Breast Spasm Pain after Augmentation: Solutions

Find out what you can do about painful spasms after breast augmentation surgery.
“Depending on where the implant was placed, it [pain] could be due to occasional spasms that one would have,” says Allen Gabriel, MD, board certified plastic surgeon with PeaceHealth Medical Group Plastic Surgery in Vancouver, WA..
“This is just more noticeable as weight (implant) is pushing against the muscle.”
How long might these painful breast spasms last?
“It is very difficult to assess without a history and exam and I recommend for one to see a board certified plastic surgeon.
Treatment for breast spasm pain from augmentation?
“During the first three months, the spasms are more common and can be daily,” says Dr. Gabriel.
“Stretching the chest and being involved in yoga and Pilates will minimize the spasms.
“It is important to have a good posture and not allow the shoulders ‘roll in.’ It is important to always stretch the pectoralis muscle. Think of a ‘Charlie Horse.’
“We stretch against it to lengthen the muscle; the same should be done with the muscles of the chest.”
Tingling
“The first year as the internal scar is maturing and nerves are regenerating, the internal ‘tingling’ can be noticeable.
“After the first couple of years, spasms and tingling will be minimal but still present since it would have been present with or without the implant.”
A qualified surgeon can be found on this website: plasticsurgery.org
 Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Theerapol Pongkangsananan
Breast Augmentation: Dissolvable Stitches not Dissolving?

A plastic surgeon explains what to do about stubborn dissolvable stitches following breast augmentation.
You’ve had breast enlargement surgery and were sutured with dissolvable stitches—but they’re not dissolving. What’s going on here?
“Depending on what type of suture was used to close the incision, the sutures can last anywhere from three weeks to nine months,” says Allen Gabriel, MD, board certified plastic surgeon with PeaceHealth Medical Group Plastic Surgery in Vancouver, WA.
“During this time, thick scar tissue can form around the sutures and it will take one to two years for the scars to soften up,” he continues.
“Massaging the scar and pinching the scar will help expedite the sutures, and scars soften.”
Type of Sutures in Breast Augmentation
“It is generally preferred to use a longer lasting suture in areas of more tension such as a tight incision where the implant is pressing against it,” says Dr. Gabriel.
“This will also improve the scar long-term, as it will have fewer tendencies to stretch.
“Using shorter lasting sutures may affect the quality of outside scar. So there is a fine line between what we feel and what we see.
“Feeling a thicker scar that can be massaged is probably preferred over having a stretched-out, discolored outside scar that may last forever.”
 Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Kanashkin Evgeniy
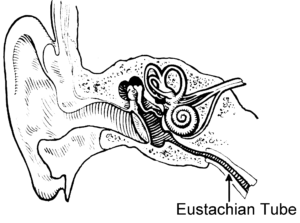
Ears Blocked in the Morning: Causes & Solutions

Find out from an ENT doctor what you can do about blocked ears in the morning and what causes this.
Ever awaken with one ear “blocked” or both of them?
“Causes of blockage in the ears are wax impact in the ear canals, middle ear fluid and Eustachian tube congestion,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“The Eustachian tube allows air to go from the back of the nose to the middle ear,” continues Dr. Silvers.
“When the tube is clogged or congested the ear feels blocked with occasional pressure.”
What else can cause this annoying symptom?
“Allergies or a cold are usually contributing factors,” continues Dr. Silvers.
“Flying with a bad cold can cause fluid in the ear that might not be fully felt until the morning.
“Eustachian tube congestion can be treated with Sudafed, and it can be prevented with decongestants if you have a cold or nasal congestion, or allergy medication if you have allergies.”
As the day goes on, this symptom will eventually dissipate.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Estrada Anton
Why Ear Pain Can Be Caused by Sinus Problems

If you’ve been wondering if the pain in one or both of your ears can be coming from something wrong in your sinuses, you may very well be correct.
But it’s important to realize that this particular symptom — persistent ear pain — can have any number of possible causes (including serious such as a brain tumor or throat cancer) that are unrelated to the sinuses.
Another unrelated cause, believe it or not, is TMJ (temporomandibular joint) disorder.
A problem with the jaw joint can radiate pain to the ear, since the pivotal area of the jaw is located very close by.
Infection is always a consideration, but should respond very well and quickly to a course of antibiotics.
Other benign causes unrelated to the sinus include acid reflux, allergies, arthritis of the neck (cervical) spine, earwax buildup and an impacted tooth.
If your ear pain persists despite being told by an ENT doctor that there is nothing going on with your sinus cavities, then you should pursue this symptom with your primary care physician.
Connection Between Sinus Problems and Pain in the Ears

