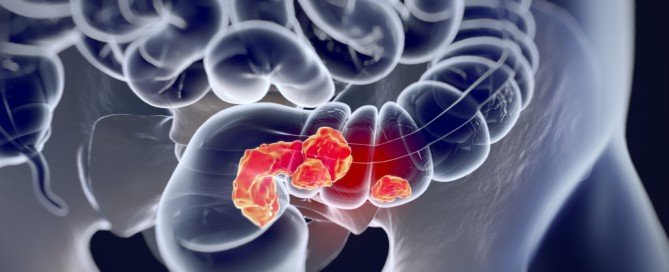
How Long Can Colon Cancer Go Undetected?
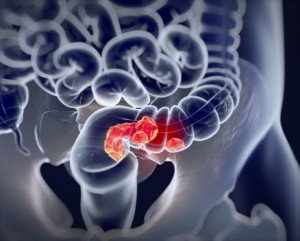
A gastroenterologist explains how long cancer of the colon can go undetected.
“Cancer [including that of the colon] can go undetected for many years since it rarely causes any pain or symptoms other than anemia,” says John Covington, MD, a gastroenterologist with a private practice in Maryland.
“If caught early it is curable. Polyps can sometimes turn into cancer, but they do not cause any symptoms.
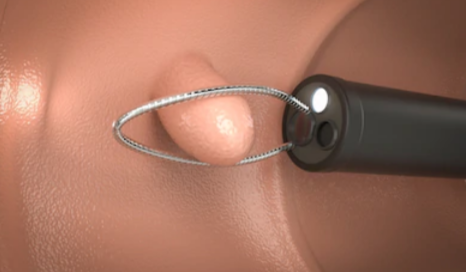
“You don’t know that you have polyps unless the doctor looks inside with a colonoscope. So in order to detect and remove them, colonoscopy is needed every 10 years.”
Based on this information, one can deduce that cancer in the colon can go undetected for up to 10 years, meaning, a colonoscopy turns up normal results, and then one a decade later shows a malignant tumor.
But it’s impossible to tell at what point along the timeline that a polyp, which would have precursed a primary cancer in the colon, began growing, and even more elusive would be at one point it began transforming into a malignancy.
Another point to consider is that a person may begin developing symptoms from a colon cancer, but there’s no way to tell how long the disease had been festering inside their gut prior to the development of symptoms.
The precise, absolute answer to “How long can colon cancer go undetected,” then, remains undetermined.
A colonoscopy can prevent the development of colon cancer.
 Dr. Covington provides comprehensive care for digestive tract diseases, offering the latest diagnostic and treatment options including colonoscopy, upper endoscopy and small bowel capsule endoscopy.
Dr. Covington provides comprehensive care for digestive tract diseases, offering the latest diagnostic and treatment options including colonoscopy, upper endoscopy and small bowel capsule endoscopy.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Anatomy Insider
sscpywrt26
How Long Does It Take for a Colon Polyp to Become Cancer?
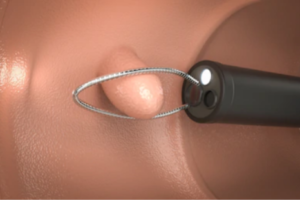
You know that a polyp can be sitting in your colon for years, but just how long does it take to turn into cancer?
There’s a real high risk for cancer transformation of a colon polyp, which is why they are removed right on the spot when discovered during a colonoscopy.
Time It Takes for a Polyp to Turn into Colon Cancer
Two Basic Kinds of Polyps
“Hyperplastic polyps which are never thought to turn to cancer, and adenomatous polyps (also called adenomas, which can potentially grow to cancer after many years),” explains John Covington, MD, a gastroenterologist with a private practice in Maryland.
“But most adenomas will not turn into cancer.”
There are five total types of polyps.
Why are screenings recommended every 10 years for those at average risk of colon cancer?
“We recommend regular screening colonoscopies every 10 years because the vast majority of adenomas in the average patient grow slowly and pose no risk for at least 10 years,” says Dr. Convington.
“Therefore a routine colonoscopy every 10 years will assure us that colon polyps can be detected and removed long before cancer develops.”
