingredient to be eliminated from the body from peak plasma levels.
“The short-half life antidepressants – Paxil, Zoloft, Effexor, Cymbalta – tend to produce the worst discontinuation syndromes.
“Prozac however, because of its long half-life (seven days), tends to produce very little, if any, discontinuation symptoms at all.”
I’m an “anti-drug” person, in that I believe that rather than rely upon drugs, people should practice natural, holistic ways of living to be strong and feel uplifted; that pills and capsules are not the answer; that feeling depressed is part of being human.
However, depression can also render a person bedridden — and then what?
Or, if they’re out of bed, they are frequently crying, refuse to eat, and do little more than sit in a chair and stare into space, worry, have panic attacks, and frequently complain about physical pains.
You can’t get somebody like this to exercise, take a brisk walk on a mountain trail, attend cognitive behavioral therapy, or eat lots of natural foods when it’s a battle just to get them to take a few bites of toast — as with what had happened with my mother when she developed severe clinical depression.
In that case, antidepressant intervention is necessary, when all else has failed, and the depression will not go away on its own.
Cymbalta is recommended for depressed people whose illness also creates physical pain.
In some people, this drug works wonders, but doggone it, this drug, along with Effexor, Paxil and Zoloft, are cursed with discontinuation syndrome.
Wegmann explains: “Tapering is dependent on the milligram strengths in which an antidepressant is available. In my experience, regardless of the antidepressant, anyone should be able to discontinue without severe withdrawal symptoms over a period of three months.
“There is a tendency for people to commiserate on these blogs (about their horrible discontinuation syndrome experiences with Cymbalta, Effexor, etc.).
“Many are quitting cold turkey and not admitting it. Others are likely taking multiple medications, some of them psychotropics, which are affecting the discontinuation process.
“Unmentioned physical illnesses and substance abuse may also be contributors. Bottom line: Severe discontinuation syndrome is avoidable with slow, steady tapering.”
 Joseph Wegmannis a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
Joseph Wegmannis a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
What to Do if You Gained Weight from an Antidepressant
Antidepressant weight gain happens, but there are ways to fight back.
Here are solutions to weight gain from antidepressants.
There are two types of weight gain from antidepressants.
It’s the second type that can have many people up in arms; after all, an antidepressant is supposed to help you gain back a positive mood, not weight.
It’s no secret that antidepressants can cause certain individuals to put on weight.
Let’s look at the second type of weight gain from antidepressants first: putting on extra pounds that weren’t there prior to antidepressant use.
“There is evidence that serotonin activation leads to an increase in appetite,” says Joe Wegmann, psychopharmacologist and licensed clinical social worker, author of Psychopharmacology: Straight Talk on Mental Health Medications.
Serotonin is the neurotransmitter that helps regulate mood, of which deficient levels are associated with depression.
Antidepressants cause an increase in serotonin levels.
Wegmann continues: “There are 14 different serotonin receptor subtypes. The activation or inhibition of some of these serotonin receptors keeps the brain’s ‘satiety switch’ in the ‘off’ position.
“As such, some individuals using the serotonin antidepressants in particular aren’t able to recognize when they feel full while eating, and as such, don’t feel satiated, and continue to eat unnecessarily.”
And that explains why putting on weight can result from using antidepressants. The body fat gain can be offset by exercise.
It’s difficult or impossible to stick to exercise while being ruled by depression, but once an antidepressant subdues those feelings of apathy, lethargy, sadness or that bottomless-pit feeling, you can work towards committing to moderate to vigorous exercise (build up gradually to vigorous if you haven’t exercised in a long time).
Wegmann adds, “Paxil tends to produce the most weight gain among the SSRIs. Weight gain with the SSRIs and SNRIs tends not to exceed 10 pounds in most people.
“There are of course exceptions. Wellbutrin, since it has no serotonin effects, is essentially weight neutral. Some people even lose weight with Wellbutrin use over time.”
The other type of antidepressant weight gain involves putting back on the pounds that you lost due to suppressed appetite from depression/anxiety.
Says Wegmann, “Most people meeting criteria for clinical depression do experience weight loss, precipitated by psychomotor retardation (slowed mind, slowed body) amotivational syndrome, and anhedonia (an inability to experience pleasure).
