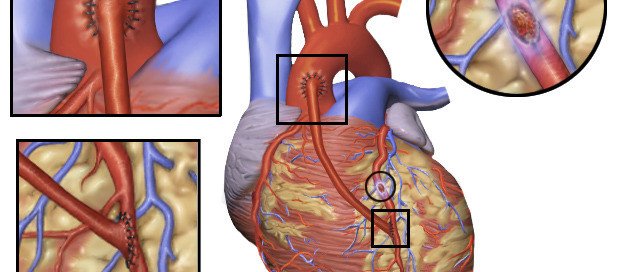
Emergency Quintuple Bypass Surgery: What to Expect
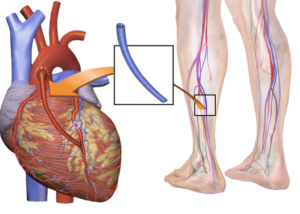
Here’s what goes on the day you’re told a family member needs emergency quintuple bypass surgery after an angiogram shows severe blockages in five major coronary arteries.
My mother was wheeled into the OR for quintuple bypass surgery two or so hours after she was told she needed the operation, and two hours after I was informed.
Imagine my shock when the worst-case scenario that I had played out in my mind had been the need for a balloon angioplasty or a stent or two.
Events Leading up to the Emergency Quintuple Bypass Surgery
My mother had chest pain two days after she had complained of shortness of breath. The first ER visit netted a “likely” diagnosis of gastroesophageal reflux disease.
The second ER visit two days later revealed an elevated troponin level, and as a result, the ER doctor (a different one this time) strongly recommended admission to the hospital.
The admission would hopefully expedite my mother’s original plans (which preceded the shortness of breath incident) to undergo a treadmill stress test.
Next day she had an echocardiogram (ultrasound of her heart). The cardiologist and internal medicine doctor said that the result was “abnormal,” and that the treadmill stress test would be unsafe.
Instead, the cardiologist recommended a catheter angiogram.
My mother refused and wanted to go home. “It would be unsafe to send you home,” said the internal medicine doctor. This doctor spent quite a bit of time convincing my mother to stay at the hospital.
My mother was mad that the catheter angiogram couldn’t be done that day, and that in order to get it, she’d have to stay another night at the hospital.
Furthermore, after reading about possible complications of a catheter angiogram, my mother refused to take the exam.
While my mother was reviewing the waiver, I was on the phone with my father, who was at home recovering from back surgery he’d had nine days prior.
He was reporting that both his legs were swollen. He told me to try to track down his surgeon to get advice, even though I insisted I drive him to the ER (he was restricted from driving) — the same ER that my mother had been in the day previous.
I tracked down the surgeon who then called my father and instructed him to go to the ER.
So I left my mother with the urging that she undergo the catheter angiogram — which by then we were told they could probably do it that day.
The 40 minute drive home took forever. Then it was back to the ER — another 40 minutes away, during which my cell phone rang: My mother reported that she was on the way to get the catheter angiogram.
Once my father was settled in the ER waiting to go to the ultrasound room, I went to the catheter angiogram floor to seek out my mother.
Shocking News
The internal medicine doctor was urgently walking down the hall and spotted me. “Oh, there you are; I’ve been looking for you and trying to call you.” (My cell phone didn’t receive well in the ER.) The doctor was not smiling. “It’s about your mother.”
I assumed there was a complication from the invasive procedure. The doctor said, “Your mother has significant disease. Her main arteries are almost completely blocked. She’s gonna need bypass surgery. Hold on…” the doctor put a hand on my arm and went off, answering a page, while my bug-eyes followed her.
Soon afterwards I met the cardiothoracic surgeon who’d be performing the operation; one by one he named the arteries that needed bypassing. I counted five by the time he was done.
He then said my mother needed a mitral valve replacement. He said a “massive” heart attack was imminent.
I asked, if my mother went home instead, could she possibly have a fatal heart attack within a week?