Shutterstock/Elen Bushe
“Sinus problems commonly cause ear pain,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“The nasal and sinus linings are the same membranes that line the Eustachian tube,” explains Dr. Silvers.
“The Eustachian tube ventilates the middle ear. When the nasal or sinus lining is a little swollen or congested, the ear tube (Eustachian tube) can be swollen as well.
“This leads to negative pressure in the middle ears which can lead to pressure and/or ear pain.”
Additionally, continues Dr. Silvers, “Nasal blockage from congestion or a deviated septum can decrease airflow through that side of the nose and reduce air that gets into the Eustachian tube on that side. This can cause ear pain.”
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Image Point Fr
Cause of Dry Mucous Chunks in Nose Every Morning

Learn the cause and solutions to dry mucous chunks in your nose every morning.
Regarding what causes chunks of dry mucous to build up in one’s nose overnight and cause a blockage in the morning, the expert source is Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“Nasal dryness is a more frequent issue in high altitude and colder climates,” says Dr. Silvers.
“If the nose is dry then mucous will dry, causing it to get stuck in the nose.”
The mucous becomes thick and sticky, becoming trapped in the nasal passages.
Dry nasal conditions can result from various factors, including low humidity, certain medications or medical conditions like allergies or sinus infections.
When mucus dries and becomes sticky, it can make breathing more difficult and may lead to discomfort or congestion, or simply like something’s stuck and compacted up the nostrils.
Fiercely blowing your nose is often ineffective with dry chunks of gunk because they’re so stuck into the nasal passages.
Using a humidifier, staying hydrated and using saline nasal sprays can help keep the nasal passages moist and prevent all that yucky gunk from becoming too dry and stuck.
Sinus Congestion
“Chronic congestion and nasal obstruction causes oral breathing; this can dry out the mouth and the nose especially at night,” adds Dr. Silvers.
“Dry membranes lead to dried mucous and ‘dry mucous chunks’ in the morning.”
If the problem is related to structural blockage in the nasal passages, the buildup of dry mucous will likely be greater on one side of the nose than in the other.
“Patients actively suffering with a cold or with nasal allergies may have higher mucous production that does not clear.”
Dr. Silvers recommends a morning sinus rinse to clear out the accumulation of the unpleasant substance.
Using a neti pot every morning can help prevent this problem.

Neti pot. Shutterstock/kavzov
A neti pot is a small, teapot-shaped device used for nasal irrigation to help clear nasal congestion.
It works by delivering a saline solution into one nostril and allowing it to flow through the nasal passages and out the other nostril, effectively rinsing away gunk and goop, allergens and other debris.
Use of a neti pot also adds moisture to dry nasal passages.
It’s important to use clean water (boil it first for five minutes) and thoroughly wash the neti pot after each use.
When finished, you’ll find that if you give your nose a good blow, a little more mucous should come out.
A humidifier overnight may also be helpful at reducing chunks of gunk in your morning nose. Give it a try.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Cause of White Slimy Stuff on Inside of Lips

A physician explains where the white slimy gunk on the inside of lips comes from…
Have you experienced a white, slimy, goopy substance on the inside of your lips?
“The slimy substance in the mouth is the oral mucosa that is peeling,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“Oral mucosa is like skin cells, will slough off as newer mucosal or skin cells develop.
“This can be exacerbated by certain mouthwashes and toothpastes, especially if the toothpaste or mouthwash is in the mouth for an excessive period of time. This is similar to exfoliating the skin.”
If you’ve noticed a slimy white substance on the inside of your lips, switch oral care products and see what happens.
Dr. Silvers says that this problem can also be caused by side effects of certain medications.
These medications include:
• Antibiotics
• Anticholinergic medications
• Antihistamines
• Cortiscosteroids that are inhaled
• Chemotherapy agents
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/massimofusaro
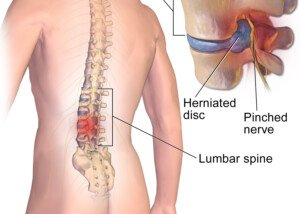
Herniated Disc: Can Excessive Bed Rest Make It Worse?

