Can You Die from a Single LPR Choking Episode?

Though untreated LPR can lead to fatal esophageal cancer, can you choke to death from one “I can’t breathe” episode of laryngopharyngeal reflux disease?
LPR causes many symptoms, and one of them is a sudden sensation that the airway has become constricted, making it difficult to INhale air (though there’s no problem exhaling).
It feels like you’re inhaling through a straw, and the sufferer may think that they’re going to die.
“The patient needs to relax; people do not die from these symptoms, as scary as they may be,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
Though LPR has been suggested as a cause of sudden infant death syndrome, this has not been proven, and SIDS continues to remain a mystery.
Furthermore, the 50 million Americans afflicted with LPR do not have to worry about choking to death or passing out and never awakening from the sudden feeling that they can’t breathe.
During such an episode, try panting heavily like a dog; that might restore normalcy.
Otherwise, stay calm and wait it out.
Dr. Silvers explains, “The patient can take some liquid Gaviscon which is fast acting to suppress the reflux and coat the throat (the European Gaviscon is best and can be purchased online).
“The patient should see an ENT who will confirm the diagnosis of LPR or silent reflux. Avoid late night eating; this is the number one trigger of nighttime breathing and choking symptoms.
“Acid reflux will worsen sleep apnea, and in some patients will cause their sleep apnea.”
A wedge to allow an elevated sleep position will help. It’s also possible that a person’s LPR can be caused by a problem with the diaphragm or the esophageal sphincter.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Aaron Amat
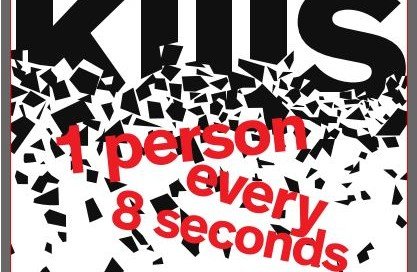
Why Does Diabetes Kill So Many If It Can Be Controlled?
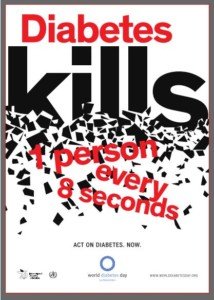
If diabetes can be controlled, why do so many Americans die from it every year?
According to the National Diabetes Statistics Report, 2014, diabetes was the seventh leading cause of death in the U.S in 2010 (over 69,000 deaths).
In that year there were over 234,000 death certificates listing diabetes as a contributing or underlying cause of death.
Diabetes is also a leading cause of blindness and amputations in U.S. adults.
This disease, as you can see, is very destructive. However, diabetes can be controlled. Have you ever heard someone say, “I have type 2 diabetes, but I control it with diet and exercise?”
Since type 2 diabetes can be controlled with diet and exercise, why do so many people die from it and even more develop serious complications leading to disability?
As for type 1, this, too, can be controlled, but requires daily injections of insulin.
Difference Between Type 1 and Type 2
In type 1 (10 percent of all cases), the pancreas fails to produce insulin—a hormone that shuttles blood sugar to muscle cells. The result is too much sugar in the blood.
In type 2, the pancreas works fine. The problem is with the insulin receptor sites on muscle cells:
They don’t work efficiently, and/or there’s not enough of them. The result is too much sugar in the blood.
Controlling Diabetes
Insulin injections provide insulin so that the blood sugar can be taken to the insulin receptor sites.
Exercise lowers blood sugar by forcing the muscles to demand more sugar.
Those with type 1 can exercise all they want, but without insulin, there’s nothing to shuttle the blood sugar to their muscle cells.
Diet is important: Too many refined carbohydrates, especially all at once, overload the blood with sugar.