The surgeon, cardiologist and internal medicine doctor all in unison said “Yes” and nodded their heads.
Preparation for Emergency Quintuple Bypass Surgery
My mother was wheeled out of the catheter angiogram lab, very sedated, on a gurney that appeared to weigh 1,000 pounds.
She was taken to the surgery prep room, people bustling around her. My father had no idea what was going on, wherever he was at the moment.
Someone went down to get him. He was wheeled up to the prep room, having not been told that his wife could have a heart attack any moment and was being prepped for quintuple bypass surgery.
He was wheeled to my mother’s side and she mumbled, “I’m going to have bypass surgery.” His mouth fell open.
My mother completely recovered from the quintuple bypass surgery, which involved the heart-lung machine.
My father didn’t have a blood clot; the swelling in his legs was from inactivity.
Anyways, hope this account helps you understand what goes on the DAY someone is told they need emergency quintuple bypass surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: BruceBlaus
How Common Is Depression after Heart Bypass Surgery?

Depression after heart bypass surgery isn’t just about feeling depressed over clogged arteries, but the depression can have other related causes.
How expected or common is depression after coronary bypass surgery?
The University of Pittsburgh School of Medicine study showed that coronary bypass patients who had depression after surgery, fared a lot better with a phone-based, nurse-led care team, than did people who did not receive this added care to their heart surgeon’s standard rehab care protocols.
Study findings appear in the Journal of the American Medical Association.
However, 20 to 25 percent of patients experienced depression following coronary bypass surgery, says this outdated study that was published in 2009.
How Truly Common Is Depression after Heart Bypass Surgery?
“Patients have reported depression and memory loss after heart surgery for many decades, and initially was thought to be a result of the unnatural state of being on the heart lung machine,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“The latest data shows that depression and memory loss after heart surgery are directly related to your preop mental state,” says Dr. Fiocco.
“In other words, these patients have undiagnosed memory loss or depression coming into the surgery, and it becomes amplified post-op.
“With today’s techniques and the approach that stresses to the patient that the surgery is performed for them to return to their normal life, new-onset depression is very rare.”
Possible Cause of New-Onset Depression After CABG
Depression following CABG has been shown to impede quality of life and increase the risk of re-hospitalization.
An apparently new-onset depression that develops after coronary bypass surgery may be explained by several factors:
- Patient’s family isn’t supportive; not giving the emotional or physical support that was expected.
- There was pre-existing depression, but it had gone under the radar. The surgery has only amplified it.
- Patient becomes “bummed out” due to what lies ahead: weeks of rehab, weakness, sore chest, having to take new medications, missing work and activities, etc.
There’s nothing about CABG itself that directly causes changes in the brain that lead to depression.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: sciencedaily.com/releases/2009/11/091116192345.htm
What to Expect Hours after a Quintuple Bypass Surgery

Here’s what to expect hours after quintuple bypass surgery — and it’s not pretty.
Forget what you’ve seen on TV shows; expect the patient to look hideous.
My mother underwent emergent quintuple bypass surgery; we had only two hours to digest this shocking information; about two hours lapsed between the time I learned that a heart attack was imminent, and the time that she was wheeled into the OR.
I was told that the coronary bypass surgery would take about six and a half hours (she also had a mitral valve replacement).
My mother was wheeled into the operating room at 7 pm. At 10:30 pm, at home, I received a call that everything was going well so far, and that the first incision had actually been made at 8 pm.
At 3 am the surgeon called and said my mother had been sutured up 30 minutes prior and that there had been no complications. He said that we could stop by and see her at around 9:00 or 10 am.
What to Expect Hours After a Quintuple Bypass Surgery
We arrived about 12 noon, and the nurse told us that just a half hour prior, my mother had been extubated (breathing tube from the general anesthesia removed; she had only then begun coming out of the anesthesia).
Her face was slightly swollen, eyes closed, body immobile. Both arms and legs were swollen.