Warning: Lying down in the name of herniated disc pain is not a smart decision.
Pain in the back (or radiating down the buttocks and/or the leg) from a herniated disc?
It may seem logical to just lie down whenever the pain becomes aggravating, even if this is on a frequent basis.
In fact, this is the advice by medical professionals in years past. And it seemed to make sense. After all, if something hurts, give it some rest by not moving it, right?
And the best way to keep a body part, especially the back, immobile is to get a lot of bed rest.
However, this way of thinking is being overhauled.
Just what are the guidelines for bed rest in those with a painful herniated disc?
“Two to three days of bed rest or recumbency are recommended for a patient with an acute disk herniation,” says Stephen T. Onesti, MD, a neurosurgeon specializing in the spine, with Neurological Surgery P.C. of Long Island. Acute means sudden-onset.
“After this, it is recommended the patient be mobilized and get into therapy and pain management quickly.
“If there are neurological deficits [e.g., leg weakness] or extreme pain, consultation with a spine surgeon is recommended.”
Excessive Bed Rest Will Worsen Symptoms of a Herniated Disc
“It is important that patients do not spend too long on bed rest,” says Dr. Onesti. “Recumbency results in negative metabolic effects and is psychologically debilitating.”
One may begin feeling as though they are on the disabled list from all that time in bed being unproductive.
Furthermore, unwanted weight gain can easily result over time, fueling the feeling of powerlessness.
Dr. Onesti adds, “Also, it is usually not necessary to see a spine surgeon right away.
“Rehabilitation doctors, chiropractors, neurologists and pain management specialists are also effective providers.”
 Dr. Onesti is a board certified neurosurgeon specializing in spine surgery and surgical treatment of chronic pain. He has published many articles in peer-reviewed journals and has given numerous presentations at local and national meetings.
Dr. Onesti is a board certified neurosurgeon specializing in spine surgery and surgical treatment of chronic pain. He has published many articles in peer-reviewed journals and has given numerous presentations at local and national meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Photographee.eu
How to Take Aleve for Herniated Disc Pain Relief
A spine doctor explains how to take Aleve for pain relief from a lumbar herniated disc.
After all, many people actually do wonder just how to take Aleve to combat the discomfort of a herniated (bulging disc).
The instructions on a bottle of Aleve state to take once every 12 hours; it’s a “12 hour relief” pain pill. This is commonly advertised in TV commercials.
Because Aleve is also an anti-inflammatory drug, a person with pain from a herniated or bulging disc may be advised to take this drug to reduce inflammation.
For how many days should a person be consistently on Aleve (or other similar NSAID) before it becomes effective for reducing pain from the inflammation of a herniated disc?
“Regular NSAIDS should be taken three times a day; a minimum of three days should be tried before the effects of the medication can be evaluated,” says Stephen T. Onesti, MD, a neurosurgeon specializing in the spine, with Neurological Surgery P.C. of Long Island.
Is three times a day safe, even though the directions for Aleve state take once every 12 hours?
Dr. Onesti explains, “Most regular NSAIDS are prescribed three times a day. Certain ones like Celebrex are indeed only used twice a day. It will be noted on the prescription.
“Also, patients with kidney problems may not be able to take NSAIDS at all.”
Causes and Risk Factors for a Herniated Disc
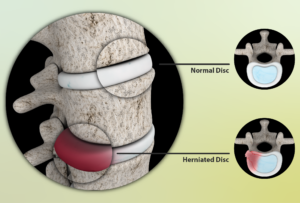
Source: myupchar. com
Degenerative disc disease is the most common cause of the gradual wear and tear that leads to pain.
The aging process makes the discs lose some water content, making them less flexible, more vulnerable to tearing or even rupturing — very painful. A minor twist or strain can be all it takes.
Most patients are not able to pinpoint a time and event that caused the herniation.
But some indeed recall an acute event, such as trying to move a heavy item.
Being overweight or lack of physical fitness are risk factors to a disc herniation.
So is an occupation that involves lots of lifting or twisting, along with a genetic predisposition.
 Dr. Onesti is a board certified neurosurgeon specializing in spine surgery and surgical treatment of chronic pain. He has published many articles in peer-reviewed journals and has given numerous presentations at local and national meetings.
Dr. Onesti is a board certified neurosurgeon specializing in spine surgery and surgical treatment of chronic pain. He has published many articles in peer-reviewed journals and has given numerous presentations at local and national meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/fizkes
Safety of Chiropractic Manipulation on a Herniated Disc
Find out the truth about chiropractic manipulation on a herniated disc in the low back.
Some people are scared to see a chiropractor regarding their herniated (bulging) disc.
This is understandable, since many men and women believe that the only way to treat low back pain is with drugs, surgery, hot packs, cold packs, ergonomic chairs, physical therapy and avoidance of lifting more than 20 pounds.
Perhaps you’ve even heard that chiropractic work on someone with a lumbar herniated disc can be potentially harmful or risky. Well, let’s get to what the truth really is.
“Chiropractic treatments for patients with lumbar disk herniation are safe and effective,” says Stephen T. Onesti, MD, a neurosurgeon specializing in the spine, with Neurological Surgery P.C. of Long Island.
“I have often referred patients to chiropractors, and in my experience they have had excellent results.”
Why would a medical doctor deem chiropractic treatments risky?
Dr. Onesti says, “The risk of neurological or vascular injury due to chiropractic manipulation is basically only when it is applied to the cervical spine.” This is the neck area.
“Experience of the chiropractor is essential–a good chiropractor will not offer manipulation therapy when it’s contraindicated, and will perform it correctly when it is [indicated].
“It should be noted that chiropractors also perform many other type of therapy than just traditional manipulation.”
This includes the strategic use of hot and cold packs.
The Atlantic Spine Center is an example of a conventional treatment enterprise that endorses chiropractic treatment as an option for those suffering from herniated disc pain.
Their site states: When used in conjunction with standard or conventional care, complementary and alternative treatments, such as seeing a chiropractor for herniated disc treatment, can be beneficial to some people with a herniated disc.
 Dr. Onesti is a board certified neurosurgeon specializing in spine surgery and surgical treatment of chronic pain. He has published many articles in peer-reviewed journals and has given numerous presentations at local and national meetings.
Dr. Onesti is a board certified neurosurgeon specializing in spine surgery and surgical treatment of chronic pain. He has published many articles in peer-reviewed journals and has given numerous presentations at local and national meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: atlanticspinecenter.com/spinehealth/conditions/herniated-disc/faq/
Melanoma Detection Technology Catches Cancer Super Early