“Eating is a pleasurable experience for us non-depressed folks, but for depressed individuals, the above mentioned symptoms inhibit appetite.
“So when placed on antidepressants, as the retardation, lack of motivation and inability to experience pleasure improves, eating becomes more pleasurable, appetite increases and weight gain (of the lost pounds) ensues as a result.
“In very severe depressions, significant weight loss may occur. So regaining this weight is essential to health.”
 Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Kzenon
Confusion, Cognitive Impairment from Dilaudid

If someone is on Dilaudid at the hospital, and not long after shows confusion or cognitive impairment, it may very well be the drug talking, which is an opioid narcotic painkiller.
Every single time my mother has ever been given Dilaudid in the ER or hospital room, cognitive changes resulted.
When this first happened, I wasn’t sure if it was the Dilaudid or if something was truly wrong with my mother’s thinking.
It’s scary, to witness mental changes in a family member, especially when the nurse never tells you, “By the way, if you notice any cognitive changes or mental confusion, it’s probably the Dilaudid.”
But after witnessing the confusion and disorientation and irrational thinking in my mother a few times, it began getting predictable: “I’ve seen this before,” I’d comment.
Dilaudid’s Affect on Mental Status
For this article, I asked a physician if Dilaudid, a commonly dispensed painkiller in emergency rooms and hospitals, could cause cognitive impairment (temporary, of course).
“Dilaudid is a very powerful narcotic and can certainly cause confusion and altered mental status, often within 30 to 60 minutes of taking it,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”

He continues, “As with any narcotic, changes in mental status would be normal, but often decrease over time as the body adapts to them.”
My first observation of Dilaudid with my mother was after her knee arthroscopy.
I convinced myself that the irrational thinking and confusion had to have been related to “something they gave her.”
Soon after was double carpal tunnel surgery, and once again, she was on Dilaudid and talking confused, thinking irrationally.
“It has to be the Dilaudid,” I reflected, though also concerned that the confusion might be psychiatrically based. The effects wore off after she returned home.
A year later she was back on Dilaudid … after coronary bypass surgery, and holy smokes, she was in La-La Land.
And maybe lingering effects of anesthesia was involved, but my mother showed numerous signs of altered mentation, such as telling the nurses that I was a doctor (I was a personal trainer).
At first my mother justified this because I was using medical jargon when I spoke to the nurses and doctors.
Then my mother began refuting my claims that I was not a doctor.
Turns out my mother thought that I was her other daughter, who is a doctor.
When my mother came home, she thought she was still in the hospital and thought that I was a nurse.
This was scary stuff, because I also speculated that the heart-lung machine might have caused permanent cognitive impairment.
But during the hospital stay, my mother was given Dilaudid. The confusion dissipated after she was home.
A few days later she was back in the ER with grueling abdominal pain and given Dilaudid, and once again, she began thinking irrationally … until the drug cleared from her system.
Some weeks later my mother was in the hospital for a chronic subdural hematoma suffered after falling and hitting her head, and was given Dilaudid after the brain surgery to drain the hematoma. Once again, she was loopy.
Of course, I couldn’t help think that maybe this time, the loopiness and irrational talking was the result of brain damage from the surgery. It disappeared when she was taken off the Dilaudid.
Not long after, she was in for a second brain surgery; the hematoma had recurred.
This time she was very irrational and disoriented … more so than before, but I kept thinking it’s just the Dilaudid, and made a comment about that to the nurse.
The nurse told me that my mother had not been on any Dilaudid at all, but she was on Seroquel due to agitation the previous night.
So I blamed the cognitive impairment on Seroquel. The cognitive impairment didn’t wear off, like it always historically had done. I was really worried.
I began thinking the neurosurgeon “nicked her brain,” or that “something happened during the surgery” that injured my mother’s brain.
Fast-forward: My mother fully recovered, and after researching chronic subdural hematoma, I have concluded that the deteriorated cognitive status resulted from her brain re-expanding to fill the space that the hematoma had taken up.