She was responsive to our presence in that she began moaning upon learning we were there but did not open her eyes.
She was able to squeeze our hands. At times her eyes opened just a bit, but were not focused.
The moans didn’t sound too good, and the nurse said they were moans to signal she was in pain.
Even though my mother had been closed at 2:30 am, and it was now noon, she had, essentially just come out of the general anesthesia and thus, appeared to be very drugged and out of it.
She spoke a few unintelligible words to the nurse, that the nurse understood; a request for more pain medication.
Above my mother was a monitor, and all around it was equipment with various tubes, and tubes went into her.
Thick tubes came out from under her legs, and pink liquid was draining through the tubes into a container.
This pink liquid was coming from her lungs. Another tube was draining urine into a urine bag.
At all times a nurse was sitting in the room at a computer monitoring my mother’s vitals.
As the day wore on, my mother’s connection to what was going on around her improved slightly.
So you can expect all of that or something very similar in the hours following a quintuple (or lower CABG) bypass surgery.
My mother was not able to carry on a conversation and was not able to hold her eyes open in a focused way.
She had absolutely no interest in eating, though she was taking ice chips, and drinking a little ice water through a straw.
She did not leave the bed once, even though the nurse did adjust the incline of the bed.
By evening, my mother was still out of it, but also acknowledged our presence.
How a patient responds, or their level of awareness, in the hours after quintuple bypass surgery will depend on their age.
Elderly people tend to “come out of it” more slowly and are far more likely to have delirium from the general anesthesia. (This is true for any type of major surgery.)
If your loved-one is scheduled for coronary bypass surgery, don’t expect much interaction or conversation the same day post-op; the patient (depending on age and comorbidities) will want to just sleep, or if awake, will much rather want to listen to you than interact.
Coronary bypass surgery is a major trauma to the body that requires a lot of procedures, anesthesia and other drugs, and thus, recovery from the anesthesia may take many hours, all throughout the day and evening.
• The patient’s temperature and blood pressure will be taken frequently and so will blood sugar.
• A respiratory therapist will come in at regular intervals
• The patient will be encouraged to do breathing exercises to open up the lungs; this is actually the standard for any surgery post-op, not just heart bypass surgery.
The ICU scene of post-op quintuple (or lower CABG) bypass surgery will look alarming, but remind yourself that the presence of fancy-looking equipment and an entanglement of tubes simply mean modern medicine at work.
And by the way, the hours following CABG will probably seem like minutes to the patient.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Rocketclips, Inc.
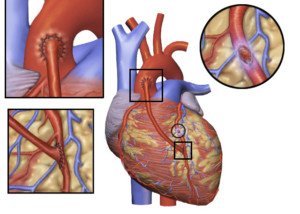
Coronary Bypass Surgery: What Patient Looks Like Right After
 After coronary bypass surgery, what exactly does the patient look like?
After coronary bypass surgery, what exactly does the patient look like?
What should family members expect to see when they walk into the ICU where the patient just arrived after undergoing coronary bypass surgery?
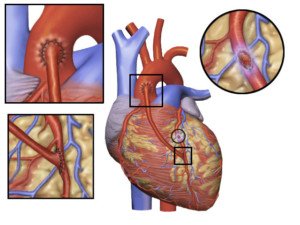
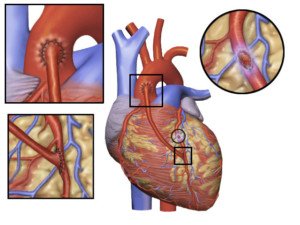
There are many variables when it comes to coronary bypass surgery (aka CABG).
My mother underwent a seven-hour operation that included mitral valve replacement, and she had five coronary arteries bypassed.
But I don’t think the way my mother looked in the ICU the day that the CABG was completed would have differed had the operation lasted only four hours.
Expect to see the following in a patient the day post-op coronary bypass surgery, and don’t be alarmed:
Swollen Legs
Swollen Arms
Swollen Face
Of course the legs will be swollen; that’s usually where the graft-vein is taken from. This is trauma to the legs and will cause fluid buildup.