Yes, there is technology that can catch melanoma very early — much earlier than what a dermatologist’s handheld scope can detect.
The waiting game with moles is over; you do not have to wait till a mole starts looking “scary” or “funny” to peg that spot as something needing medical evaluation.
An early detection program for melanoma goes way beyond simply examining your skin at home and having a dermatologist look it over in the exam room (which often takes only minutes).
“The importance of enrolling in an early detection program is to identify melanomas when they are shallow and have not metastasized, requiring only a simple incision or treatment,” says Richard Bezozo, MD, President of MoleSafe, the world’s most advanced melanoma screening program.
“To the naked eye early melanoma can be mistaken for a mole or lesion. The changes that occur with a melanoma may not be visible for some time.
“For people at high risk for melanoma it is essential that these lesions be identified as early as possible and that action be taken. The best available program for these people is MoleSafe.”
Serial digital dermoscopy is superior to a clinical exam by a dermatologist for detecting melanoma.
“The MoleSafe procedure utilizes a combination of high resolution dermoscopy imaging technology that uses painless, high intensity light to penetrate through the surface of the skin to show the structure of moles,” explains Dr. Bezozo.
“The results are digital, and in high resolution and are quickly interpreted by some of the world’s leading experts in dermoscopy.
“These experts flag hundreds of melanoma cases each year, compared to a dermatologist who will only see a handful.”
Who should undergo serial digital dermoscopy?
Though people at particular risk for melanoma should do this, the technology is open to anybody who wants to get a head start on the earliest melanoma detection.
I myself am in a serial digital dermoscopy program (have had my second imaging), and this gives me great peace of mind.
This technology is also ideal for people who simply cannot inspect their moles due to their location on the body.
Who’s especially at risk?
“The majority of people at risk include those with multiple moles (dysplastic nevus syndrome), people who have had more than one blistering sunburn, people who have had melanoma before, and people on an immunosuppressive agent,” says Dr. Bezozo.

Richard Bezozo, MD