The neurosurgeon blamed the impaired mental functioning on a combination of anesthesia, surgery and painkillers.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Effexor Withdrawal How to Minimize Discontinuation Syndrome

A doctor explains how to best get off Effexor to minimize discontinuation syndrome side effects and withdrawal.
Effexor can be difficult to get off of, due to discontinuation syndrome. Ask the many people who have decided to stop taking Effexor (or other SSRI’s), only to experience troubling withdrawal symptoms.
Effexor is prescribed for clinical depression, but getting off it doesn’t have to be difficult.
First of all, if you want to get off Effexor but haven’t made any changes in that direction yet, first consult with your prescribing physician.
Never quit Effexor before discussing this with you doctor.
So, is there a way to make Effexor withdrawal easy, or, at least, not so troublesome?
What are the common withdrawal effects when quitting Effexor?
“The longer you’ve been on the medication and the higher the dose, the more likely one is to get the discontinuation syndrome,” says Dr. David Gutman, Assistant Clinical Professor in the Department of Psychiatry at Columbia University, and Director of Psychopharmacology, ColumbiaDoctors Eastside.
Dr. Gutman continues, “It can include agitation, loss of appetite, anxiety, diarrhea, dizziness, dry mouth, low mood, fatigue, flu-like symptoms, headaches, insomnia, nausea and sensory disturbances (including shock-like electrical sensations), among other symptoms. Most common is a flu-like feeling.”
Why does quitting Effexor cause these side effects?
“It is related to rapidly stopping the serotonin reuptake inhibition,” says Dr. Gutman.
“Medications with longer half lives (they take longer for your body to digest) or that work on other neurotransmitter systems are less likely to cause this condition.”
Can a person just outright quit Effexor?
“A physician should be consulted prior to making medication changes.
“They can help a person decide how quickly to reduce the medication depending on the total clinical situation.”
What is the best way a person can get off Effexor?
Dr. Gutman says, “Reducing the medication slowly is the best way to avoid or minimize the discontinuation syndrome.
“Switching to an SSRI with a longer half life and then tapering that medication is another option.
“Effexor, like other antidepressants and other classes of drugs, should be tapered off of with the guidance of the prescribing physician, to minimize discontinuation syndrome (side effects).
“Clinical or ‘major’ depression in its truest form is incapacitating and can leave people essentially bedridden.
“If depression becomes disabling and a person has difficulty functioning, medication can be very helpful.”
 Dr. Gutmanis interested in the intersection between neurobiology and psychology; his general practice consists of psychiatry, psychopharmacology and psychotherapy.
Dr. Gutmanis interested in the intersection between neurobiology and psychology; his general practice consists of psychiatry, psychopharmacology and psychotherapy.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Has My Child Been Misdiagnosed with ADHD?

If your child’s been diagnosed with ADHD, consider a misdiagnosis; so many other conditions can masquerade as attention deficit hyperactivity disorder.
“I would say that many of the kids I see come in with that diagnosis,” says Claudia B. Rutherford, PhD, a Massachusetts-based licensed psychologist specializing in the psychological and neuropsychological testing of children and adults.
Dr. Rutherford says that the diagnosis of ADHD in her patients “turns out to be incorrect” many times, “and I know that many clinicians feel it is over-diagnosed.”
ADHD Misdiagnoses
Sleep disorders. About 25 to 30 percent of children diagnosed with ADHD actually have untreated obstructive sleep apnea, explains Steven Y. Park, MD, otolaryngologist, author of Sleep, Interrupted: A Physician Reveals The #1 Reason Why So Many Of Us Are Sick And Tired.
Have your ADHD-diagnosed child or teen undergo sleep apnea testing, since this condition can replicate ADHD symptoms such as poor ability to focus on school work or pay attention in class, restlessness and being easily distracted.
Posttraumatic stress disorder. Emotional trauma from a recent crisis event can cause symptoms that mimic ADHD.
Hearing impairment. If your child doesn’t pay attention to you or to teachers, maybe it’s because they’re not hearing adequately.
Numbed hearing can result from a chronic exposure to loud sounds such as screaming and shrieking children/toddlers, wearing earbuds loud with music, being around blaring entertainment systems, motors or machines, or having a history of multiple ear infections.