The entire body is severely traumatized during CABG, and this includes the kidneys, which when normal, prevent fluid buildup in the body. Damaged kidneys will result in body-wide fluid retention.
A few days after CABG, my mother’s weight had shot up to 172. Pre-operation it was around 142. Her face was puffy and a bit discolored. The legs and arms were yellowish.
“Tubes are everywhere.”
You’ve heard this saying when someone describes a hospital patient.
You’ll think this upon seeing your family member or friend fresh from coronary bypass surgery, and all the tubes will be there while they are in ICU.
Tubing will include one for urinary output (leading to a bag on the floor) and one or two that are draining fluid from the lungs (leading to another bag).
In an episode of “The Golden Girls,” Rose is visited in her hospital room the day she has a coronary triple bypass.
If you see enough of these kinds of scenes, you’ll be that much more shocked upon seeing what it really looks like after a person has had CABG.
The “Golden Girls” scene was fake on every level. There wasn’t even an IV hookup!
Patient May Be Unresponsive
My mother’s CABG ended at 2:30 am.
It was around 12 noon when she was extubated … that is, the breathing tube from the general anesthesia was removed from her throat.
Extubation does not occur until the patient is conscious enough to follow breathing commands by the nurse.
If this didn’t happen till nine and a half hours after the CABG, then don’t be surprised if your loved-one still seems under anesthesia by the time you visit.
We visited shortly after extubation and my mother was non-conversational, could barely keep her eyes half open for more than several moments, and what few words she could say were feeble and slurred.
I’m inclined to believe that nobody just talks, like Rose did, the day post-op coronary bypass surgery.
Lots of Machines
You’ll see a lot of technology in the patient’s room and will wonder what it’s all for.
The machines are programmed to make beeping sounds when readings get to a certain point (or when medication runs low), such as blood pressure too low, heart rate too fast or heart rate fluctuating.
I will never forget the sound of the beep that signaled that my mother’s heart was “popping into” atrial fibrillation. This kept happening.
It got to a point where if I heard this same kind of beeping coming from another room, I’d get unnerved.
But after a while the occurrence became routine, and I became more desensitized to the beeping.
In summary, what a patient looks like right after, and even two or three days after, coronary bypass surgery is not pretty.
Expect lots of swelling, “thunder thighs” on a woman who, pre-surgery, had trim thighs, and arms “twice their normal size.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/BruceBlaus
Is 90s Too Old for Coronary Bypass Surgery?

Coronary bypass surgery is actually becoming more and more common in very old people.
Thousands of people in their 90s have had heart bypass surgery, also known as CABG.
People over 90 Years of Age Having Coronary Bypass Surgery
The American Journal of Cardiology has a paper endorsing coronary bypass surgery in people 90 and older. And this paper was published in 2007.
So more than ever today, your 90-something parent, grandparent or spouse may be a good candidate for CABG.
Look What the Study Says
The subjects for the study were 4,224 Medicare patients in their 90s who underwent heart bypass surgery between 1993 and 1999.
The patients were followed up for five years after their CABG procedures.
Interestingly, the women in the study had better survival rates than did the men.
However, this may have been because the women, who comprised 50 percent of the CABG patients, were more likely to spend time rehabbing in a nursing home as a transition, than were the men.
Can Just ANY Person 90 or Over Get Heart Bypass Surgery?

“When I first began doing cardiac surgery, we looked at 80 year olds as too old for surgery,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Now we operate on them all the time. I have operated on several 90+ year olds — but they must be robust, active and without dementia.
“Physiological age is much more important than chronological age.”
Carefully selected people in their 90s can benefit quite a bit from heart bypass surgery.
Suppose someone is 92 but has well-functioning kidneys, normal blood pressure without medication, and the only thing wrong with their heart is that the main arteries are 99 percent blocked.
