Men Who Exercise but Sit a Lot at Risk for Heart Failure
Men who have a desk job have an increased risk of heart failure even if after work they hit the gym like a warrior–not exactly the news you wanted to hear, right?
If you work out like a beast after work, but sit a lot on the job and then also at home, your risk of heart failure increases.
There is a very intriguing study report in the journal Circulation: Heart Failure.
To prevent heart failure, one must take a two-pronged approach: 1) exercise a lot, and 2) avoid prolonged sitting. “Be more active AND sit less,” says lead study author Deborah Rohm Young, PhD, in the paper.
The Study
A racially diverse group of over 84,000 men, from age 45 to 69, without heart failure at the get-go, were followed for about eight years.
The Results
Men with a lot of inactivity were 52 percent more likely to acquire heart failure than were men with high activity levels.
This isn’t just about structured exercise sessions, but overall movement that was carried out beyond the workplace (the study didn’t account for movement on the job).
Beyond the workplace, men who spent at least five hours a day in a chair were 34 percent more likely to acquire heart failure than were men who sat around for less than two hours a day.
This higher heart failure risk was independent of how much they engaged in structured exercise.
For men who sat for a minimum of five hours a day, and did little structured exercise, risk of heart failure was doubled that of men who exercised a lot, as well as spent under two hours a day sitting.
Study Limitations
The results may not apply to women; physical activity was self-reported, and thus, may have been over-reported; results were based strictly on time outside the workplace.
How to Oppose the Sitting Disease
A lot of home sitting time is done while a person works on a computer. How about getting a treadmill desk?

If you’re entrenched in computer activity, you’ll forget you’re walking. I know; I have a treadmill desk.
Set the speed to even one-half mph, and this is all you need to oppose the sitting disease.
Another way to reduce sitting time and lower heart failure risk is to (yes, I’m serious) watch TV while standing. But you should move around a bit while standing.
Less Sitting Time at the Gym
The study shows that gym time alone isn’t enough to fight off the sitting disease.
How much sitting do you do while at the gym in between sets?
You may be on your can far more than you think, what with texting and other phone use in between sets.
Stand while using your phone.
Walk around in between sets instead of sitting on a bench.
If you think someone will grab your seated equipment if you leave it, then pace very close to it, or at least stand beside it — anything to get off your butt.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com
Source: sciencedaily.com/releases/2014/01/140121164743.htm
Ascending Aortic Aneurysm Stent Graft Repair Is Here
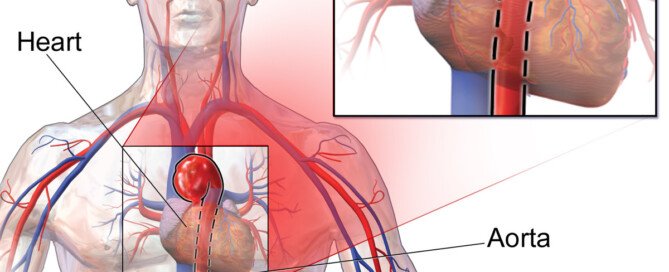
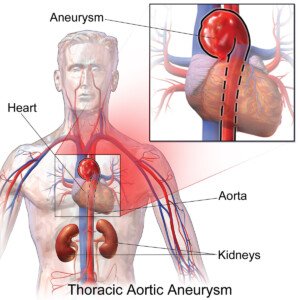
Stent graft technology for the repair of an ascending thoracic aortic aneurysm is a marvel of medical advancement.
Stent technology continues to evolve; soon, endovascular repair (stent grafting) will be more common with ascending aortic aneurysms.
Currently, fusiform ascending aortic aneurysms cannot be repaired with stent grafting (endovascular repair) because the placement of the stent requires landing zones.
The ascending aorta has openings that are formed from the vessels that branch off the top of it where it begins arching.
A stent graft would overlap one of these openings in order for the graft to be set in place.
If one of these portals is obstructed, then adequate blood supply will not flow through the vessel branch and reach other parts of the body.
The descending aorta has no openings formed by vessel branch-offs; hence, stent grafts can be set in place with generous landing zones.
This is why endovascular repair of a descending aortic aneurysm is rather common.
New Stent on the Block