Mood disorders. Feeling the blues is normal in life, but undue or relentless depression can impair one’s attentiveness.
If you suspect depression, then a medical workup is in order, since this may be caused by a medical situation such as an underactive thyroid.
At the opposite end, bipolar disorder’s “manic” phase can result in hyperactive behavior.
Generalized anxiety disorder. Could your child or teen be unsettled about things going on in their life? New school? Parents’ pending divorce? Problems with a coach or teacher?
Kids can have ongoing anxiety from stressful environments or from getting too much criticism or pressure to be perfect in a sport from a parent.
Learning disabilities. This does NOT mean a low I.Q. or that of being “slow.”
The so-called learning disability is an impairment of information processing that can affect speech, reading, listening and learning math.
Auditory processing deficits. Dr. Rutherford says, “Kids with central auditory processing disorders have trouble performing well in the classroom.”
They do better with one-on-one teaching.
“They can display symptoms that can easily mimic the inattentive type of ADHD,” says Dr. Rutherford, “such as having difficulty following directions in a series, showing comprehension problems during conversations, or poorly discriminating between similar sounding words.”
Speech-language delays. “I see numerous kids with a question of ADHD and turn out to have undiagnosed receptive speech-language delays,” continues Dr. Rutherford.
“These are kids who may have had chronic ear infections or were slow in mastering language acquisition.
“They are behind in the ability to understand spoken language; if this is not diagnosed, it is easy to assume the child is simply not paying attention.”
TBI (traumatic brain injury). Has there been any recent trauma to the head during sports or play? Even if it was months ago?
Autism spectrum disorder. ASD and ADHD share come traits, such as the ability to hyperfocus, repetitive movements (often called fidgeting or stimming) and sensory sensitivities.
However, a child can have both of these conditions, but with only the ADHD being identified during the assessment.
So though there are cases where the child eventually is given an autism diagnosis instead of the ADHD diagnosis, there are also cases in which the individual gets an ASD diagnosis added to their ADHD status. This is now commonly called AuDHD.
Only a psychologist or neuropsychologist with a specialty in evaluating the pediatric population for ADHD should conduct an ADHD assessment.
If a pediatrician or social worker has said to you, “Your child has ADHD,” this really means your child has been exhibiting a minimal number of symptoms that may fit criteria for an ADHD diagnosis.
But you should still seek a formal assessment from a psychologist or neuropsychologist with this specific experience.

Claudia B. Rutherford
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Freepik
Child Has Nightmares about Drowning, Choking: Cause, Solutions
Does your child suffer night terrors about drowning, suffocating or choking?
There may be a very definitive cause for your child’s night terrors of suffocation and drowning, and it will surprise you.
It may very well be sleep apnea. Yes, sleep apnea. Sleep apnea can occur in children, even thin kids.
Kids with sleep apnea are sometimes misdiagnosed as having ADHD, says Dr. Frank Barnhill, MD, board certified family physician practicing child and adult preventative care/ADHD-behavior medicine in upstate South Carolina.
Dr. Barnhill hence sees quite a few children who actually have sleep apnea … which causes breathing problems, including stopped breathing, during sleep, which can lead to night terrors about suffocating or drowning.
Dreams About Drowning Mean a Real-Life Airway Obstruction
Dr. Barnhill explains that night terrors centering around choking, drowning or suffocation are “caused by the child struggling for breath as his or her obstruction to airflow increases and oxygen levels drop.”
Children often describe the sensation as being choked, drowning or suffocating.
Experts think they link the actual event to something they have either seen or read or been told about (television, movies, books, word of mouth stories), as a memory, and it creates a night terror nightmare.”
Dr. Barnhill says that the typical scenario is that the child begins falling asleep.
If the child has obstructive sleep apnea, he or she will start snoring.
If it’s central sleep apnea, the child won’t snore but will develop “sighing breaths.”
As the condition progresses, the respiratory rate will get interrupted by irregular partial breaths called hypopneas, or breathing cessation (apneas).
Both types of breathing disturbances may cause either partial arousal from slumber, or complete awakening, “as the brain tries to alert the rest of the body to falling oxygen levels,” says Dr. Barnhill.