“Although it can be controlled, it does not mean that most people do a good job,” says John Whyte, MD, board certified internist in Washington, DC, and author of “Is This Normal? The Essential Guide to Middle Age and Beyond.”
This is easy to believe. I used to work at a place where there were two diabetics.
One pedaled hard every day on a stationary bike, kept his weight in check and watched what he ate.
The other was overweight and was frequently seen eating junk food.
Dr. Whyte explains, “Diabetes is a progressive disease — which means that beta-cells in the pancreas which are responsible for insulin continue to ‘burn out.’ Changing our diet and taking medicines can slow that down, but all too often patients either don’t take their medicine as directed, or they don’t make changes to their lifestyle.
“It can be hard to make the healthy choice if you’ve grown up with processed foods and a love of candy!
“And if you have always been a couch potato, one doesn’t change overnight.
“I always get frustrated when patients are very reluctant to start insulin, and then after a few months, their diet gets worse since they learned [incorrectly] if they eat a cupcake, they can just take more insulin.
“So the reality is that we see far fewer complications when patients have good control. But we’re not doing a good enough job helping patients understand the importance of daily control.”
Controlling diabetes also means regularly checking blood sugar levels. Many people neglect to do this when they should.

Dr. Whyte is the chief medical officer of webmd.com. Prior, he was the chief medical expert for almost a decade at Discovery Channel.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Scalp Tenderness Above the Ear: Doctor Explains

A medical doctor answers what may cause scalp tenderness above the ear.
Many people want to know what might cause tenderness or soreness, even pain, on or in their scalp above the ear.
“In terms of scalp tenderness, there are a range of diseases and conditions for which this could be a harbinger,” explains John Whyte, MD, board certified internist in Washington, DC, and author of “Is This Normal? The Essential Guide to Middle Age and Beyond.”
Dr. Whyte continues, “But the reality is that most of the time it is related to tension headaches.
“We think of herpes as a condition that primarily affects our mouth or genital areas, but herpes zoster actually can cause tenderness of the scalp.
“One of the most serious conditions which can cause scalp tenderness is temporal arteritis.
“This is a condition which results in swelling of certain arteries in the head, typically around the eyes, but can also affect the side of our heads.
“There are almost always other symptoms such as vision changes and jaw pain. This is a medical emergency and needs to be evaluated quickly.”
Don’t panic if you discover some tenderness on or in your scalp above an ear.
First ask yourself if you bumped your head in that location within the past few days.
There could be a bruise from skin trauma — the same kind of bruise that would appear on your thigh if you accidentally rammed your thigh into something sticking out; after a few days the skin is still tender to the touch.
Another possible, and very benign, cause of tenderness at the scalp above an ear is the result of aggressive hair brushing.

Shutterstock/Image Point Fr
You should try a softer brush. Brushes with natural bristles or wide-tooth combs are generally gentler on the scalp compared to those with stiff or plastic bristles.
When you’re brushing, be mindful of your technique. Use gentle strokes and avoid yanking or pulling hard on your hair.
If you hit a knot, try to gently work through it with your fingers before reaching for the brush.
This approach can prevent unnecessary strain on your scalp.
The hair has nothing to do with this pain or soreness.
It’s the bristles of the brush making aggressive contact with the skin of the scalp.

Dr. Whyte is the chief medical officer of webmd.com. Prior, he was the chief medical expert for almost a decade at Discovery Channel.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Is It Bulbar ALS or Normal Tongue Twitching?

A neurologist explains why constantly examining your tongue for Bulbar ALS doesn’t make sense.
Your tongue is twitching, you Googled twitching tongue, and now you’re terrified you might have bulbar onset ALS, because the bulbar onset version of this awful disease can involve a twitching tongue.
You’ve been giving your tongue all sorts of strength tests, such as quickly moving it back and forth, pressing it against the roof of your mouth and so on.
Being that ALS references show up on the first page of keyword search results of tongue twitching, it’s no wonder that you’re now freaking that you might have ALS.
It certainly doesn’t help that the second page has several more ALS links regarding tongue twitching.
Ironically, the first two pages of the search results also reference nonfatal causes of tongue twitching.
But it’s human nature to fixate on the worst possible explanation, even though bulbar onset ALS, whose symptoms indeed can include tongue twitching, strikes about 1,375 Americans every year. This makes bulbar onset ALS an extremely rare disease.
However, the fact that it shows up amply in search results for tongue twitching creates the illusion that it’s more common.
“If a person is really worried about having bulbar onset ALS,” says Kristina Lafaye, MD, “inspecting the tongue is not the exam to perform.”
She adds: “If they do not have any problems with swallowing, chewing, or controlling their secretions, then they do not need to bother looking at their tongues.”
Dr. Lafaye is a board certified neurologist specializing in clinical neurophysiology and neuromuscular medicine with Tulane Doctors Neurosciences.
“Bulbar onset is marked by problems swallowing, chewing, and controlling secretions,” Dr. Lafaye points out.
“There is coughing and a perception of food (liquids) ‘going down the wrong way.'”
She emphasizes that development of these symptoms is “subtle” and not an overnight process.
Search engine results do not correlate with how common a disease is.
They only indicate how often it’s written about, and/or how crafty the keywording of the article is.