The 10-year guideline applies to people with average risk of colon cancer.
Dr. Covington says, “There are special situations where cancer risk is higher and could develop earlier, but your doctor can identify those particular situations where colonoscopy is needed sooner and more frequently.”
 Dr. Covington provides comprehensive care for digestive tract diseases, offering the latest diagnostic and treatment options including colonoscopy, upper endoscopy and small bowel capsule endoscopy.
Dr. Covington provides comprehensive care for digestive tract diseases, offering the latest diagnostic and treatment options including colonoscopy, upper endoscopy and small bowel capsule endoscopy.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Phonlamai Photo
sscpywrt26
When It Comes to Bullying Among Kids, Size DOESN’T Matter

It’s actually often the case that a bully is much smaller than the victim.
You’ve probably witnessed this growing up: The meanest bully is far from being the biggest kid in the grade or even classroom.
Certainly many people, in childhood or teen-hood, have witnessed bullying situations in which the victim was the bigger of the two.
This phenomenon occurs in adults all the time — in which the victim is bigger — so why wouldn’t it also be prevalent among school kids?
Though it’s easier for one to be a cyber bully since they are safe behind a computer screen and don’t have to worry about getting punched by the victim, it still stands even today that often, the bully has enough fire inside that it’s not required for their targets to be smaller.
“Bullying is becoming more of a mental game than a physical one with multiple ways in which a bully can ridicule or induce a feeling of powerlessness within a victim,” says Kyle Gillett, Ph.D., LMFT, Executive Director and Founder of Solstice East and Asheville Academy for Girls.
He leads groups and conferences on bullying, helping not only victims but also the bullies.
But as far as face-to-face bullying, it’s “truly a myth” that the mean kid is usually bigger, heavier and/or taller, says Tara Fishler, a conflict resolution specialist and founder of Customized Training Solutions in New York which provides conflict resolution, training and strategic management services.
“Once when I taught a parent workshop, I used clip art of a bigger child punching a smaller child,” says Fishler.
“A parent came up to me and asked me not to use that in the future. Her son was a big kid and it seemed people assumed he was a bully, but from her perspective, he was a sweet kid who was often the target, not the perpetrator.
“I never used that image again. It is not a child’s size that matters; it is the authority they project.”
There’s nothing inherent in a big body that increases the propensity for becoming mean. What drives a child to become a bully are the circumstances at home, not the size of his body.
A small child with enough anger or learned-aggression in him can always find a vulnerable, non-assertive classmate to heap on, and vulnerable, defenseless kids come in all sizes—including extra large and extra tall.
In junior high school and high school I witnessed incidents involving bullies who were a lot smaller than their targets.
“While there isn’t a universally accepted definition of bullying, the best way I can describe it is some type of aggressive behavior (physical, emotional, social, etc.) from one individual or a group of individuals with the intent to harm (physically, emotionally, socially, etc.) in which a power differential is present,” explains Dr. Gillet.
“This power differential can take many forms—including physical (bigger or stronger), intellectual (smarter or more savvy), social (more “popular” or accepted), or could even represent a power differential in numbers (a group of kids bullying one single child).
“So, again, size is only one example of power differential that can be present in a bully.”
 Tara Fishler works with adults and students creating interactive workshops on numerous topics including anger management, communication skills and anti-bullying.
Tara Fishler works with adults and students creating interactive workshops on numerous topics including anger management, communication skills and anti-bullying.
 Dr. Gillett’s career has focused on treating both boys and girls, with specialization in trauma, processing difficulties, eating disorders, depression, anxiety, OCD and difficult family systems.
Dr. Gillett’s career has focused on treating both boys and girls, with specialization in trauma, processing difficulties, eating disorders, depression, anxiety, OCD and difficult family systems.
Source: solsticeeast.com, ashevilleacademy.com bully bigger than victim
Do Kids Who Don’t Get Spanked Become Bullies?

If you never spank your child, will they be at higher risk of eventually becoming a bully towards other kids?
Is there really a connection between lack of corporal punishment and becoming a bully?
More than one parent has posted in a forum, “If more people spanked their children, there’d be a lot less bullying.”
But we really have to look at this from a logical perspective rather than from an emotional perspective.