Now let’s suppose we have a 75 year old who also has 99 percent blockages.
But in addition, this person requires medication for blood pressure control — and has moderate chronic kidney failure secondary to chronic heart failure.
The 92 year old will make the much better candidate for CABG.
Emergency Bypass Surgery
Another point to consider is if the heart bypass surgery is determined necessary on an emergent basis, versus as a planned treatment option for severe coronary artery disease.
In the case of an emergent basis, the elderly patient may be told that a massive heart attack is imminent without the CABG procedure.
According to the American Heart Association and the American College of Cardiology, a patient should not be considered too old for coronary artery bypass surgery based strictly on age alone, because potential long-term benefits must be weighed against the risk of the procedure.
Thus, a person who’s 95 but in otherwise good health (e.g., no diabetes, nonsmoker, healthy body weight) may actually be a better candidate for heart bypass surgery than a 70-year-old smoker who’s obese and diabetic.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: sciencedaily.com/releases/2008/02/080202124039.htm
Survival Rates of Elderly Bypass Patients after Heart Attacks
An elderly person suffers a heart attack and undergoes coronary bypass surgery.
How long are they expected to survive on average?
Is the bypass surgery even worth it for a very elderly person?
Heart bypass surgery in the elderly following heart attacks is becoming more common, but there has been little research into the mortality rates for this population.
Coronary bypass surgery is also known as revascularization.
A study in the Canadian Medical Association Journal (2010) reports that coronary bypass surgery in the elderly after a heart attack can improve survival rates — but the study forecasts the improvement out to one year.
There isn’t a whole lot of data on the impact of coronary bypass surgery on the elderly who have suffered a heart attack.
The researchers in this particular study wanted to investigate the trends in the use of revascularization and medication prescriptions in the elderly, over a span of 10 years.
The research involved over 29,000 patients at least 80 years old.
This is one of just a few investigations into long-term mortality developments in the elderly who’ve had a heart attack.
First author of the study, Maude Pagé, explains, “We found that the rate of one-year mortality after a heart attack decreased from 48.4% in 1996 to 30% at the end of the study in 2006.”
It’s important to note that the data may be influenced by the fact that elderly patients have been arriving at hospitals sooner over the years.
Nevertheless, the data indeed reflects the increasing use of coronary bypass surgery for people who once were considered too old for revascularization.
Coronary bypass surgery is becoming more common in people even over the age of 90, with favorable outcomes.
“There is great physiologic variability in the older group and the published results of surgery in the elderly do not support prejudice based on age,” says Dr. Mark Katlic, of Geisinger Health System.
“There is no age in isolation that contraindicates surgery, although ageism exists. Many groups have shown that excellent results are attainable with compulsive attention to detail.”
Risk factors for heart disease, which can become severe enough to require coronary bypass surgery (revascularization) go well-beyond the highly publicized obesity, smoking, lack of exercise and emotional stress.
Here are additional risk factors for heart disease: poor sleep, which includes excessive sleep; excess belly fat, despite thin limbs; having a hostile or argumentative nature; poor oral hygiene; and having panic attacks (at least in postmenopausal women).
The need for coronary bypass surgery does not occur overnight. It takes years to develop.
Thus, it would seem that the need for revascularization could be prevented in many people if they began heart disease screening early on in their adult life, rather than waiting till they were elderly to get things taken care of.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Alexander Raths
Source: sciencedaily.com/releases/2010/08/100803132732.htm
How to Prevent Weight Gain from Caregiving Stress

Here’s a no-nonsense way to outright prevent gaining weight no matter how stressful your caregiving tasks are, no matter how demanding your charge is.
I’m an exercise and fitness enthusiast, and former personal trainer, who had the experience of “extreme caregiving” for my 80-something mother during her numerous serious medical situations (severe depression, quintuple bypass surgery, constant fainting episodes, two brain bleeds and a hip fracture).