Shutterstock/El Nariz
Effective search engine optimization and latent semantic indexing will help get an article at the top of the search results.
Don’t let that fool you into believing that your twitching tongue means you might have bulbar onset ALS.
The first two symptoms of bulbar onset ALS are speech and swallowing difficulties.
When scared people, who Googled tongue twitching, learn this fact, they feel relieved, but the relief is often short-lived, because soon, the person then starts perceiving difficulty speaking and swallowing.
Attention then turns to talking and swallowing. Nevertheless, the tongue continues to twitch, often more than ever, panicking the person.
Bulbar onset ALS progresses rapidly, but an anxiety-stricken person can remain terrified of bulbar onset ALS on a chronic basis, even though after months and months, the only symptom he or she has is the twitching tongue.
The person has “molded” their mind into thinking a certain way, and it’s virtually impossible to just snap out of it.
The best treatment for this hypochondria affliction is behavior modification, and visiting new perspectives.
Suppose you know that 1,375 Americans every year get zapped by aliens into thin air, but a year before this happens, the selected victims experience a normal headache.
Would this mean that every time you had a headache, you’d freak out and feel convinced that the aliens have you on their zap list?
Probably not, especially since you know that millions of people suffer headaches every day, and there are over 300 million people in this country.
You’d recognize the astronomically low odds that the aliens would ever zap you.
Yet, this same kind of thinking does not take place with people scared out of their wits that, due to a mere twitching tongue, that they probably have bulbar onset ALS.
Maybe it’s because a twitching tongue is a stranger symptom than a headache.
We grow up hearing about headaches. We hear about headaches all the time, everywhere. They are part of our culture, part of living, and part of our vernacular.
How often do parents tell their kids, “You’re giving me a headache!” Headaches are the topics of jokes and humor.
But tongue twitching? What is THAT? Seems mighty odd. But it shouldn’t be. After all, the tongue is a muscle.
And muscles twitch — millions of times in millions of people EVERY DAY. A twitching tongue shouldn’t frighten you any more than should a twitching calf muscle. The tongue is a muscle.
Nonfatal Causes of Tongue Fasciculations
– Anxiety (which may initially be due to factors unrelated to health, such as money or relationships)
– Fatigue
– No known cause other than sometimes, muscles just twitch
– Benign fasciculation syndrome (annoying muscle twitching disorder)
– Side effects from some medications
– Mineral imbalance, particularly calcium/magnesium deficiency
– Dehydration
– Dystonia (neurological movement disorder)
– Bulbar onset ALS – but realize THIS: About four out of every 100,000 American people will be diagnosed with ALS. Bulbar onset comprises 25 percent of ALS victims.
This means that it would require up to 100,000 people before a new diagnosis of bulbar onset ALS was made.
You can’t live your life as though you are that one (or four) person out of 100,000.
You are over 30 times more likely to die in a car accident this year than get bulbar onset ALS.
So next time your tongue twitches, relax, take a few deep breaths, and promise yourself you will stop examining your tongue in the mirror.