Just how on earth can getting NO spankings inspire a child to push around a classmate or pick fights in the schoolyard?
To put this another way, how would punishment of only timeouts, groundings, being sent to one’s room and confiscation of toys, the computer, TV, etc., encourage that child to then go out and shove other kids to the ground, trip them or unleash verbal insults?
Do you really believe that the absence of spankings made this child mean?
Why do kids become bullies?
– To prevent being a victim.
– Low self-esteem; bullying makes them feel 10 feet tall.
– To be revered by classmates as a leader.
– Learned behavior: An older person in the household, usually a parent, bullies the bully; or, the bully has repeatedly witnessed a parent behave aggressively towards other adults.
Expert’s Perspective
“It’s unfortunate when blanket statements are made regarding specific parenting approaches,” says Kyle Gillett, PhD, a licensed marriage and family therapist, and Executive Director and Founder of Solstice East and Asheville Academy for Girls.
He leads groups and conferences on bullying, aiding victims and also the bullies.
“The truth is that spanking or the lack of spanking in a parenting skillset has never been shown to cause anything — the association lies much more in the overall approach that parents apply in their parenting.”
Parenting can be divided into three categories: permissive, authoritarian and authoritative.
“A permissive parent has too few boundaries/rules and/or does not enforce them in a healthy way in the home (may be seen as a pushover).
“An authoritarian parent has too many boundaries/rules and/or may enforce them in too strict or demeaning of a manner (yelling, punitive punishments, could be seen as a drill sergeant).
“An authoritative parent has just the right balance of boundaries/rules, and enforces them consistently and with a respectful tone/approach.”
Dr. Gillet further explains, “So, a permissive parent not spanking his/her child could — along with MANY other passive and permissive parenting approaches — inadvertently teach a child how to manipulate a situation, take advantage of others, have very few boundaries, etc., which could lead to bullying.
“An authoritarian parent spanking his/her child on a regular basis could teach a child that physical confrontation is the way to solve problems and enforce differences in opinion.
“The good ol’ ‘kick the dog’ syndrome could apply here in which a child feels powerless with his or her parents, and in craving some power, determines to exert it through bullying behavior towards younger siblings or same-aged peers.
“An authoritative parent may choose to spank their child or not, and apply alongside their spanking strategy [or not] many other well-balanced boundaries/rules and ways to enforce those rules that teach their children not only to follow rules, but also how to appropriately show respect for others, communicate in healthy ways, and ultimately how not to be a bully.
“In other words, spanking or not spanking has little to nothing to do with whether a child will become a bully.”
 Dr. Gillett’s career has focused on treating both boys and girls, with specialization in trauma, processing difficulties, eating disorders, depression, anxiety, OCD and difficult family systems.
Dr. Gillett’s career has focused on treating both boys and girls, with specialization in trauma, processing difficulties, eating disorders, depression, anxiety, OCD and difficult family systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Lopolo
Sources: solsticeeast.com, www.ashevilleacademy.com
Bullying: Complaining to School vs. Empowering the Victim

If you complain to the school that your child is being bullied, will this dis-empower the victim by making him or her feel helpless?
Parents whose child is being bullied at school are in a tough spot, because on one hand, it seems that the best course of action is to report the problem to the school officials and principal.
But on the other hand, could this course make the victim feel as though they lack any power to help solve the problem?
Will this feeling of “I need help to solve all my problems” haunt them throughout adulthood?
“A sad truth about bullying is that, while no one ‘asks for’ or ‘deserves’ to be bullied, there are actually many things that the targets of bullying may inadvertently do that serves to invite, or ‘attract’ bullying behavior,” explains Kyle Gillett, PhD, LMFT, Executive Director and Founder of Solstice East and Asheville Academy for Girls.
He leads groups and conferences on bullying, helping not only victims but also the bullies.
This is not a blame the victim mindset, either. The “invitation” is a human phenomenon, and it’s evident across all age brackets, including at the workplace.
Simply compare coworkers who are harassed to those who are not, and you’ll see common threads in both groups.
Another way to understand this is to imagine you’re back in high school or junior high, and you feel like bullying a classmate. What kind of classmate would you choose?