Food Provides a Relief from Caregiver Stress
A caregiver will often turn to food for comfort (and thus gain weight); the mental angst can be unspeakable.
Another reason a stressed-out caregiver may gain weight is because the time required to keep up with a supply of healthful food, and then to prepare healthful dishes, is no longer present.
Convenience-eating translates to junk food eating. Feelings of powerlessness encourage the stressed caregiver to eat well-beyond the point of satiation, and weight gain happens.
During my first round of caregiving (my mother had knee arthroscopy followed by crippling depression) I subsisted almost entirely on junk food and ate like a horse, while staying with my parents to take care of her.
Alongside that, I was battling against my father’s poor judgment as far as what should be done with her (e.g., he kept denying that she had full-blown depression and hence, was an obstacle to antidepressant treatment).
There were many trips to IHOP, Village Inn and Perkins (my mother was too disabled to cook).
Whenever we went out for breakfast I’d order the same thing: French toast, drenched in butter and syrup. I had given up cardio exercise and gained weight (around 15 pounds), but had continued lifting weights.
A small amount of “stress weight” is one thing, but a LOT of weight gain (i.e., 15 or more pounds) doesn’t have to happen. Never take up smoking to prevent this!
- Do NOT quit exercising just because you’re seeking comfort through food!
- Do NOT quit exercising just because you’ve gained some weight.
Though I lived on large quantities of junk food, this was no excuse for ditching the weight workouts. I ditched the cardio, but the weight workouts were far more valuable.
The stressed caregiver needs to get away, and when possible, should use that time wisely: a gym workout will do much more good than a trip to a bar to “unwind.”
Gym workouts, rather than spending inordinate amounts of time on social media, will help prevent weight gain or at least help prevent more than 15 pounds of weight gain.

Freepik.com
Exercise can also include yoga, which may sound too passive, but a yoga class–if your gym offers one–will provide a unique challenge to your body. This beats unwinding with “a few drinks” any day.
My mother completely recovered, I moved back home, resumed cardio, stopped living on junk food, and quickly got my lean physique back.
Second Caregiving Stint: No Weight Gain
Less than a year later…another tour of duty…the quintuple bypass surgery. The ensuing four months were a nightmare.
Somehow, someway, I made the time to do all my shopping at Whole Foods and eat a plant-based diet with minimal junk food. I continued cardio and never missed a weight workout.
There were many trips to restaurants, and I almost always ordered something healthy like grilled salmon, broccoli and a salad.
I always had to go with my parents to restaurants because my mother was prone to passing out, and my father, being a senior citizen with recent back surgery, was in no condition to support 135 pounds of fainting weight.
Throughout the stress of this second round of caregiving, I dropped 10 pounds in its first 30 days, despite eating more food than usual.
The emotional strain was enormous (my mother was non-compliant), but the one thing that gave me a sense of control was eating healthfully and stopping at the point of satiation.
So you see, if you put your mind to it, weight gain from caregiving CAN be prevented. A few pounds are okay, but there was no excuse for my 15 pound weight gain during that first stint.
Caregiver stress is all the more reason why the individual should stick to a rigorous exercise regimen and make every effort possible to eat healthfully.
By not gaining weight, you will feel more in control amid what seems to be a very out-of-control environment.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: pexels-liza-summer
Why Grown Kids of the Super Obese Keep Bringing Food to Them

Why do the grown kids of the super morbidly obese who can’t even walk across a room keep bringing them giant portions of junk food?
Bringing enormous amounts of food to one’s 900 pound parent is like bringing caseloads of whiskey to someone with liver disease.
Renee Williams weighed about 900 pounds before she died, and the TV show depicting her life at this weight revealed that she lived with her two daughters, which made me wonder:
What enablers kept bringing this bedridden, essentially paralyzed woman all the food?
An online Daily Mail article (among other sources) notes that Williams would eat eight hamburgers in one sitting.
Her eldest daughter reported that Williams would eat till her stomach hurt.
Were her daughters participating in the enabling, bringing their mother some of the junk food she’d gorge on?