A new kind of stent—multilayer—has been developed, and Grayson H. Wheatley III, MD, is leading the way.
He is an aortic disease surgeon with TriStar Cardiovascular Surgery in Nashville, TN.
“The advantage of this stent is that because the stent has an open structure, it can cover branches without interfering with flow,” explains Dr. Wheatley.
Dr. Wheatley further explains that “the stent can be used in the ascending aorta and if additional landing zones are needed, it can cover the coronary arteries or the great vessels.”
The great vessels are the ones that branch off the aorta’s arch.
“This may be the best solution for ascending aortic aneurysms,” adds Dr. Wheatley.
“There wouldn’t be blood flowing into the aneurysm around the stent except in rare cases where the aneurysm goes all the way to the aortic valve (called aortic root aneurysms).”
When will endovascular treatment of an ascending aortic aneurysm become more common?
“We are working with the FDA to initiate a trial for high risk surgical patients with complex aneurysms.”
Normally, when the diameter of a TAA reaches close to 6 cm, it’s time for repair in a patient who has not been having symptoms, and does not have a connective tissue disorder or a bicuspid aortic valve.
(Patients who do have at least one of these variables have a lower measurement threshold before surgical repair is warranted.)
Learning about this threshold got me thinking about how all of those people, who are under 5.7 cm but greater than 4 cm, must continuously live on what I call the disability list, not to mention the anxiety that a sudden charge of emotions, straining on the toilet or lifting a child might cause a rupture.
Could the new multilayered stent graft lower the threshold measurement?
After all, living with a TAA is unnerving; why wait for it to reach 5.8 cm when it can be endovascularly repaired at 4.5 cm?
Lowering the threshold is a potential possibility, says Dr. Wheatley. “The decision on when to treat an aneurysm is based on the risk of rupture versus risk of surgery.
“With this new stent, the risk of the surgery would potentially be much lower and thus we might be able to treat patients earlier with smaller aneurysms, but this has yet to be studied with this device.”
The evolution of a milestone in stent technology is only beginning; you will be hearing a lot more about this remarkable advance in endovascular stent grafting for thoracic aortic aneurysms.
More About the Stent
Dr. Wheatley explains: “This type of stent functions differently than coronary stents even though they both have an open mesh.
“This stent was developed by a team of engineers who understood fluid dynamics and the role of blood flow in an aneurysm sac.
“These specialists took their understanding of fluids and applied it in a way that no one had previously thought of with regards to treating aneurysms.”
 Dr. Wheatley is an internationally recognized expert in aortic treatments and specializes in open and endovascular repair of complex aortic diseases plus the surgical treatment of coronary artery disease and valvular heart disease. Check out his website.
Dr. Wheatley is an internationally recognized expert in aortic treatments and specializes in open and endovascular repair of complex aortic diseases plus the surgical treatment of coronary artery disease and valvular heart disease. Check out his website.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/BruceBlaus
My 600 Pound Life: Enablers Should Be Questioned

Why doesn’t the show, “My 600 Pound Life,” corner the enabling spouses and require them to explain their actions?
The enabling spouses on “My 600 Pound Life” need to explain why they continue bringing huge quantities of junk food to their bedridden, super morbidly obese partners.
One episode of “My 600 Pound Life” focused on Penny Saeger. She was bound to her bed, and her husband, Edgar, was shown bringing her tray-fuls of rich, high calorie foods.
At one point, Penny Saeger’s sister spoke about this — and quite briefly.
Penny’s sister commented to the effect that Edgar brings his wife what she wants — or there will be “trouble” otherwise. Then the brief segment ended.

Penny (above image) underwent the surgery and was not losing weight despite being in the hospital.
The surgeon, Dr. Younan Nowzaradan, believed someone was sneaking her food, though this was not confirmed.
She was sent home, which was actually an apartment that Edgar had found nearby the hospital.
From the apartment, Penny was expected to stick to a low calorie diet and attend doctor appointments.
Instead, the cameras followed Edgar preparing huge amounts of junk food and bringing them to Penny, who was as bedbound as ever.
The cameras did not show Penny demanding Edgar bring her the food. The show simply followed him serving her, and her gorging.
The question all viewers have of “My 600 Pound Life” is what is going ON with Edgar and all the other enabling spouses?
They do not care about one more box of donuts being handed to the bed- or chair-bound 600+ pound family member.
In nearly every episode of “My 600 Pound Life,” the subject lives with at least one enabler.