Gillet continues, “Each situation is a little different, so a blanket statement of how to approach a situation is relatively impossible, but the truth of the matter is that both approaches (complaining to the school and empowering the bully victim) need to be taken to ensure that your child is best protected from bullying.”
Depends on the School
“Many schools these days have very active anti-bullying campaigns, and solid policies that simply do not tolerate bullying,” says Gillet.
“Other schools may not have well-developed bullying prevention strategies, or honestly may be so consumed by attempting to deal with many instances of bullying that singular requests could fall by the wayside.”
Responsibility of School
“Regardless of the situation, it is the responsibility of ALL schools to provide a safe learning environment that allows each child in attendance the ability to access an education,” explains Gillet.
“If the school is not doing this, they can be financially responsible for providing a different environment in which a child’s needs can be met. Bottom line is, the school should always be at least notified of the occurrence of bullying.”
What can parents do to help empower their child?
Gillet says that parents should educate their children as follows:
– how to identify if you are being bullied
– that it is okay and important to defend oneself if possible in unsafe situations
– how to speak to a parent or adult if you are experiencing bullying
– the importance of not just trying to bully someone back or seek revenge
 Dr. Gillett’s career has focused on treating both boys and girls, with specialization in trauma, processing difficulties, eating disorders, depression, anxiety, OCD and difficult family systems.
Dr. Gillett’s career has focused on treating both boys and girls, with specialization in trauma, processing difficulties, eating disorders, depression, anxiety, OCD and difficult family systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Lopolo
Sources: www.solsticeeast.com, www.ashevilleacademy.com
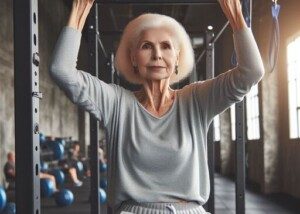
Caregivers: Prevent Back, Shoulder Pain with 3 Exercises

Here are three exercises that every caregiver should do to help prevent back and shoulder pain.
I know what the physical demands of caregiving are like due to personal experience with both parents.
And as a former personal trainer who’s had clients with back and shoulder issues, I also know which exercises are best at preventing back and shoulder pain.
If I could choose only three exercises for caregivers that would, more than any other type of exercise, prevent back and shoulder pain, they would be:
DEADLIFT

Shutterstock, Everyonephoto Studio
SQUAT


Shutterstock/BLACKDAY
BENCH PRESS

Shutterstock/Monkey Business Images
This doesn’t mean that there’s no such thing as a caregiver with back and shoulder pain who does at least one of these exercises. I’m sure there are.
Which brings me to my next point: HOW these exercises are conducted is just as important as actually doing them.
According to research by Amy Darragh, PhD, an occupational therapist from Ohio State’s School of Health and Rehabilitation Sciences, the small group of caregivers who were part of her study reported the following tasks as being problematic: transfers, toilet use, bathing, navigation of stairs and recovery from falls.
I urge all caregivers to seriously and intensely do the deadlift, bench press and squat.
I’ve been doing these for years, so when it was time to be a caregiver to my mother, I was already prepared.
However, if you’re currently caregiving and have not been working out; or, if you’ve been exercising but still suffer back and shoulder pain; or if you’re not a caregiver but foresee that one day in the future you will be — then by all means, follow my plan.
The key to the prevention of back and shoulder pain is to engage in the deadlift, bench press and squat using the following scheme: a five- to 10-repetition maximum.
This means you can perform at least five repetitions of any of these three exercises, but find that 11 at the same weight is absolutely impossible.
There are additional requirements for making these three multi-joint movements go a very long way at preventing back and shoulder pain in the caregiver:
#1. Master correct form. I can’t say this enough! Perfect form is mandatory.
#2. Be consistent. Twice a week is all you need.
#3. Warm up; don’t skimp here.
#4. Be progressive. This means don’t sit pretty at the same weight for months on end. Strive to increase the poundage over time.
#5. Crush any delusion that developing musculoskeletal strength via these exercises will result in unsightly muscles.
#6. Trust me. I took care of my elderly mother for four months after she had quintuple bypass surgery and mitral valve replacement, a pacemaker implant and two brain surgeries.