Dr. Lafaye is triple board certified: neurology, clinical neurophysiology and neuromuscular medicine from the American Board of Psychiatry and Neurology. Her expertise and leadership continue to make a significant impact on patient outcomes.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/MCarper
Sources: nlm.nih.gov/medlineplus/ency/article/003296.htm & cdc.gov/mmwr/preview/mmwrhtml/ss6307a1.htm
Can Middle Age Cause Your Ankles to Swell?

Have you noticed that lately your ankles appear swollen and you’re wondering if this is due to middle age?
“As we get older we may see swelling of our ankles — usually near the last half of the day especially if we stand or sit for long periods,” says John Whyte, MD, board certified internist in Washington, DC, and author of “Is This Normal? The Essential Guide to Middle Age and Beyond.”
Why does this happen?
“We have valves in our veins which typically prevent pooling,” says Dr. Whyte.
“But as we get older the valves don’t work as well or get damaged. Gravity takes control and therefore we have some pooling.
“Fluid due to aging typically resolves by morning; it is usually a small amount; it is never accompanied by difficulty breathing and usually occurs in both ankles/lower legs.”
An assortment of medical conditions can cause fluid buildup in the lower legs and around the ankles, even the feet. Have a medical doctor check the swelling in your feet.
Nurses, too, have a lot of experience with this presentation and are very knowledgeable of it.
If your socks are leaving “imprints” of their patterns in your skin, this most likely is nothing to be alarmed about.
A rubber band around your wrist, left there for a while, will also leave an imprint.
Aging and Your Skin

Shutterstock/Elvira Koneva
As people age, the skin undergoes various changes that contribute to its loss of elasticity and firmness, commonly referred to as losing its “bounce.”
This phenomenon primarily results from a decline in the production and quality of collagen and elastin, two proteins crucial for maintaining the skin’s structure and resilience.
Collagen provides strength and support, while elastin allows the skin to stretch and return to its original shape.
With age, the production of these proteins decreases, and the existing ones become more fragmented and less effective.
In addition to the decline in collagen and elastin, the skin’s ability to retain moisture diminishes over time.
This is partly due to reduced production of hyaluronic acid (“HA”), a substance that helps maintain skin hydration and the so-called plumpness.
As the skin becomes drier, it loses its softness and suppleness, contributing to the formation of fine lines and wrinkles.
The loss of bounce or firmness in skin, as people enter middle age, should not be confused with fluid buildup, swelling or edema.

Dr. Whyte is the chief medical officer of webmd.com. Prior, he was the chief medical expert for almost a decade at Discovery Channel.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can Statin Drugs Undo a Bad Diet?

Don’t think for a second that taking statins means you can eat lots of junk food and not worry about that causing heart disease.
Can statin use counteract the damage caused by bad eating habits?
“That’s a great question because I see this play out in practice all the time,” begins Dr. Elizabeth Klodas, a board certified cardiologist and co-founder of Step One Foods.
“People get really complacent about what they eat when they’re on a statin, because no matter what they do, their ‘numbers’ are perfect. But you have to remember that cholesterol readings are only one small clue as to what is going on inside your body.”
Statins vs. Healthy Diet
Dr. Klodas explains, “A good way to think about this is to consider exercise and eating Twinkies. You can get rid of the calories inside a Twinkie by exercising, but you can’t get rid of the biochemical effects that the sugars, fats and preservatives have on all your cells.
“It’s the same with statins and Twinkies. You can mitigate the effects of the sugars and fats on your cholesterol numbers, but you still can’t get rid of the biochemical effects of those same sugars, fats and preservatives on all your cells and you certainly can’t get rid of the calories.”
Think about how long a Twinkie’s shelf life is—superpreservatives!
“Whenever I put someone on a statin I always point out to them that I can make virtually anyone’s cholesterol numbers perfect if I just put them on enough medication.
“But unless they are doing their part in terms of what they eat and how much they exercise, all I’m doing is putting very pretty (and often very expensive) wallpaper over crumbling walls. It may look great, but we really haven’t fixed anything.”
It’s like the analogy with firefighters. You know a fire is nearby. But knocking down the firefighters doesn’t mean the fire disappears.
Statins knock down cholesterol and bad fat numbers, but this doesn’t mean that the inflammation inside the coronary arteries goes away; it’s still raging.
Dr. Klodas continues, “Unfortunately, wallpaper over crumbling walls is too often the norm in medical practice, and many people are placed on statins without first being given the right tools to mitigate the need for these medications.
“This is why I came up with Step One Foods. I wanted to make it really easy, essentially goof-proof, for people to start fixing the walls.”
Statins are easy to take; just pop the pill at bedtime with some water. People want the easy route.
My brother takes statins and has “great numbers,” but eats a lot of processed foods.
Those numbers aren’t the innards of the wall; they are merely the superficial pretty wall paper.
Trained at Mayo Clinic and Johns Hopkins, Dr. Klodas believes in first changing the diet, rather than taking pills, to improve cholesterol profile.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Why Your White German Shepherd Is Losing Patches of Fur