They never live alone — except maybe for one or two over the many seasons of the show.
That’s because if they did, there’d be no enabler to help them become bed- or chair-bound.
- Viewers would like to know what the enablers are afraid of.
- Viewers wonder if there’s more to the dynamic than, “I bring her food because it makes her happy.”
How much power can a bedridden person have?
A bedridden person can wield a LOT of power to the enabler who has severe psychological issues.
Childhood Roots
Anyone who saw Penny on “My 600 Pound Life” can easily figure out why she was so afraid to commit to lifestyle changes to lose weight.
The tragedy is rooted in Penny’s childhood. Briefly touched upon was abuse at the hands of her father.
Penny’s parents were not mentioned in the present. We can easily imagine that her father made her believe she’d fail at anything she’d try.
So maybe the idea of trying to walk with the help of a physical therapist, post-surgery, was too frightening, which is why after four months, she couldn’t even take a few steps.
And the idea of sticking to a diet so that she could live long enough to see her son enter middle school was just too daunting.
Why Won’t TLC Explore the Enabling Dynamic?
Sometimes the enabler is asked point-blank by Dr. Now why they bring so much food to the sufferer.
There are three basic responses:
- I hate to see her hungry.
- It makes him happy.
- There’ll be hell to pay if I don’t.
And then the probing stops there. Viewers are left thinking, “WHAT…?!
Perhaps the probing indeed gets carried out, but the footage gets cut — but if that’s the case…then why has it been getting cut for all but a few episodes?
Much episode footage involves moving preparations to Houston, surgical prep and the actual surgery.
Thus, there is plenty of air time to explore the enabler dynamic. Certainly, viewers would rather see this investigated than watch people packing boxes for the move or endoscopic images of someone’s gut.
This is one reality TV show that can’t be faked, save for perhaps what seem to be some pre-orchestrated argument scenes among family members and the overly scripted “I’m afraid the doctor will turn me away.”
Each episode of “My 600 Pound Life” is now two hours. For sure, there is plenty of time to delve into the mysteries of what makes the enabler’s mind tick.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Microscopic Colitis Exercise Guidelines by GI Doctor

Exercise will NOT make microscopic colitis worse.
So don’t use microscopic colitis as an excuse to avoid working out at a gym, even if you’re having diarrhea 20 times a day.
“Generally speaking, exercise is good for the body,” begins Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“It can improve specific conditions, such as microscopic colitis, and your general health.”
If urgency is a problem, then you should try to configure your workout routine close to the gym’s restroom, whenever possible.
Dr. Fine’s Recommendations for Exercising with Microscopic Colitis
Consider yoga. Yoga exercises can aid in the digestion process.
Certain yoga poses may help people with microscopic colitis or other gastrointestinal (GI) conditions.
A few poses I recommend include flowing bridge pose, Marichi’s pose and revolved triangle pose (below).
If you aren’t sure how to get started, there are many websites, books and classes that may help you learn about yoga.
Establishing a regular exercise routine is essential for maintaining long-term fitness and health.
By incorporating exercise into your daily schedule, you form a habit that increases your likelihood of sticking with it.
To support this habit, start with a basic routine that you can gradually build upon.
Stretching before and after your workouts is crucial for relieving muscle tension and reducing the risk of injury.
If you have gastrointestinal conditions like microscopic colitis, pay special attention to exercises targeting muscle groups near the GI tract.
Kegel and pelvic floor exercises can be particularly beneficial in this regard.
Incorporate both core strengthening and cardiovascular exercises into your routine.
Cardiovascular workouts are excellent for managing weight, which can ease joint stress and mitigate the risks associated with diabetes, heart disease, and various GI conditions.
Strengthening your core supports overall stability and can improve posture and balance.

Freepik.com/yanalya
Exercising with a friend can make your workouts more enjoyable and provide motivation.
Having a workout buddy can also help you stay accountable to your fitness goals.
Finally, always seek recommendations from your doctor to ensure that your exercise routine is safe and effective for your individual needs.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Can Microscopic Colitis Diarrhea Cause Nutrient Loss?