“This explains why some kids awake struggling to get a deep breath, while others are just partially awake and don’t remember it.
“The latter kids often complain of nightmares or night terrors about drowning or suffocating.”
This is easy to understand, the concept of having a dream or nightmare related to a physical problem that’s happening to you in real life.
How many times have you dreamt you were insanely thirsty and couldn’t get enough water in your dream, only to awaken thoroughly parched?
Night terrors about suffocating or drowning have other causes besides sleep apnea.
Dr. Barnhill explains, “Anything that interferes with the child’s normal sleep can cause them — gastroesophageal reflux and restless leg syndrome, for example.”
If your child has the following symptoms, don’t chalk it up to him or her being a pest; instead, consider a real, physical cause of these symptoms: bedwetting, sleepwalking, complaints of things happening to their legs like “bugs biting,” and sudden emotional problems.
The brains of sleeping children are adept at manufacturing a story about what’s really happening to their bodies, and hence, night terrors about drowning, choking or suffocating in kids with sleep apnea and other problems that affect their body.
 In practice for 30+ years, Dr. Barnhill is the author of “Mistaken for ADHD.” He has additional training in Infant, child and adolescent medicine, urgent and emergent medicine, and gerontology. Selfgrowth.com/experts/frank_barnhill
In practice for 30+ years, Dr. Barnhill is the author of “Mistaken for ADHD.” He has additional training in Infant, child and adolescent medicine, urgent and emergent medicine, and gerontology. Selfgrowth.com/experts/frank_barnhill
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can You Have Celiac Disease without Symptoms?

You can have celiac disease and not even know it; that’s because half of people with this autoimmune disorder don’t have any symptoms.
So how do they learn they have it?
Usually it’s because they get tested because an immediate family member–who has symptoms–is diagnosed with it.
The Commonality of Celiac Disease
Celiac disease is more common than most people think, and most don’t have symptoms, says Stefano Guandalini, MD, Founder and Medical Director, The University of Chicago Celiac Disease Center.
The condition is more common than many doctors believe, which is why it takes an average of nine years for this autoimmune disorder to finally be diagnosed in an ailing patient.
Can you have active celiac disease yet no symptoms?
Dr. Guandalini explains, “Yes, in fact, the majority of people with celiac disease have no symptoms at all.” So what brings these individuals to the diagnostics stage if they don’t have symptoms?
Perhaps a first-degree relative has CD and they decided to get tested.
Another way a person, without symptoms, can discover he has celiac disease is if he learns he has the gene/s for the disorder, and decides to get a blood test for CD – which turns up positive for tissue transglutaminase antibodies. The positive blood test then leads to a small-intestine biopsy.
Dr. Guandalini continues, “Even though they have no symptoms, when the disease is active it is doing the same harm internally.
“Ultimately, research has shown that celiac disease left untreated … with or without symptoms … can not only lead to serious complications, but it most definitely leads to a shorter life span.”
The University of Chicago Celiac Disease Center states: There are more than 200 signs and symptoms of celiac disease, yet a significant percentage of people with celiac disease have no symptoms at all.
It continues:
The undamaged part of their small intestine is able to absorb enough nutrients to prevent symptoms.
However, people without symptoms are still at risk for some of the complications of celiac disease.
“To help diagnose celiac disease, physicians first test blood to measure levels of certain antibodies,” explains Dr. Guandalini.
“These antibodies are: the anti-tissue transglutaminase (tTG); the anti-endomysium (EMA); and the anti-deamidated gliadin peptides (DGP).”
He continues:
“A positive antibody test suggests that a person might be celiac, but it is not a conclusive test; a biopsy will be needed to confirm the diagnosis.
“The blood test is, in other words, a quite accurate” first step. If the test is positive, your doctor should know what steps to take next.
Symptoms of celiac disease (remember, not all patients have even ONE of these)…
- Diarrhea
- Constipation
- Bloating
- Gas
- Abdominal pain
- Vomiting
- Weight loss without trying
- Grayish foul-smelling stools
- Fatigue
- Anemia
- Tingling or numbness in the legs
- Tooth discoloration
- Pale sores inside the mouth
- Unexplained infertility and miscarriages
- Brittle bones
- Skin rashes
- Brain fog
- Depression
The disorder, left untreated, raises the risk of bowel cancer, and can cause neurological problems. Treatment is eliminating gluten 100 percent, for life.