A common household product may be what’s causing your white German shepherd to be losing chunks of its beautiful fur.
A veterinarian can overlook this cause, as was the case of our dog!
When my parent’s white German shepherd was a young adult, he began to mysteriously begin losing patches of his gorgeous fur.
We started noticing that his fur was falling out in certain areas. It was not a diffuse or evenly-distributed loss of fur. There were bare patches here and there.
I came up with the solution, but not before we took the white German shepherd in for a visit with the veterinarian.
The veterinarian couldn’t come up with an explanation. He sent us home with nothing to work with. Soon after, my cousin visited and suggested adding white rice to his diet.
This was part of her own diet, which she said put her multiple sclerosis into remission.
The white rice failed to remedy the problem.
An idea then struck me: Only an allergic reaction could cause fur loss in a dog.
The idea of an allergic reaction had come up before with the veterinarian, but it only went as far as that.
Just what the white German shepherd could be allergic to was never explored.
But I began noticing that the fur loss was in the very areas that the dog would lie on when on his big doggie pillow.
I also knew that periodically, my mother took the cover off the pillow and washed it in the washing machine — with standard laundry detergent.
“I bet he’s allergic to the laundry detergent!”
I added, “There’s a chemical from it in the pillow covering. He lies on that very often, and it can’t be coincidence that he’s losing fur in the very areas of his body that make contact with the pillow!”
I told my mother to start using a hypo-allergenic laundry detergent. Once she switched to the hypo-allergenic brand, the fur began growing back in!
My mother initially thought that it was “the diet” that my cousin had recommended. But eventually, my mother got tired of preparing all that rice and stopped giving it to the dog.
Despite that, the fur loss never recurred! This meant that the rice had no effect on the fur growing back in, and that it had to be an allergic reaction to the laundry detergent.
There’s a reason why there are hypo-allergenic versions of laundry detergents.
Many people, and dogs, are allergic to the chemicals in standard products.
Our German shepherd never again suffered from the loss of his beautiful white fur.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Teen Has Skipped Heartbeat with Breathing Problems
If your teenager has a “skipped” heartbeat and problems breathing, what might this possibly mean?
A teen may experience what seems like a skipped heartbeat from anxiety, but trouble with breathing adds a whole new dimension to the sensation.
“A teen with these complaints needs to be evaluated for congenital heart disease, abnormalities of heart rhythm and lung disease,” says cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
He adds, “Absent these one would consider seeking out psychological causes (stress…) that can be associated with hyperventilation.
“Useful testing in these patients include pulse oximetry, echocardiography, Holter monitor and even treadmill testing to assess exercise tolerance.”
The symptoms can be caused by panic attacks, and panic attacks aren’t always triggered by a definitive stressor.
The skipped heartbeat and apparent difficulty or problems with breathing may also have separate causes.
For instance, the issue with breathing can be caused by acid reflux, and yes, teenagers can get acid reflux.
When the acid gets as far up as the vocal cords (and the patient won’t necessarily experience heartburn), this can cause a situation called laryngopharyngeal reflux (LPR).
“Even young healthy people can develop LPR during stressful periods, eating a poor diet, even during exercise,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“Sudden or gradual voice changes, choking symptoms and shortness of breath are usually symptoms of LPR,” says Dr. Silvers.
The skipped heartbeat could be from fear stemming from the shortness of breath, from general anxiety or from a cardiac issue, even though in a teen, a skipped heartbeat and problems with breathing are more likely to have a non-cardiac origin.
Nevertheless, it’s important to see a cardiologist to see if a cardiac cause can be ruled out.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.