Do you ever wonder if all the good things you eat are being passed out of your system by your microscopic colitis?
Does this disease make healthy food come out withthe diarrhea?
Let’s say a person eats a lot of fruits and vegetables whole, and/or juices them.
Shortly after they have the classic porridge-like or watery diarrhea the color of the consumed produce (greenish for spinach, reddish for beets, plus visible particles of produce floating in the toilet water).
Does this indicate that a significant amount of nutrients went right through the person?
“Yes, when the body expels waste, nutrients are also expelled,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“That’s one of the reasons it’s so important to stay hydrated. I recommend drinking an ounce of filtered water, per kilogram per day.”
What would you tell a patient who’s concerned about wasting produce because it appears that much of it comes out in their diarrhea?
Assume this individual has only microscopic colitis—no other GI diseases or other medical conditions.
But they’re concerned that all that juicing or whole-fruit consumption—which they do for the nutrient density—is being wasted.
“What you’re describing is rapid transit and possible malabsorption,” says Dr. Fine.
“The patient should see a gastroenterologist for evaluation. The gastroenterologist can recommend treatment options, including diet changes.
“What he/she recommends depends on what is causing the rapid transit, but usually in situations like this, I recommend chicken and rice soup, and nutritional supplements with predigested sugar components.
“Also, avoid juices and raw vegetables while the diarrhea is occurring and take a multivitamin with minerals.”
That may be a tough pill to swallow for those with microscopic colitis who strive to get a lot of antioxidants and enzymes (abundant in fruits and vegetables) in their daily diet.
But if a significant amount of these nutrients is going to end up getting expelled through your other end, you may as well avoid these foods so that the flare-up of microscopic colitis has a chance to recede.
After all, it’s no secret that fruits and vegetables can bring the diarrhea into the spotlight.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/bitt24
Why Can Microscopic Colitis Cause Low Back Ache?

Is that low backache you have a part of your microscopic colitis? Or is it just a coincidence?
But if it’s a coincidence, why does the timeline include diarrhea?
“None of my microscopic colitis patients have exhibited signs of low back ache,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“However, low back ache can be associated with gastrointestinal distress because of where our intestines are located. Our bodies are a complex network. Everything is connected.”
But can the low back ache that some people with microscopic colitis get be caused by something else related to this inflammatory bowel condition?
“None of my microscopic colitis patients have exhibited this particular symptom, but based on what we know about prostaglandins, it can be speculated that they may be contributing to lower back pain.,” explains Dr. Fine.
What are prostaglandins?
“Prostaglandins are chemicals that generally cause inflammation, and ‘aching’ is often considered a symptom of inflammation,” says Dr. Fine.
This explains why the low back ache that I myself have experienced with microscopic colitis felt identical to that caused by premenstrual syndrome (PMS).
After all, the “pains” of PMS are caused by prostaglandins, which is why NSAIDS such as ibuprofen work remarkably well at suppressing the discomfort.
However, people with microscopic colitis should never take NSAIDS, as this class of drugs can worsen the condition.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/aijiro
Sources:
onlinelibrary.wiley.com/doi/10.1111/j.1365-2036.2011.04686.x/full (prostaglandins and MC)
ncbi.nlm.nih.gov/pmc/articles/PMC3629156/ (prostaglandins and MC)
ncbi.nlm.nih.gov/pubmed/6350580 (prostaglandins and PMS)
ncbi.nlm.nih.gov/pubmed/19594490 (prostaglandins and IBD)
Microscopic Colitis Joint Aches Preceding Diarrhea for How Long?