Kids and even babies can develop celiac disease.
For children and babies, it can manifest itself by stunting their growth.
The most common symptom of celiac disease in adults is iron deficiency (anemia) that does not respond to therapy.
 Dr. Guandalini is an internationally recognized expert on celiac disease, Professor Emeritus, University of Chicago, and the founder of the University of Chicago Celiac Disease Center. His clinical and research efforts have greatly influenced how celiac disease is diagnosed and treated today.
Dr. Guandalini is an internationally recognized expert on celiac disease, Professor Emeritus, University of Chicago, and the founder of the University of Chicago Celiac Disease Center. His clinical and research efforts have greatly influenced how celiac disease is diagnosed and treated today.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: celiacdisease.net/assets/documents/CDCFactSheet_Symptoms_2010.pdf
Is a Torn Rotator Cuff Always Painful?

If you had a torn rotator cuff, would you necessarily be in enough pain to suspect this?
Or might the pain–even severe–come and go, faking you out?
According to Edmond Cleeman, MD, the pain of a torn rotator cuff can actually come and go, surprisingly.
I’m a former personal trainer and wondered about whether or not pain, from a torn rotator cuff, could take breaks every so often, providing no-pain days for the patient.
“They certainly can have good days,” says Dr. Cleeman, a board certified orthopedic surgeon who specializes in sports medicine and arthroscopic surgery of the shoulder, knee and hip.
This surprised me, because when a rotator cuff is torn, the tendon (usually some of it, rather than all of it) is disconnected from the bone it’s supposed to be attached to; it’s torn away.
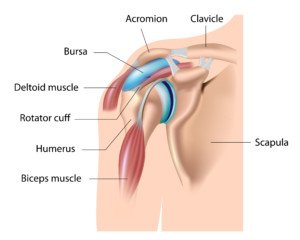
Shutterstock/Alila Medical Media
How could this sometimes be painless?
I can understand this if the patient is still. But “good days” mean that the patient is using the shoulder and arm, and feeling no pain at all, despite the torn rotator cuff.
“To make things more confusing, there are many older patients walking around with rotator cuff tendon tears and don’t even know it,” says Dr. Cleeman, founding member of TRIARQ, a community of orthopedists and physical therapists.
“There are MRI and ultrasound imaging studies that have found that a certain percentage of people have rotator cuff tears without symptoms.
“These studies took groups of people with no shoulder pain and no history of trauma and found that as people age (particularly over 60), a percentage had tears.
“Some studies followed these patients and found that a percentage eventually became symptomatic.”
Tears in the rotator cuff are not always caused by a single-event trauma, such as during a heavy weight lift at the gym, in which the person suddenly feels intense pain arise in the shoulder.
Nor do rotator cuff tears necessarily result over a short time period, in which an athlete repeatedly performs the activity that initiated a small tear, such as throwing or a particular weight-lifting routine.
Many tears happen over time in older people, a part of aging, particularly in people who are not physically fit. The tendons degenerate over time, and a tear results.
A comprehensive strength-training program, especially when initiated during young adulthood, will go a tremendous way in helping prevent tendon degeneration down the road.

Freepik.com
However, even an intense strength training program is no guarantee against an acute injury of the rotator cuff.
For example, the strongest guy in the gym one day plays beach volleyball.
He leaps for the ball and dives into the sand for it, his arm outstretched before him, palm down, as he slides into the sand.
This is a very potential recipe for a shoulder tendon injury.
Thinking he should work through the pain that continues to persist several days later, he decides to do some bench pressing, further injuring the shoulder tendons.
He doesn’t go to a doctor and continues trying to lift weights, and eventually suffers a rotator cuff tear.

























 Dr. Cleeman
Dr. Cleeman







