I had to deal with extreme non-compliance that was generated in part by her natural personality and also cognitive impairment that resulted from bizarre drops in blood pressure (which depleted oxygen supply to her brain).
Nobody was ever able to identify her blood pressure dives which began soon after the pacemaker implant.
But every time she exited a chair, within minutes she’d begin passing out, but not before her cognition became impaired — too impaired to realize she should have a seat to avoid fainting.
This meant I had to shadow her to prevent a fall. My father couldn’t because nine days prior to her heart surgery, he’d had back surgery and had limited physical abilities.
When my mother began passing out, no matter where she was, I had to be behind her to “catch” her and “sink” her to the floor or ground.
If I continued holding her upright, she’d pass out completely.
To restore blood flow to her brain, I had to sink her to the floor/ground.
This was done by slipping my arms under her armpits and lowering her 135-pound body gently (she was not able to assist, due to lack of wits due to the oxygen depletion) to the floor/ground, setting her first in a seated position, then leaning her back at an incline and waiting for adequate blood to reach her brain.
Sometimes during the sinking, her legs were stiff, nearly straight and non-functioning.
Once I saw her wits returning, I’d get into a squat-deadlift hybrid position, arms under her armpits, and straighten, lifting her to her feet, since these episodes would weaken her.
Once she was back on her feet, her blood pressure (mysteriously) was stable and she was able to function normally (until she sat down again for a while and then exited the chair…).
Caregivers report tremendous mental stress, and this can lead to impaired physical health of the caregiver.
Imagine my stress when my mother refused to alert me every time she exited a chair or bed. I had to keep her within my sight at all times.
But because I’m not omnipotent, during one of the few times she was out of sight (my bed was in my parents’ living room), she passed out in the upstairs bathroom while I was asleep.
I’ll never forget the sound of her head striking the bathtub. Six weeks later she underwent the first of two brain surgeries to drain a brain bleed.
I’m telling you this to establish myself as one who has experienced both the physical and mental demands of caregiving.
I once used the “sink” maneuver when my mother was passing out while trying to sit on a toilet.
I had to straddle the toilet behind her and do the maneuver, which involved a non-linear motion to get her on the floor.
If you’re strong at the deadlift, squat and bench press, you will be strong as a caregiver and be at low risk of back and shoulder pain — which I never experienced.
I did get several bad headaches and went five months without a period, but my back and shoulders never suffered.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com
Source: ccts.osu.edu/news-and-events/news/millions-informal-caregivers-risk-chronic-pain-injury-trying-help-disabled
Sudden Brief Pain at the End of Sternum: Possible Cause

Sudden brief “dings” of pain that occur in the divot at the bottom of the sternum might have a benign cause.
I can only speak from my experience, but it’s very fair to conclude that the cause of the brief “dings” of pain in that little divot between my breasts, at the bottom of the breastbone, had a musculoskeletal cause.
When you experience interesting sensations of pain or aching, you should record when this happens and anything that might have occurred that day or the day prior, so that over time, if these events keep recurring, you’ll maybe be able to see a pattern.
I began having the short sudden pain at the end of my breastbone, and had not recollected that I had documentation of this going back more than three years.
There were only a handful of notations in my health log, but as I did a “search and find” on the keyword divot, several entries popped up in the log.
The description was the same for all the entries, and there was such a long time lapse between them and my most recent episodes, that I had no choice but to conclude that it was the same benign cause.
However, I had not established a pattern for the previous incidents.
But this time, I did. It came from doing narrow to medium grip pull-downs at the gym on the “lat machine.” There was a correlation.
It seemed that whenever I had this divot pain at the end of my sternum — either earlier that day or the day before, I had done pull-downs.
The clincher came when about 40 minutes after doing pull-downs, when I was in the grocery store next door to the gym, I got sudden dings in the divot.
But why would this be happening when I’ve been lifting weights for most of my life? Well, that’s just how the musculoskeletal system sometimes behaves.
Another consideration is that I had NOT been doing any kind of pull-downs (let alone chin-ups and pull-ups) for a very long time, due to tendonitis in my elbow. So I was just getting back into heavier pull-downs.