Did you know that the joint aches of microscopic colitis can occur many days before the first day of a new flareup of diarrhea?
A small percentage of people with microscopic colitis experience associated but benign joint aches.
Medical literature says that joint aches, that are associated with Crohn’s disease and ulcerative colitis, can precede the gut problems of these conditions in a new flare-up.
But what about joint aches, that are linked to microscopic colitis, occurring in a new flare-up of this IBD, before the diarrhea comes?
“The amount of time it takes for each symptom to manifest itself varies from patient to patient,” explains says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“Some may have joint aches for three months before they start seeing other symptoms, but it could take years.”
Arthralgia: pain in the joints (“arth” refers to joints, and “algia” refers to pain).
“I recommend seeing a rheumatologist if you’ve had joint aches for a couple of weeks or more,” continues Dr. Fine.
“Generally speaking, joint aches aren’t just joint aches – just like diarrhea isn’t just diarrhea.
“These symptoms are often signs of more complex issues, and it’s best to get as much information as you can, as early as possible.”
What if the patient has already been diagnosed with microscopic colitis?
This condition can be transient or intermittent, while others have it daily and chronically.
“Every patient is different, so yes — it is possible that they will experience joint aches for a while and then diarrhea,” says Dr. Fine.
There’s no research on this precise phenomenon. Why would researchers want to invest time and money on studying the range of time that can pass between onset of joint aches and onset of diarrhea in a flare-up of microscopic colitis?
Nevertheless, I’m sure that some individuals who have microscopic colitis wonder about this.
It sure got ME thinking, because I’ve had two bouts of microscopic colitis in a three-year and eight-month period.
The second round was the craziest thing because it consisted of joint aches ALONE that masqueraded as PMS (especially since one of the locations of the aching was the pelvic region)—only I had by then completed menopause!
Differential Diagnoses
- One last “hurrah” of an ovary: PMS, despite high fsh level
- Ovarian cyst (though this won’t cause ankle, wrist or neck aches, which I had)
- Psoriatic arthritis, which my brother has (though this won’t cause pelvic cramping, which I had)
- Celiac disease (a past lab test revealed I have the celiac gene)
- A second flare-up of microscopic colitis (though I didn’t have any diarrhea)
Time passage ruled out ovulation, and tests ruled out any other gynecological cause.
Going gluten free for five days ruled out celiac disease. That left psoriatic arthritis or microscopic colitis.
But no matter how much I searched the Internet, I could not find even one medical journal or medical site that named pelvic pain as a symptom of psoriatic arthritis.
After 27 days of my mysterious aching (ankles, upper legs, low back, wrists, pelvic area), I experienced explosive, watery diarrhea!
Over the next four weeks I had 25 episodes of watery or porridge-like diarrhea. There was also some gas and “bubbly” like sensations in my stomach.
For how long can joint aches precede a flare-up of microscopic colitis?
Twenty-seven days for at least one individual. Oddly, two days after the diarrhea came, the brunt of the arthralgia disappeared.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com/ Racool_studio
Sources: ccfc.ca/site/pp.asp?c=ajIRK4NLLhJ0E&b=6349433&printmode=1
rheumatology.org/Practice/Clinical/Patients/Diseases_And_Conditions/Psoriatic_Arthritis/
Microscopic Colitis Flare-up: How Short Can It Last?

Microscopic colitis can be chronic or intermittent. It can also be transient, which isn’t necessarily the same as intermittent.
For example, I’ve had only two blatant rounds of a microscopic colitis flare-up over a period of three years and eight months.
The first flare-up lasted about two months. The second persisted for about five weeks.
The concept of transience and intermittency can be vague.
“Microscopic colitis flare-ups vary in length and intensity from patient to patient,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“Diet, exercise, sleep patterns, stress, and many other factors can affect a flare-up. It can take weeks or years to heal.
“MC flare-ups can vary from a few weeks to several years. Some factors that may help shorten a flare-up include eating a gluten-free diet and avoiding NSAIDs because they can damage the GI tract.
“Generally a three-month course of budesonide will take care of a microscopic colitis flare-up, but people who have more refractory cases may need other agents such as azathioprine and anti-TNF agents.”
The Diarrhea of Microscopic Colitis
Typically, the diarrhea is explosive. This means it bursts out of you very fast, splattering its contents all over the interior of the toilet bowl.
This burst or explosion is made possible by the high volume of water that’s mixed in with the diarrhea.
Sometimes it appears that what’s coming out of you is dark thick urine, when in fact, it’s very liquid diarrhea.
There may be severe abdominal cramping beforehand that disappears after voiding.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Notto Yeez
Can Microscopic Colitis Symptoms Be Too Mild to Notice?