960 Pound Woman, Confined to Bed for Years, Didn’t Get that Way without Enablers
When I watched Williams’ story on TLC (“Half-Ton Mom”), the topic of who keeps bringing her so much food wasn’t dare broached, but the viewer could easily infer that Williams’ daughters were partially involved, simply because they were old enough to bring her food.
Presumably, at least one adult was part of the enabling process, since the daughters weren’t old enough to drive. It’s also possible that Williams received a large percentage of food from delivery people.
However, her oldest daughter, at the time of the TLC airing, was about 14 — old enough to take a stand against allowing excess food to get near her mother, who wasn’t even able to sit up in bed.
“It is common for adult children of addicts to develop their own addictive patterns,” says David Sack, MD, a psychiatrist specializing in addiction disorders, and CEO of Promises Treatment Centers in Malibu and Los Angeles.
“Many struggle with people-pleasing, an overdeveloped sense of responsibility, and fear of rejection or abandonment, which often manifests as codependency and enabling.”
Son Kept Taking Food Orders for Severely Morbidly Obese Mother
Another TLC program focused on a man about 19 who was shown leaving the house for and returning from food runs for his severely obese mother.
His mother was able to walk short distances in the house but not able to venture out shopping.
He’d bring her bags of candy bars, fastfood and other unhealthy items in alarming quantities, totally helpless at saying “No, I will not help you commit suicide!”
What’s odd is that it was not revealed what kind of stranglehold Williams had over her daughters, or what the second mother had over her adult son, that made it impossible for them to suppress the influx of food.
The mothers were never shown throwing temper tantrums or threatening to stop loving their kids.
Dr. Sack explains, “We often see adult children make excuses for a parent’s addiction or look the other way because they don’t want to disrespect or embarrass their parent, or perhaps they feel the parent has earned the right to behave as they please. Often, they’ve lost hope that change is possible.”
 Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Source: dailymail.co.uk/news/article-505198/The-half-ton-mum-Tragic-story-worlds-heaviest-woman.html
Morbidly Obese Reality Shows Ignore the Enabler Issue

Why don’t TLC shows about massively obese people confined to bed ever explore why their family members keep bringing them food?
Over the past several years there’s been quite a few TLC programs focusing on people weighing close to 1,000 pounds, showing gruesome footage of their gastric bypass surgeries and other unsightly details.
Yet not once spending some time visiting the enabling aspect of these situations — the enabling spouse or family member who keeps bringing tremendous amounts of food to their super obese loved-one who cannot get out of bed.
Is TLC afraid to broach the enabling component of super morbidly obese people?
Does TLC think that viewers would rather watch the surgeons slice away at grisly layers of fat to rearrange intestines — a most ghastly sight — than hear from the enabler why he or she is an enabler? These surgery scenes are extended.
The viewer doesn’t expect the enabler of super morbidly obese people to give a Freudian explanation; we just want to hear what they have to say — why they find it so difficult to just say no to the food addict.

What is TLC afraid of?
“Part of the problem is lack of awareness,” begins David Sack, MD, a psychiatrist specializing in addiction disorders, and CEO of Promises Treatment Centers in Malibu and Los Angeles.
“The public, and even the mental health field, has been slow to recognize that food can fuel addictive patterns in much the same way as drugs like heroin and cocaine.
“Just as family and friends can enable drug and alcohol abuse, they can become enablers to the food addict or compulsive overeater.”
TLC should devote an entire program to investigating enablers of obese family members who are confined to bed.
This would be far more intriguing than listening to the surgeon give commentary as he examines various folds of fat on the patient’s back.
“There also may be a reluctance to point the finger at people who, at least on the surface, appear to be trying to help,” says Dr. Sack.
“In many ways, obesity enablers are hostages and victims in their own right and require compassion and treatment just like the addicts they’re enabling.”