As the tendonitis has been clearing up, I’ve been increasing the resistance on the pull-downs.
I’m able to deadlift quite a bit, but my rehab isn’t complete when the pulling is done from above my head.
If you’ve been experiencing sudden brief episodes of pain (it wasn’t stabbing or sharp; I’d call it more like a strong ache) right at the divot that’s located at the bottom of your breastbone, document when this occurs and what exercises you’ve been doing recently to see if a pattern shows up.
This isn’t about a diagnosis. It’s about documentation and seeing if an association or pattern emerges over time. This can help you should you decide to see a doctor.
If you’re dumbfounded and/or the pain gets worse or more prolonged, do see a doctor.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/ShotPrime Studio
Mole Shave Biopsy on Lower Leg Healing Time
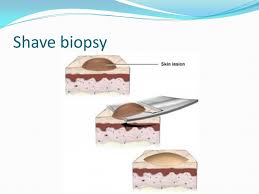
Find out how long it may take for a mole shave biopsy on your lower leg to heal.
I had a shave biopsy on my lower leg for a mole that I was concerned about (it turned out to be harmless; benign).
Sixty days later the scab was still on it and still did not look like it was ready to naturally fall off (never pick off a scab!).
It looked as though if I picked the scab off, it would bleed beneath, because it appeared that the scab was filling in a depression.
The next time I looked at the site (73 days out from procedure), which was on the front part of my upper shin, the scab was gone, and what remained was a dry, pink, very slightly depressed area.
For at least two weeks after the shave biopsy for the mole, the site still did not appear that it was healing much. It had a fresh look about it, almost raw, moist.
I also kept a Band-Aid on it all day and overnight, changing it every three to four days because every time I changed it, it seemed as though the bandage part of the Band-Aid would lift off minute particles from the site.
Finally, after three weeks, it looked like a scab was definitely beginning to form.
However, for the longest time, the site’s appearance seemed to be the same. I’d view it every three or four days when I removed the Band-Aid.
The shave biopsy for the mole either didn’t seem to be healing, or, it was healing so slowly that it was imperceptible to me.
But gradually over time, the forming-scab took on an increasingly dry, sturdy, browner appearance, and also very gradually seemed to be getting smaller.
Then it began getting a slightly crusty look—meaning that healing of the shave biopsy was continuing to progress.
“Lesions below the knee take longer to heal in everyone, particularly as we age,” says Adarsh Vijay Mudgil, MD, double board certified in dermatology and dermatopathology, and founder of Mudgil Dermatology in NY.
“The predominant reason is that circulation at the most distal parts of our body (namely below the knee) is not as robust as parts of the body more proximal to the heart; this fact intensifies as we age.”
Via e-mail, I asked my dermatologist, who performed the shave biopsy, if the fact that the Band-Aid had been covering the site for about four weeks before I decided to stop using Band-Aids, had slowed the healing time.
She said it did not slow the healing time, and in fact, it would have helped keep the site moist, which is important for optimal healing.
If you’re wondering when on earth the shaved area of your mole is going to heal…well…it may take nine and a half weeks for the scab to be ready to fall off.
 Dr. Mudgil treats infant to geriatric patients, and is versed in all aspects of medical, surgical and cosmetic dermatology. He has published extensively in the medical literature plus has lectured at numerous national meetings.
Dr. Mudgil treats infant to geriatric patients, and is versed in all aspects of medical, surgical and cosmetic dermatology. He has published extensively in the medical literature plus has lectured at numerous national meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Life Span of Morbidly Obese vs. Normal Weight People
More truth shows that there’s no such thing as a healthy extremely obese individual and that obesity cuts life span SHORT.
People who are extremely obese (class III) are more likely to have a much shortened life span than are those of normal weight.
But there is no formula for determining exactly how many years — for any particular overweight person at a given weight, height and age — will be taken off their life span.
“I generally don’t get specific with my patients about how long they will live; there are too many variables to really answer a question like that,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“I will tell them that their lifespan is likely shorter — as they are at risk to develop complications from morbid obesity over time — such as hypertension, diabetes, heart disease, liver disease and so on.”