Can the symptoms of a microscopic colitis flare be small enough to appear below the radar?
Can the signs be so subtle that they fail to register on your awareness map?
Microscopic colitis is not an “all or none” condition.
I was diagnosed with microscopic colitis in May 2010, but does this mean that my first bout was at this time?
I really wonder, because there have been a few times way, way in the past in which I had experienced what I now know to be “explosive watery diarrhea.”
It had happened just a few times here and there over a span of years. Maybe it was something I had eaten. But maybe not.
I began juicing several years prior to my diagnosis, and noticed that on just about every juicing day, within 90 minutes to two hours after consuming an average of 32 ounces of juiced fruits and vegetables, I’d have one episode of major diarrhea.
It wasn’t watery or explosive, but it was like a thick porridge. I’d have just one occurrence, then I was done for the day.
I simply thought that all the juicing was triggering this. The diarrhea occurred only on days that I juiced.
Mild Microscopic Colitis Symptoms
“Yes – you can have microscopic colitis and not know it. You might not exhibit all the usual symptoms but still have the disease,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“With microscopic colitis, the colon looks completely normal until you get to the microscopic level.
“On the microscopic level, it’s abnormal. In some cases, a patient could have sub-acute symptoms. Sub-acute or milder symptoms may be harder for patients to recognize.”
My first round of microscopic colitis came and went (lasted about two months). The second round occurred about three and a half years later and lasted about five weeks.
But in between, could it have been there on a sub-acute or “low grade” level, masquerading as juicing-induced diarrhea?
I’d see particles of fruit/vegetable fragments floating around in the brown murky water of the toilet.
The diarrhea that I had with my first round of microscopic colitis did not look like typical diarrhea.
It looked really weird and came at all times of the day (including nocturnally) – even though during that time I was not juicing.
At around the beginning of 2013, I became gradually aware that I was no longer having diarrhea on juicing days; the bowel movements were normal.
This went on for months, and it really got my attention, because I was so used to the diarrhea.
“Why isn’t the juicing causing the diarrhea anymore?” I wondered. I had always thought that the fiber content in 32 to 40 ounces of juiced produce caused the diarrhea. So where was it now?
In retrospect, I’m thinking that maybe all along, it had been a very subtle manifestation of microscopic colitis, and that in 2013, I went into complete remission. Then…I had my second MC round later in the year.
Enteropathic Arthralgia Mimicking other Conditions
If you’re having subtle joint aches but no other symptoms, this, too, can be microscopic colitis, especially if you’ve already been diagnosed with MC and believe you’ve been in remission for a while.
It will be especially inconspicuous if the aching is in only one part of your body, such as only the low back.
After all, low back pain is extremely common and easily brought on by a combination of physical de-conditioning and improper lifting around the house or on the job.
The timeline could be a coincidence, when it’s really MC at work.
(Low back pain can also be brought on by physical de-conditioning alone! As a former personal trainer, I’ve witnessed this with clients who were new to exercise but complaining of low back pain.)
A subtle flare-up of microscopic colitis can also be missed by a fertile woman who’s experiencing what she believes are the minor aches of mid-cycle joint pain—when in fact, it’s enteropathic arthralgia.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Andreas Poertner
Are the Joint Aches of Microscopic Colitis Destructive?

Ever wonder if the joint aches you get with your microscopic colitis will over time cause damage to your joints, possibly weakening them or making them permanently stiff?
“Joint pain” doesn’t always mean damage or degeneration to the joints, and this includes in microscopic colitis.
When you hear or see the words “joint pain,” do you automatically think of gnarled fingers and a compromised ability to unscrew jar lids, carry a suitcase, tie a knot or handle a bowling ball?
Joint pain is one of several symptoms that can result from microscopic colitis.
It can also result from an injured tendon, worn-down cartilage, torn ligaments and rheumatoid disease. And premenstrual syndrome.
“At present, we do not know enough about microscopic colitis to understand how it affects the joints, but we know joint aches often accompany the disease,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
Aches vs. Pain
Dr. Fine explains: “The type and intensity of joint aches can vary greatly from patient to patient, with a wide variety of contributing factors, such as age, diet, exercise, stress, etc.
However, there is research that suggests certain types of arthritis, like enteropathic arthritis, may be a manifestation of microscopic colitis, and enteropathic arthritis is considered nondestructive.
In these cases, once the underlying microscopic colitis has been treated effectively, the joint aches associated with it are resolved.”
Don’t let the term “arthritis” trick you into thinking this necessarily means the deformed fingers you’ve seen in people with arthritis. Don’t let those pharma TV commercials about arthritis mislead you, either.
“Arth” refers to joints, and “itis” means inflammation.
In microscopic colitis, there may be an inflammatory process occurring in the region of the joints.
This process is NOT the same as the one that occurs in, for example, rheumatoid arthritis or psoriatic arthritis.
“Arthritis” is a general or catch-all term that can have many meanings to the layperson, and numerous etiologies that result in different types or experiences of discomfort.
In the midst of the joint aches I’ve had from my own microscopic colitis, I have carried out intense and heavy weight lifting—without any deficits in performance.
In fact, rigorous use of my joints (deadlift, bench press, squat, kicking a heavybag, etc.) suppressed the achy feeling that was being generated from microscopic colitis.