Nevertheless, I was so angry at Cheryl for becoming irate when a surgeon told her she had to help her 900 pound husband, Ricky Naputi, lose 100 pounds before he could qualify for surgery.
She stormed out of the room upon hearing this requirement.
But TLC didn’t explore why she reacted this way. It would have been LESS work for Cheryl to help Ricky lose weight — less food shopping, less food preparation, less cleaning, less money spent.
Why was she so mad? TLC owed viewers an explanation instead of leaving us hanging.
Maybe Cheryl was asked off-camera and refused to answer?
But what about the many other enablers? Do ALL of them refuse to share their insight about their enabling ways, yet have no qualms about revealing other issues such as no sex life or past sexual abuse?
Or perhaps some enablers have begged TLC to spend some time on the enabling issue, but TLC refused?
It’s anyone’s guess, because this component of the super morbidly obese lifestyle is kept well-hidden.
The only case I’m aware of in which the enabling was significantly focused on was the riveting case of Billy Robbins.
Much of the show centered on why his mother overfed him since childhood, such that by age 18, he weighed 800 pounds and spent most time in bed.
“Enabling is a topic morbidly obese individuals and their caretakers may be loathe to talk about because of the shame and confusion they feel,” says Dr. Sack. “They may avoid seeking help for fear of judgment from others.”
 Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Source: nydailynews.com/life-style/health/world-fattest-man-died-900-pounds-article-1.1353829
Enabler of Super Obese Family Member: Might YOU Become One?

Are you at risk of ever becoming an enabler to a family member who eventually gets so super morbidly obese that they can barely get out of bed or are even confined to bed?
They are being maintained in this condition by enablers (usually a spouse or family member) who keeps bringing them enormous amounts of junk food.
I’ve noticed that in every single case (and I’ve seen quite a few of these shows), the enabler is obese, often morbidly, but functional enough to be a caregiver/enabler.
I just can’t imagine that anyone who works out at a gym, has a physically fit body and eats mindfully could ever become an enabler such that eventually, their “enablee” gets too heavy to leave their bed.
You’ve heard of the “addictive personality” or “addictive brain.” Is there a such thing as an “enabler personality” or “enabler brain”?
Many women refuse to serve their husbands the amount of junk food they request; perhaps they are “anti-enablers”?
Though most functional obese people aren’t enablers, most enablers on the TLC shows are quite obese and don’t do any exercise.
It’s easy for me to believe, just based on the behavior of the enablers, that most were abused as children, or grew up in an emotionally corrupt household, stripping them of the capacity to engage in an emotionally and physically healthy adult relationship.
Inside the Mind of a “600 Pound Life” Enabler
“Anyone can become an enabler, but those with low self-esteem or who have difficulty saying no, expressing feelings, or setting and maintaining personal boundaries are most at risk,” says David Sack, MD, a psychiatrist specializing in addiction disorders, and CEO of Promises Treatment Centers in Malibu and Los Angeles.

More Risk Factors for Becoming an Enabler to a Super Obese Person
“Enablers believe they are bad or cruel if they don’t help and are afraid of what might happen if they don’t,” continues Dr. Sack.
“They feel compelled to take on other people’s responsibilities, sometimes out of guilt or fear, but also in an attempt to gain control.”
Enablers or those at risk put the needs and desires of others ahead of their own. This may sound noble, but when it leads to disaster, it’s destructive.
“In an attempt to protect themselves from victimization, they prefer to keep the peace than address the problem and deal with the potential fallout,” says Dr. Sack.
This begs the question: How extensive could the fallout be, when the bedridden food addict can’t get up and do anything?
What kind of frightening fallout was sweet, loving, 900 pound Renee Williams capable of inflicting upon her children if they stopped bringing her huge amounts of food?
“Most people learn codependent behaviors from their role models growing up, especially if they were raised in an addicted or dysfunctional home,” says Dr. Sack.
“Others may suffer traumatic experiences early in life, which contribute to low self-esteem, a fear of abandonment and other codependent traits.”