Extreme obesity is referred to as class III, and it’s on the rise. It translates to being more than a hundred pounds over a person’s recommended weight range for their height.

A body mass index (BMI) of at least 40 is class III. “Normal” is 18.5 to 24.9.
Obesity Shortens Life Span: Study
This study comes from the National Cancer Institute, and the full report is in PLOS Medicine (July 8, 2014).
The NCI analyzed 20 studies that included adults from the U.S., Australia and Sweden.
The researchers eliminated smokers and subjects with a history of certain medical conditions to balance the results.
The risk of a shortened life span was looked at in over 9,500 subjects with extreme obesity and 304,000 who were at normal weight.
Findings
As BMI rose within the extreme obesity group, so did the risk of death overall, as well as death from most major diseases.
In the class III group, the prevalent causes of death were from cancer, heart disease and diabetes.
A BMI of 40 to 44.9 meant 6.5 years of life lost; a BMI of 55 to 59.9 meant 13.7 years lost.
Accuracy of the Study
Accuracy was contingent upon self-reported weight and height values (though if anything, this would suggest that the findings are even more alarming than they seem to be, since a person who weighs 255 pounds isn’t likely to inflate this number).
Use of BMI only, for the obesity measurement, also limits accuracy, though once BMI hits 40, you can be assured that this reflects obesity rather than a high degree of muscle mass.
It’s easy to see, without the medical research, why the people in the images above have a shortened lifespan due to their obesity.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Image source: canweallgo.com
Source: sciencedaily.com/releases/2014/07/140708153902.htm
How Safe Are Hip & Knee Replacements for People Over 80?

Here’s what you need to know if you’re over 80 and wondering if it’s worth it to have a hip or knee replacement electively. How safe is it?
It’s one thing if an 80-plus person absolutely has to have a total hip or knee replacement due to an acute injury such as from a fall or motor vehicle accident.
But what about people over age 80 who are plagued by the pain of osteoarthritis in their joints and are wondering about the mortality rates of a hip or knee replacement?
“Studies seem to indicate that total joint replacement in the elderly, provided all factors regarding the patient’s health are similar, are really quite safe,” says Barbara Bergin, MD, board certified orthopedic surgeon at and co-founder of Texas Orthopedics, Sports & Rehabilitation Associates.
“There may be a slightly higher potential for post-operative complications, which would seem intuitively apparent,” continues Dr. Bergin.
“However, when compared to the benefits of improved quality of life, increased mobilization and reduced use of pain relievers, consideration of these operations in folks over 80 is becoming a reality.”
One such study is in the Journal of Bone and Joint Surgery (July 2014), affirming that these kinds of surgeries for people over 80 are generally safe.
This applies to patients with few to zero accompanying medical conditions.

“It is especially important when we also consider the aging population, as well as the activity of the elderly now, as compared to decades in the past,” says Dr. Bergin.
“It is harder to recover from a total knee replacement than a total hip replacement.
“We have to consider the rigors of rehabilitation and a patient’s ability to comply with a program when discussing total knee replacement.
“Dementia and overall physical disability certainly influence our decision to recommend surgery.
“Not so with total hip replacements. In fact, we frequently do basically the same operation for hip fractures [when compared to hip osteoarthritis] in the very elderly, and they do quite well. They’re able to bare weight and mobilize very quickly.
“My dad had his knee replaced when he was 79. He was golfing three months later. He is now 87 and still golfing a couple of times a week!”
The BJS study, which involved hundreds of thousands of patients spanning a number of years, showed that in people with no other medical conditions/diseases (comorbidities) or only a small number of comorbidities, the in-hospital complication rate decreased significantly for total knee replacement in patients over age 80.
However, the in-hospital complication rate for total hip replacement, with these same variables, remained about the same.
For overall patients (i.e., including those with many comorbidities) over 80, the complication rate for total knee replacement went from 9.9 percent to 9.1 percent, and for total hip replacement, it went from 9 percent to 10.3 percent.
Again, these figures include the patients with more comorbidities (e.g., diabetes, congestive heart failure, poor kidney function).
The in-hospital death rate for patients over 80 who had a total knee replacement was 0.3 percent, and for total hip replacement, 0.5 percent.