An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Heart Rate in 60s BUT You Also Have Heart Disease?

How is it possible for an elderly person (over age 65) to have a low resting heart rate along with severe coronary artery disease (CAD)?
Before my mother had CABG x 5, her resting heart rate was often in the high 60s, giving her the illusion that she had a healthy heart! After she had the surgery, I learned that her ejection fraction was 35 percent.
So I was thinking, here we have an elderly patient with severe heart disease plus a low ejection fraction—yet a pre-surgical resting heart rate in the high 60s.
I’d think that her conditions would have made her heart beat fast since its “squeeze” was only 35 percent, and the coronary arteries were quite narrowed.
In fact, many very out-of-shape people have slow resting heart rates, or at least pulses in the high 60s (which is very slow for them), while there are younger gym rats with resting pulses in the 80s. What’s going on here?
What a Cardiologist Says
“The heart has one main internal pacemaker that generates the electrical charge that leads to the heartbeat or heart contraction,” says cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
“As part of aging, this internal, called the sino-atrial node, can fatigue and slow down the electrical discharge.
“If the heartbeat slows to the point that one becomes dizzy or faints, an artificial pacemaker implantation is often performed to resolve this.
“In patients with coronary artery disease, a slow heartbeat can also be caused by medications that are used to treat angina or chest pain symptoms (my mother was not on any cardiac medications prior to surgery, so presumably her sino-atrial node was persistently fatigued).
“Common medicines that are used in these patients that can slow heartbeat include beta blockers (metoprolol, atenolol, carvedilol.) and some calcium channel blockers (verapamil, diltiazem).”

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik
HOW Anxiety Causes PVCs

You already know that PVCs can be caused by anxiety, but just HOW does this mechanism occur?
“PVCs, which are extra beats that occur commonly and if they occur in modest frequency are not necessarily a pathologic condition,” begins cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
“The sensation of the PVC is usually referred to as a palpitation or extra beats.
“The sensing of extra bests seems to occur both with anxiety related to both excess adrenaline release, leading to cardiac electrical excitation, and to heightened sensitivity to one’s heartbeat that occurs in an anxiety state.”
The “stress hormone” adrenaline, then, is a culprit when a person experiences a premature ventricular contraction during a stressful or fear-inducing event.
In fact, if you tend to feel the thump-THUMP of PVCs when you experience acute anxiety or some kind of fear, you’ll also notice that you have that “butterflies in the stomach” feeling — and this is the adrenaline at work:
The body’s so-called fight or flee hormone that revs up the body’s engine to prepare it for a fight or escape.
“People also have a tendency to feel these extra beats at bedtime when the environment is quiet and there are fewer distractions,” says Dr. Lepor.
Beware of the Bed

Bedtime — right after you slip into bed and are just lying there, awake and thinking — is also the time that many people begin reflecting about all the problems going on in their lives, and all the tasks they must get through come next day — and this leads to anxiety and…of course…the PVCs.
For some people, the bed is a conditioned stimulus to anxiety and edginess, as they anticipate the stresses that the next day will bring on.
These stressors include the next day being Monday, a doctor or dentist appointment, a visit from a relative, a situation with a neighbor and a new injury.
Dr. Lepor continues, “Cortisol is not directly related to PVCs, but as a stress hormone it is released in higher concentrations along with adrenaline.
“It is the adrenaline component that is more responsible for the cardiac effects of stress and the cortisol which tries to mitigate this effect.”
Engaging in strenuous exercise can help blunt cortisol production.
While moderate exercise can elevate cortisol levels temporarily, intense physical activity such as HIIT can lead to a more balanced hormonal response over time.
This effect can help you manage anxiety and also reduce the occurrences of premature ventricular contractions.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick